Abstract
Background
The two-incision approach to THA has been controversial, with some authors reporting its use is associated with a rapid recovery whereas others report no differences in outcomes and a higher risk of perioperative complications secondary to increased surgical complexity.
Questions/purposes
We therefore compared early postoperative variables including pain, length of stay, functional recovery, complications, and complexity of the mini-posterior and two-incision approaches to THA.
Patients and Methods
We prospectively enrolled 72 patients scheduled for THA and randomized them into two groups: mini-incision posterior approach and the two-incision approach. Preoperative teaching, anesthetic protocols, implants used, and rehabilitation pathways were identical for both groups. All variables were assessed at a maximum of 1 year postoperatively.
Results
All key outcomes were similar in the two groups: mean visual analog scale (VAS) scores for pain during the first 3 postoperative days and the first 6 weeks, total narcotic requirements in the hospital and during the first 6 weeks, mean length of stay (51 hours versus 48 hours), and mean Harris hip scores and SF-12 scores. Achievement of functional milestones was similar between the two groups. There was one reoperation in each group. Mean operative time was longer for patients in the two-incision group (98 minutes versus 77 minutes), however the accuracy of component positioning was similar.
Conclusions
We found no differences in perioperative outcomes between these two approaches for THA. Variables other than the surgical approach including perioperative protocols, patient expectations, and the patient’s general health may have a greater effect on outcomes such as pain during the early postoperative period, functional recovery, and length of hospital stay. The use of small incisions for THA was safe as was a shortened hospital stay in selected patients.
Level of Evidence
Level I, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The use of small incisions for THA has become popularized as an alternative to more traditional approaches to THA. Proponents of these procedures have reported less perioperative blood loss, less pain, and an accelerated recovery [2, 4–8, 19, 22]. Critics have raised concerns that the more limited exposure may negatively affect component position and increase the risk of perioperative complications [1, 15, 17, 24]. There has been particular interest in the so-called “two-incision” approach to THA, which uses an intermuscular plane for insertion of the acetabular component and a second incision for percutaneous insertion of the femoral component combined with fluoroscopic guidance to facilitate bony preparation and component insertion [2, 3, 5, 6, 8]. Although reports from some centers have associated this approach with minimal perioperative pain and a rapid recovery [2, 5, 6, 8, 19], others have reported a high rate of perioperative complications secondary to the technically demanding nature of the procedure [1, 17] and a recovery that is not different from those of modifications of more traditional approaches [18].
Along with these alternative surgical approaches have come advanced pathways for perioperative pain management, anesthetic care, and accelerated rehabilitation protocols [4, 5, 7, 21]. The introduction of changes to surgical technique and perioperative protocols in a similar time frame has made it difficult to determine whether the more rapid recovery and decreased pain that have been attributed in some centers with these less invasive approaches are secondary to the surgical approach used, patient selection, or the perioperative protocols followed.
We therefore asked whether the two-incision approach would be associated with (1) less perioperative pain, (2) shorter length of hospitalization, and (3) faster recovery as measured by the attainment of functional milestones than the mini-posterior approach. We also sought to document the incidence of complications between the two groups and relative operative complexity by determining operative time and the accuracy of component placement between the two groups.
Patients and Methods
Seventy-two patients consented to participate in this institutional review board-approved, prospective randomized trial; this study also was registered with clinicaltrials.gov (NCT00594893). All procedures were performed by one surgeon (CDV) who had participated in industry-sponsored training for the two-incision technique. Before initiating the trial, the surgeon had performed 69 THAs using the two-incision approach and approximately 400 THAs using the mini-posterior approach. Perioperative management and preoperative teaching were the same for patients in both groups. Patients were enrolled between July 2006 and September 2008.
Patients were approached for participation in the trial once indicated for unilateral THA if they had a diagnosis of osteoarthritis, a body mass index (BMI) less than 35, were between the ages of 18 and 80 years, and had no major medical comorbidities that potentially could delay their discharge from the hospital. Patients had to be willing to undergo surgery with the use of a neuraxial anesthetic and were told the expectations of the study were for them to mobilize with physical therapy on the day of the procedure and to be discharged home on the day after the surgical procedure. The criteria for discharge included the ability to get in and out of bed independently while following standard hip precautions, the ability to ambulate 150 feet using an assist device (walker, crutches, or a cane) appropriately, and the ability to navigate stairs safely if present in the home.
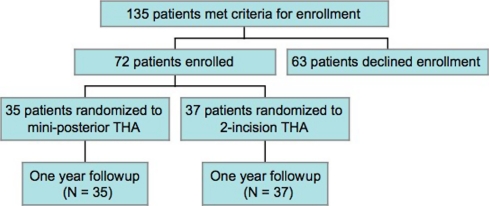
During the course of the study, the operating surgeon performed 417 primary THAs; 282 patients were not eligible for the study based on interest in an alternate bearing surface (metal-on-metal) or hip resurfacing (97 patients; 34.4%), the presence of medical issues that precluded an early discharge (95 patients; 33.7%), a diagnosis other than osteoarthritis or a history of prior hip surgery (47 patients; 16.7%), or a BMI greater than 35 (43 patients; 15.3%). Of the remaining 135 patients, 72 were enrolled in the study, 58 declined to participate, and five patients who were enrolled in the study subsequently had their contralateral hip replaced during the time that the study was still enrolling patients (Fig. 1).
Fig. 1.
A flowchart shows patient enrollment.
Thirty-five patients were randomized to the mini-posterior arm of the study and 37 to the two-incision arm. Patients were randomized using opaque, sealed, numbered envelopes after the successful induction of neuraxial anesthesia. The envelopes were created from a computer-generated randomization list. Power analysis determined a total of 70 patients (35 in each group) would be required to identify a 20% difference in VAS scores and narcotic consumption with a significance of 0.05 and 80% power. All patients were followed and assessed at 1 year postoperatively with no patients lost to followup. Patient demographics including age, gender distribution, BMI, and American Society of Anesthesiologists (ASA) class were similar between the two groups, indicating successful randomization (Table 1).
Table 1.
Patient and surgical characteristics (n = 72)
| Characteristic | Mini-posterior (n = 35) | Two-incision (n = 37) | p Value |
|---|---|---|---|
| Age (years)* | 63.8 ± 8.2 | 61.2 ± 8.0 | 0.1703 |
| BMI* | 27.3 ± 3.5 | 27.6 ± 3.3 | 0.7699 |
| Gender (number of patients) | 0.9272 | ||
| Female | 24 (69%) | 25 (68%) | |
| Male | 11 (31%) | 12 (32%) | |
| ASA score (number of patients) | 0.1019 | ||
| 1 | 1 (3%) | 4 (11%) | |
| 2 | 28 (80%) | 30 (81%) | |
| 3 | 6 (17%) | 3 (8%) |
* Values are expressed as mean ± SD; BMI = body mass index; ASA = American Society of Anesthesiologists.
A cementless acetabular component that allowed for adjunctive screw fixation was used in all cases combined with a modular, highly cross-linked polyethylene liner (Trilogy® acetabular component and Longevity® liner; Zimmer Inc, Warsaw, IN, USA). The inner diameter of the acetabular liner was 28 mm in hips in which the acetabular component outer diameter was 54 mm or less and 32 mm in hips in which the acetabular component outer diameter was 56 mm or greater. A cementless, cylindrical, diaphyseal-engaging femoral component (VerSys® Epoch Full Coat; Zimmer) was used in all cases.
The two-incision technique was performed as described by Berger [2]. The mini-posterior approach was performed with the patient in the lateral decubitus position. A straight incision of 7 to 10 cm in length was made over the posterior border of the greater trochanter and the gluteus maximus muscle was split in line with its fibers. The short external rotators were released including the piriformis; however, the quadratus femoris was preserved. The posterior capsule and short external rotators were tagged and repaired at the end of the procedure.
Patients in both groups were given 400 mg of celecoxib orally (Celebrex®; Pfizer, New York, NY, USA) on the morning of surgery. A combined spinal-epidural anesthetic was used and patients were sedated intraoperatively using 50 to 75 μg diprivan (Propofol®; AstraZeneca, Wilmington, DE, USA) per kg per hour and given 4 mg ondansetron hydrochloride (Zofran®; GlaxoSmithKline, Philadelphia, PA, USA) to prevent nausea. Sixty mL bupivacaine 0.5% with epinephrine (1:200,000) was infiltrated at the surgical site in both groups. In the recovery room, an epidural infusion was initiated for pain control. If the patient had donated autologous blood, it was transfused while the patient was in the recovery room.
All surgery on these 72 patients was performed as the first case of the day to facilitate discharge on the first postoperative day. If hemodynamically stable, patients were out of bed and ambulating with the assistance of a physical therapist on the day of surgery. The epidural catheter, Foley catheter, and Hemovac® drain were removed on the morning after surgery. Patients were given 20 mg OxyContin® (Purdue Pharma LP, Cranbury, NJ, USA) orally (10 mg for patients older than 70 years or weighing less than 120 pounds) 2 hours before removing the epidural catheter. After removal of the epidural catheter, patients were given Norco® 5/325 or 10/325 mg (Watson Pharmaceuticals, Corona, CA, USA) every 4 hours for pain as needed and continued on celecoxib 200 mg orally for the first 6 weeks postoperatively.
Patients were allowed to weightbear as tolerated on the extremity and instructed in the use of a walker or two crutches and were advised to follow THA precautions for the first 3 months postoperatively. Once discharged from the hospital, a physical therapist went to the patient’s home three times per week for the first 3 weeks postoperatively, and patients were encouraged to transition to a cane and then no assist device when the patient and the therapist judged it was safe to do so. Patients then were encouraged to attend outpatient physical therapy for an additional 6 weeks for abductor strengthening and gait training. A nurse also visited the patient at home for the first 3 weeks postoperatively to monitor their wound and anticoagulation.
Although the patient was not blinded to the procedure performed, all postoperative assessments were performed by a clinical nurse (ED) without knowledge of the surgical approach used. Patients were instructed not to share with the nurse the number of incisions used and they wore shorts during all clinical assessments. Patients were monitored for pain perioperatively using a VAS with 0 corresponding to no pain and 10 to the worst imaginable pain [22]. Pain scores using the VAS for the surgically treated hip were assessed every 8 hours for the immediate postoperative phase (while hospitalized) and then once daily at home for 6 weeks and recorded in a patient diary. The total (continuous and patient-controlled epidural analgesia [PCEA] mode) epidural medication consumption, total number of PCEA demands, and delivered boluses were recorded for each 4-hour interval postoperatively. All other opioid consumption while in the hospital and for the first 6 weeks postoperatively was recorded and subsequently converted to parenteral morphine equivalents (5 mg hydrocodone was considered equivalent to 2.5 mg parenteral morphine) for statistical comparisons.
Patients also recorded in a diary functional and other milestones, including the ability to transition to a cane from a walker or crutches, the ability to ambulate inside the home without a cane, the ability to ambulate outside the home without a cane, when oral narcotic pain medication was discontinued, and when they were able to ambulate for unlimited distances. Patients who were actively employed recorded the date of return to work. SF-12 scores [16] and Harris hip scores [9] (HHS) also were obtained for all patients preoperatively, at 3 weeks, 6 weeks, 3 months, and 1 year postoperatively.
Postoperative blood loss was assessed by measuring the amount of blood collected in the drain during the first 24 hours. Any blood product transfused during the perioperative phase also was recorded and a blood loss index (BLI) was calculated using the following formula: BLI = (preoperative hemoglobin − discharge hemoglobin) + number of units of blood transfused [11, 12]. Demographic characteristics were collected, including height, weight, BMI, age, gender, and ASA score.
One of us (SMS) evaluated the 6-week postoperative radiographs (AP pelvis, AP and lateral hip) to determine the abduction angle of the acetabular component [13] and alignment of the femoral component. Radiographic review was performed independently without knowledge of the surgical technique. Acetabular components were considered malpositioned if they had an abduction angle less than 35° or greater than 55° and femoral components were judged malpositioned if they were greater than 3° from neutral alignment.
Pain, as quantified using VAS and opioid consumption, was modeled across times using repeated-measures regression with an autoregressive covariance structure for the time-based data. Difference in length of hospitalization was evaluated using Student’s t-test, after validating assumptions of normality and homoscedasticity. Physical therapy attendance on the day of surgery and discharges on Day 1 were tested using a traditional chi square test and corroborated with Fisher’s Exact test. Functional outcomes (SF-12, HHS) were modeled using a repeated-measures regression with an autoregressive covariance structure for the time-based data. For each of the recovery measures we also evaluated a within-subject test of the main effect of the time factor, to test for improvements with time. For all repeated measures models, time-based interactions were evaluated before main effects to identify possible confounds. Differences in preoperative demographics, including normally distributed univariate data (age and BMI) were analyzed using Student’s t tests whereas categorical data were analyzed using the chi square test for dichotomous data and Mantel-Haenszel test for ordered categorical data (ASA status). The Bonferroni step-down method was used to control for multiple-comparison error inflation. The CONSORT guidelines were used for preparation of the manuscript.
Results
Mean VAS scores and amounts of narcotics consumed while in the hospital were not different between the two groups with the given sample size (Table 2). Similarly, the mean VAS scores and amounts of narcotics consumed during the first 6 weeks were similar between the two groups.
Table 2.
Pain scores (VAS), analgesics, and health-related quality of life measures
| Parameter | Mini-posterior (n = 35) | Two-incision (n = 37) | p Value |
|---|---|---|---|
| During hospital stay | |||
| VAS pain average | 1.8 ± 1.3 | 1.7 ± 1.3 | 0.8205 |
| Epidural infusion (mL) | 117 ± 38 | 113 ± 25 | 0.6284 |
| Morphine equivalent (mL) | 26 ± 17 | 26 ± 17 | 0.9073 |
| Hydrocodone | 0.7864 | ||
| Week 1 | 14.2 ± 15.3 | 15.9 ± 16.7 | |
| Week 3 | 3.2 ± 6.9 | 4.4 ± 8.9 | |
| Week 6 | 1.3 ± 4.4 | 1.4 ± 4.0 | |
| Pain (VAS) | 0.2795 | ||
| Week 1 | 1.7 ± 2.4 | 2.4 ± 1.8 | |
| Week 3 | 0.5 ± 0.5 | 1.5 ± 2.0 | |
| Week 6 | 0.3 ± 0.4 | 0.8 ± 0.3 | |
| SF-12 | |||
| PCS | 0.5914 | ||
| Preoperative | 31 ± 8 | 30 ± 6 | |
| 3-week followup | 36 ± 8 | 33 ± 8 | |
| 6-week followup | 39 ± 9 | 39 ± 9 | |
| 3-month followup | 46 ± 9 | 45 ± 10 | |
| 1-year followup | 48 ± 10 | 47 ± 10 | |
| MCS | 0.1942 | ||
| Preoperative | 58 ± 7 | 54 ± 11 | |
| 3-week followup | 57 ± 7 | 54 ± 11 | |
| 6-week followup | 60 ± 5 | 54 ± 10 | |
| 3-month followup | 57 ± 5 | 57 ± 8 | |
| 1-year followup | 58 ± 6 | 55 ± 8 | |
| Harris hip score | 0.3298 | ||
| Preoperative | 50 ± 12 | 52 ± 10 | |
| 3-week followup | 68 ± 11 | 62 ± 14 | |
| 6-week followup | 77 ± 14 | 75 ± 11 | |
| 3-month followup | 85 ± 11 | 85 ± 11 | |
| 1-year followup | 91 ± 5 | 89 ± 8 | |
The values are given as mean ± standard deviation or count with percent in parentheses; preoperative values were added in as covariates to compensate for preoperative differences; PCS = physical component score; MCS = mental component score.
The mean length of stay, the percentage of patients discharged on the first postoperative day, and the ability to participate in physical therapy on the day of surgery were similar between the two groups (Table 3). Intraoperative blood loss, transfusion requirements, and BLI were similar although drainage from the Hemovac® was greater in the two-incision group.
Table 3.
Perioperative outcomes
| Parameter | Mini-posterior | Two-incision | p Value |
|---|---|---|---|
| (n = 35) | (n = 37) | ||
| Operative outcome | |||
| Operative time (minutes) | 77 ± 15 | 98 ± 25 | 0.0008 |
| Fluoroscopic time (seconds) | NA | 37 ± 10 | |
| Estimated blood loss | 391 ± 231 | 437 ± 191 | 0.3621 |
| Blood loss index | 3.7 ± 1.4 | 3.8 ± 1.3 | 0.7269 |
| Length of stay (hours) | 51 ± 25 | 47 ± 20 | 0.4082 |
| Hemovac drainage (mL) | 207 ± 160 | 401 ± 243 | 0.0002 |
| Transfusions | 0.9278 | ||
| 0 | 27 (77%) | 26 (70%) | |
| 1 | 7 (20%) | 11 (30%) | |
| 2 | 1 (3%) | 0 (0%) | |
| Physical therapy on Day 1 | 0.7892 | ||
| Yes | 31 (89%) | 32 (86%) | |
| No | 4 (11%) | 5 (14%) | |
| Discharge on Day 1 | 0.4868 | ||
| Yes | 17 (49%) | 21 (57%) | |
| No | 18 (51%) | 16 (43%) | |
The values are given as mean ± standard deviation or count with percent in parentheses.
The mean HHS and SF-12 scores obtained at 3 weeks, 6 weeks, 3 months, and 1 year were not different between the two groups (Table 2). The achievement of functional milestones during the first 6 weeks was similar between the two groups (Table 4), with the exception of the patients in the two-incision group reporting a trend toward a faster return to work although we had only a small sample: only 12 patients in each arm of the study were employed before THA.
Table 4.
Milestones
| Milestone (days postoperatively) | Mini-posterior (n = 35) | Two-incision (n = 37) | p Value |
|---|---|---|---|
| Transitioned from walker to cane | 13.3 ± 10.4 | 12.7 ± 10.0 | 0.8070 |
| Walk inside home without a cane | 19.7 ± 12.0 | 19.7 ± 11.8 | 0.9891 |
| Walk outside home without a cane | 28.5 ± 16.6 | 28.6 ± 17.4 | 0.9893 |
| Stopped analgesics | 19.3 ± 13.7 | 19.1 ± 14.0 | 0.9679 |
| Walk unlimited distance | 34.8 ± 17.4 | 34.6 ± 16.9 | 0.9749 |
| Return to work (n = 24, 12 in each group) | 42.3 ± 26.9 | 26.0 ± 13.6 | 0.0791 |
Values are expressed as mean ± SD.
There were two reoperations, one in each arm of the study. One patient in the mini-posterior arm of the study had revision surgery for recurrent instability and one patient in the two-incision arm of the study underwent open treatment of a periprosthetic fracture of the femur that was not recognized on the fluoroscopic images but was seen on the immediate postoperative radiographs. There was one readmission to an outside hospital by a patient in the two-incision arm of the study for lower extremity swelling on postoperative Day 12; no evidence of thromboembolic disease was found and she was discharged to home.
There was no difference in acetabular or femoral component positioning between the two groups. There were four acetabular components outside the acceptable range in the mini-posterior group (two greater than 55°, two less than 35°) and two components outside the acceptable range in the two-incision group (both less than 35°) (p = 0.355). None of the femoral components were greater than 3° from neutral in either group. The mean operative time was longer (p < 0.001) for patients who had the two-incision as opposed to the mini-posterior procedure (77 versus 98 minutes).
Discussion
The two-incision approach to THA has been controversial. Some authors have reported it is associated with a rapid recovery although others report no differences in recovery but a higher risk of perioperative complications, likely secondary to increased surgical complexity. To address this controversy we compared early postoperative variables including pain, length of stay, functional recovery, complications, and complexity of the mini-posterior and two-incision approaches with those of THA.
We recognize several limitations to our study. First, we examined a relatively small sample size. The study was powered to detect a 20% difference in narcotic requirements and VAS scores, which we believed to be a clinically relevant difference. Given the study was not powered on other variables, the risk of a Type II error is not unexpected. Second, although the outcome data were collected by an observer not involved with the surgical procedures and blinded to which had been performed, the patients were not blinded to which procedure they had undergone, as in one study [14], and the patients’ knowledge of the surgical approach may have introduced bias based on their perceptions of the surgical approach used. Third, the procedures were performed on a selected group of patients, and these results may not be generalizable to a more typical population of patients undergoing THA.
We found no difference in early perioperative pain scores between the two patient groups. Pagnano et al. [18] performed a similar prospective randomized study (Table 5) comparing the two-incision and mini-posterior approaches with THA; however, perioperative pain scores and narcotic consumption were not measured. Although it is still controversial whether an abbreviated surgical approach is associated with a faster recovery, less pain, or improved outcomes [7, 10, 15, 21, 22, 24], our results suggest, similar to the study of Pour et al. [21], that perioperative protocols, patient selection, and preoperative education may have a greater effect on early outcomes than the surgical approach.
Table 5.
Comparison of results of similar published studies and current study
| Study | Subjects | Type of trial | Operative time | Pain | Length of hospital stay | Recovery | Complications |
|---|---|---|---|---|---|---|---|
| Pagnano et al. [18] | 72 | Prospective randomized | Two-incision longer | Not measured | Not measured | Two-incision slower | No difference |
| Duwelius et al. [8] | 86 | Retrospective | Two-incision longer | Not measured | Faster | Two-incision faster | No difference |
| Current study | 72 | Prospective randomized | Two-incision longer | No difference | No difference | No difference | No difference |
The length of hospitalization was not different between the two groups of patients in our trial. In contradistinction, Duwelius et al. [8], in a retrospective matched analysis of 86 patients (43 in each group) comparing the mini-posterior and two-incision approaches, found the latter approach was associated with a shorter length of stay (Table 5), although they recognized the retrospective nature of their study may have biased their results by the use of different selection criteria for the two procedures.
We found no differences in functional outcomes or recovery in this trial. Pagnano et al. [18], reporting results for 72 patients, found those who had undergone the two-incision procedure had a slower recovery, as measured by the attainment of functional milestones. With a similar sample size, we found similarly rapid recovery, with no detectable differences between them, other than a trend toward a faster return to work for the patients who had the two-incision procedure (Table 4). The reasons for this difference in outcomes despite a similar study design are unclear but could reflect merely sampling error or differing populations.
Although several reports have raised concern regarding a high risk of complications with the two-incision approach [1, 17] and the mini-incision approach [24], in our small series we found both techniques were associated with an acceptable rate of complications, which is in agreement with other studies [5, 7, 8, 10, 14, 15, 19, 23]. Pagnano et al. [18] also reported a low risk of complications with both approaches as did Duwelius et al. [8]. We also observed no complications directly related to the shortened length of hospitalization, indicating a shortened hospital stay is safe for carefully selected patients. Although Parvizi et al. [20] suggest an abbreviated hospital stay may place patients at greater risk for serious complications, we observed no such difference; only one patient was admitted to another facility for reasons which did not appear to be directly related to the surgery.
The two-incision technique generally is believed to be a more technically demanding procedure than the mini-posterior procedure and the increased operative time observed is not unexpected and is in agreement with other studies [8, 18]. However, the accuracy of component placement was equivalent in the two groups of patients despite the increased complexity and decreased observation associated with the two-incision approach. Based on our increased operative time and no differences in the studied variables, we no longer perform the two-incision approach for THA.
Footnotes
This study was supported by a grant from Zimmer Inc (Warsaw, IN). Dr. Della Valle has performed consulting services for Zimmer within the past year and presently is a consultant for Smith and Nephew Inc (Memphis, TN), Biomet Inc (Warsaw, IN), and Kinamed Inc (Camarillo, CA). Dr. Sporer is a consultant for Zimmer.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique: surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1 pt 2):221–233. doi: 10.2106/JBJS.F.00326. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res. 2003;417:232–241. doi: 10.1097/01.blo.0000096828.67494.95. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA. The technique of minimally invasive total hip arthroplasty using the two-incision approach. Instr Course Lect. 2004;53:149–155. [PubMed] [Google Scholar]
- 4.Berger RA. A comprehensive approach to outpatient total hip arthroplasty. Am J Orthop (Belle Mead NJ) 2007;36(9 suppl):4–5. [PubMed] [Google Scholar]
- 5.Berger RA, Duwelius PJ. The two-incision minimally invasive total hip arthroplasty: technique and results. Orthop Clin North Am. 2004;35:163–172. doi: 10.1016/S0030-5898(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 7.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty: a prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 8.Duwelius PJ, Burkhart RL, Hayhurst JO, Moller H, Butler JB. Comparison of the 2-incision and mini-incision posterior total hip arthroplasty technique: a retrospective match-pair controlled study. J Arthroplasty. 2007;22:48–56. doi: 10.1016/j.arth.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 10.Howell JR, Masri BA, Duncan CP. Minimally invasive versus standard incision anterolateral hip replacement: a comparative study. Orthop Clin North Am. 2004;35:153–162. doi: 10.1016/S0030-5898(03)00137-8. [DOI] [PubMed] [Google Scholar]
- 11.Landefeld CS, Cook EF, Flatley M, Weisberg M, Goldman L. Identification and preliminary validation of predictors of major bleeding in hospitalized patients starting anticoagulant therapy. Am J Med. 1987;82:703–713. doi: 10.1016/0002-9343(87)90004-0. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Berend KR, Mallory TH, Dodds KL, Adams JB. Soft tissue and intra-articular injection of bupivacaine, epinephrine, and morphine has a beneficial effect after total knee arthroplasty. Clin Orthop Relat Res. 2004;428:125–130. doi: 10.1097/01.blo.0000147701.24029.cc. [DOI] [PubMed] [Google Scholar]
- 13.Martell JM, Pierson RH, III, Jacobs JJ, Rosenberg AG, Maley M, Galante JO. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg Am. 1993;75:554–571. doi: 10.2106/00004623-199304000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Meneghini RM, Smits SA, Swinford RR, Bahamonde RE. A randomized, prospective study of 3 minimally invasive surgical approaches in total hip arthroplasty: comprehensive gait analysis. J Arthroplasty. 2008;23(6 suppl 1):68–73. doi: 10.1016/j.arth.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 16.Ostendorf M, Stel HF, Buskens E, Schrijvers AJ, Marting LN, Verbout AJ, Dhert WJ. Patient-reported outcome in total hip replacement: a comparison of five instruments of health status. J Bone Joint Surg Br. 2004;86:801–808. doi: 10.1302/0301-620X.86B6.14950. [DOI] [PubMed] [Google Scholar]
- 17.Pagnano MW, Leone J, Lewallen DG, Hanssen AD. Two-incision THA had modest outcomes and some substantial complications. Clin Orthop Relat Res. 2005;441:86–90. doi: 10.1097/01.blo.0000191275.80527.d6. [DOI] [PubMed] [Google Scholar]
- 18.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:1000–1006. doi: 10.2106/JBJS.G.00804. [DOI] [PubMed] [Google Scholar]
- 19.Palutsis RS, Sheridan KC, Wasielewski RC. One surgeon’s experience with the 2-incision technique for total hip arthroplasty. J Arthroplasty. 2010;25:71–75. doi: 10.1016/j.arth.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 20.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 21.Pour AE, Parvizi J, Sharkey PF, Hozack WJ, Rothman RH. Minimally invasive hip arthroplasty: what role does patient preconditioning play? J Bone Joint Surg Am. 2007;89:1920–1927. doi: 10.2106/JBJS.F.01153. [DOI] [PubMed] [Google Scholar]
- 22.Sriwatanakul K, Kelvie W, Lasagna L, Carimlin JF, Weis OF, Mehta G. Studies with different types of visual analog scales for measurement of pain. Clin Pharmacol Ther. 1983;34:234–239. doi: 10.1038/clpt.1983.159. [DOI] [PubMed] [Google Scholar]
- 23.Wenz JF, Gurkan I, Jibodh SR. Mini-incision total hip arthroplasty: a comparative assessment of perioperative outcomes. Orthopedics. 2002;25:1031–1043. doi: 10.3928/0147-7447-20021001-14. [DOI] [PubMed] [Google Scholar]
- 24.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86:1353–1358. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]