FK 506, a macrolide antibiotic, is a powerful immunosuppressant which is approximately 100 times more potent than cyclosporine (CyA). The first clinical experience with this agent was attained in patients with refractory hepatic rejection and complications of CyA therapy.1,2 Initial experience suggested that FK 506 was surprisingly effective in reversing rejection in these patients. In the first patients, the combined nephrotoxicity of FK 506 and CyA was apparent. Serum creatinine (SCr) regularly increased and, at times, dramatically.3 This was termed the “crossover nephrotoxicity” of FK 506 and CyA. FK 506 has now been used for approximately 2 years at the University of Pittsburgh. We will update our experience with the changes in renal function after conversion from CyA to FK 506.
Patients and Methods
The first 121 patients converted from CyA to FK 506 will be described. The reasons for conversion included: (a) refractory hepatic rejection (90 patients); (b) complications of CyA therapy (25 patients); (c) those in which a reduction in steroid dosage was desirable (6 patients). Initially, all patients received IV FK 506, 0.075 mg/kg per day for several days, and 0.15 mg/kg per day subsequently. CyA was retained for the first day in some patients, but our policy later was to discontinue it the day FK 506 was started. Patients without hepatic rejection were usually converted with oral FK 506 0.1 to 0.15 mg/kg per day. Patients with renal failure prior to conversion received the lower dose. Renal function was determined by daily BUN, creatinine, and electrolytes. Glomerular filtration rate (GFR) and ERPF were determined by iothalamate and hippuran clearance in some patients.
Results
All patients experienced a rise in SCr at some time. Surprisingly, 25 patients (21%) experienced a fall in SCr during the first week. An increase in SCr of <0.9 mg/dL occurred in 60 patients, <1.8 mg/dL in 21, and the remainder experienced a rise in SCr >2.0 mg/dL during the first week. Fig 1 illustrates the change in SCr for all patients over time. Peak SCr occurred usually during the first 2 months, and decreased as FK 506 dosage was reduced. Patients rescued for acute hepatic rejection experienced the greatest rise in SCr and required higher FK 506 drug doses and levels. Interestingly, patients converted for renal insufficiency (Fig 2) noted an overall reduction in SCr at latest follow-up compared to pretreatment values (2.8 ± 1.8 vs 1.8 ± 0.8 mg/dL). This probably reflects aggressive attempts to reduce FK 506 doses and preserve renal function.
Fig 1.
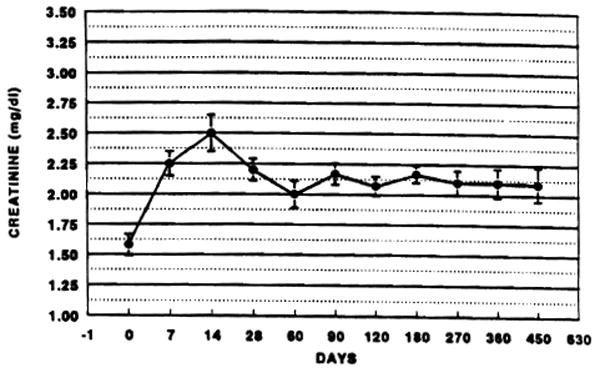
Change in creatinine for all rescue patients.
Fig 2.
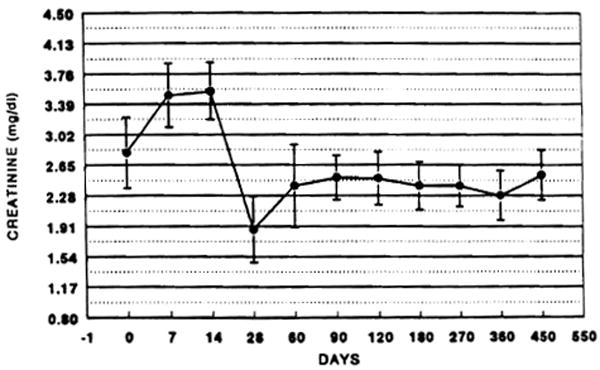
Changes in creatinine for patients converted for renal insufficiency.
In all patients tested, ERPF and GFR fell in parallel after starting FK 506. As FK 506 was tapered and drug levels fell, ERPF and GFR returned toward pretreatment values.
Patients converted for hypertension, steroid intolerance, and chronic rejection had intermediate changes in SCr. Pretreatment and latest follow-up SCr were: 1.7 ± 0.7 vs 1.8 ± 1.2 mg/dL for hypertension, 1.3 ± 0.6 vs 1.8 ± 0.4 mg/dL for steroid intolerance, and 1.4 ± 0.7 vs 1.9 ± 0.5 mg/dL, respectively.
Discussion
The changes in renal function after conversion appear to be related primarily to the requirement for FK 506. Patients experiencing acute hepatic rejection required the maximal doses to rescue the liver and, therefore, developed the greatest reduction in renal function. Since these original cases, the initial doses of FK 506 have decreased progressively. No longer are large IV infusions performed, and the current policy is to progressively taper FK 506 doses to the minimal dose needed to prevent rejection. These patients, however, demonstrated that the benefits of conversion from CyA to FK 506 could be accomplished without permanently reducing renal function, if the doses of FK 506 were lowered in a deliberate and progressive manner.
References
- 1.Starzl TE, Abu-Elmagd, Tzakis A, et al. Transplant Proc. 1991;23:914. [PubMed] [Google Scholar]
- 2.Fung J, Todo S, Jain A, et al. Transplant Proc. 1990;22:6. [PMC free article] [PubMed] [Google Scholar]
- 3.McCauley J, Fung J, Jain A, et al. Transplant Proc. 1990;22:17. [PMC free article] [PubMed] [Google Scholar]


