SUMMARY
Liver transplantation is now the preferred treatment for many diseases leading to end-stage liver disease. Transplantation for cancer has been disappointing and there is a significant recurrence rate after transplantation in hepatitis B-virus carriers. Additional strategies will have to be developed if we are to improve the results of transplantation for these patients. The role of immunological factors in liver transplantation continues to reveal significant differences from their role in renal transplantation and will continue to be an interesting area of study for years to come.
The liver transplant program at the University of Colorado began using CsA in 1980 and it soon became apparent that the most effective way to use the drug was in combination with low-dose steroids (1). The Starzl program transferred in 1981 to the University of Pittsburgh where it, along with programs in kidney and heart transplantation, has flourished (Fig. 1). In 1984, use of monoclonal murine antihuman lymphocyte antibody (Orthoclone OKT3[R]) was begun in trials in Pittsburgh for treatment of steroid-resistant rejection and immediately proved to be a highly effective agent (2,3).
Figure 1.
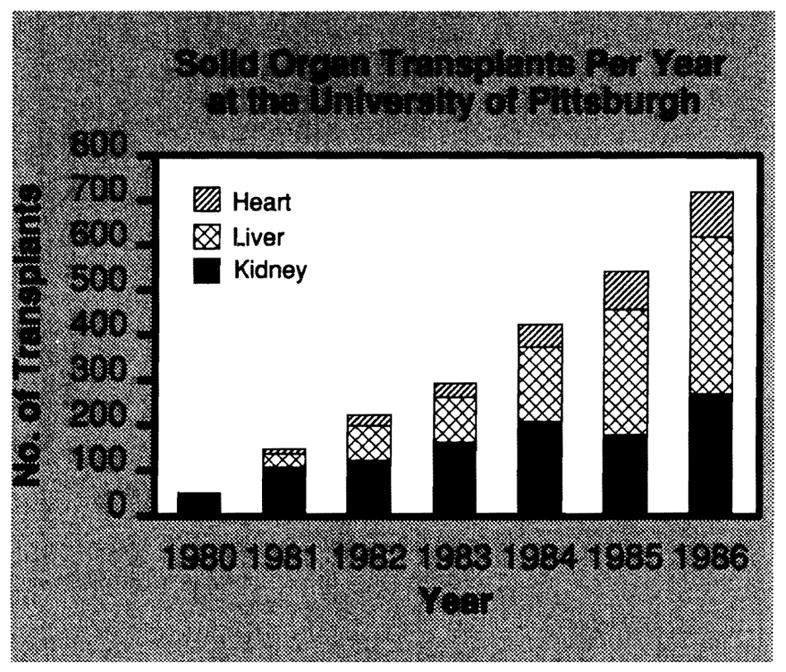
Transplants per year at the University of Pittsburgh. The liver transplant program has become the most active clinical transplant program at the medical center but there has also been substantial growth in the kidney and heart transplant programs.
On July 20, 1987, the 1,000th primary human liver transplant in the Denver-Pittsburgh CsA series was performed. The results of this experience were recently presented by Iwatsuki at the International Transplant Forum held in Pittsburgh to honor 25 years of contributions to this field by Thomas E. Starzl. The full proceedings of the forum will be published in Transplantation Proceedings. Highlights of this 1,000-case experience are presented here.
SURVIVAL AFTER LIVER TRANSPLANTATION
Most of the morbidity and mortality after liver transplantation occurs within the first year after transplantation. Routine use of CsA has had a dramatic impact on survival during this critical period. One-year survival after liver transplantation has improved from 32.4% with azathioprine and high-dose steroids to 70.5% with CsA and low-dose steroids (Fig. 2).
Figure 2.
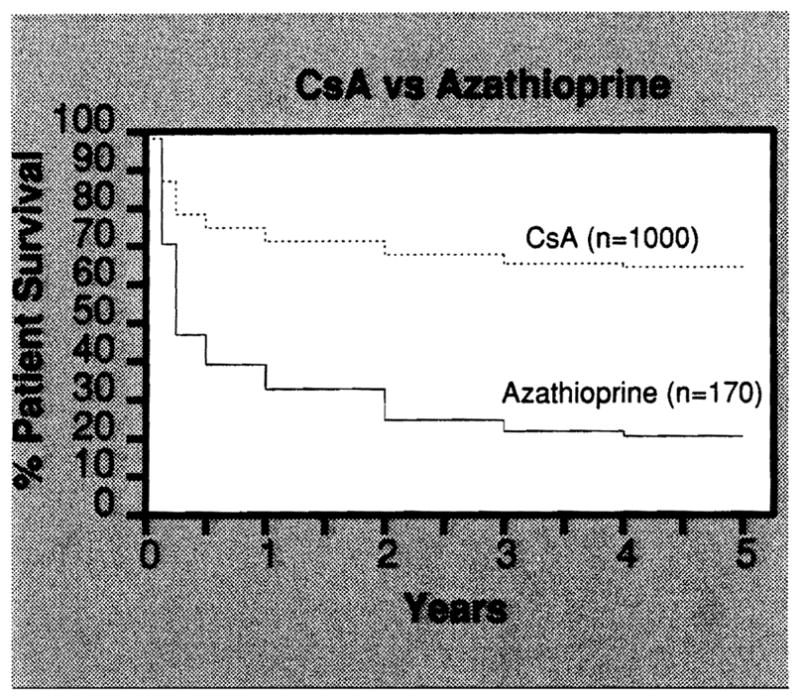
Survival rates for 170 patients transplanted with azathioprine - high-dose steroids between March 1963 and February 1980 and for 1,000 patients transplanted with CsA-low-dose prednisone between March 1980 and July 1987. Follow-up is complete through August 1987.
Equally impressive has been the durability of liver grafts beyond the first year after transplantation. Only 55 of the original 170 patients transplanted in Denver using azathioprine and high-dose steroids survived at least one year, but 28 of these 55 remain alive and well, including 20 patients more than 10 years after transplantation. Even more remarkable is the fact that of 498 patients transplanted with CsA-prednisone who survived at least one year, only 33 have subsequently been lost.
Biliary atresia, inborn errors of metabolism, and postnecrotic or cryptogenic cirrhosis have been the most common indications for transplantation in children (Table 1). In adults, the most frequent indications for liver transplantation are postnecrotic cirrhosis, primary biliary cirrhosis, and sclerosing cholangitis (Table 1). Survival rates for these indications are similar and are summarized in Figures 3 and 4.
Table 1.
Major indications for liver transplantation.
| Indication | Pediatric | Adult | Total |
|---|---|---|---|
| Cirrhosis | 40 (12.0%) | 282 (42.3%) | 322 (32.2%) |
| Biliary Atresia | 178 (53.3%) | 1 (0.2%) | 179 (17.9%) |
| Primary biliary cirrhosis | 0 | 161 (24.2%) | 161 (16.1%) |
| Inborn errors | 63 (18.9%) | 35 (5.3%) | 98 (9.8%) |
| Sclerosing cholangitis | 1 (0.3%) | 81 (12.2%) | 82 (8.2%) |
| Primary liver tumors | 4 (1.2%) | 38 (5.7%) | 42 (4.2%) |
| Fulminant hepatic failure | 13 (3.9%) | 27 (4.1%) | 40 (4.0%) |
| Secondary biliary cirrhosis | 7 (2.1%) | 13 (2.0%) | 20 (2.0%) |
| Familial cholestasis | 15 (4.5%) | 0 | 15 (1.5%) |
| Budd-Chiari syndrome | 2 (0.6%) | 13 (2.0%) | 15 (1.5%) |
| Congenital hepatic fibrosis | 7 (2.1%) | 1 (0.2%) | 8 (0.8%) |
Figure 3.
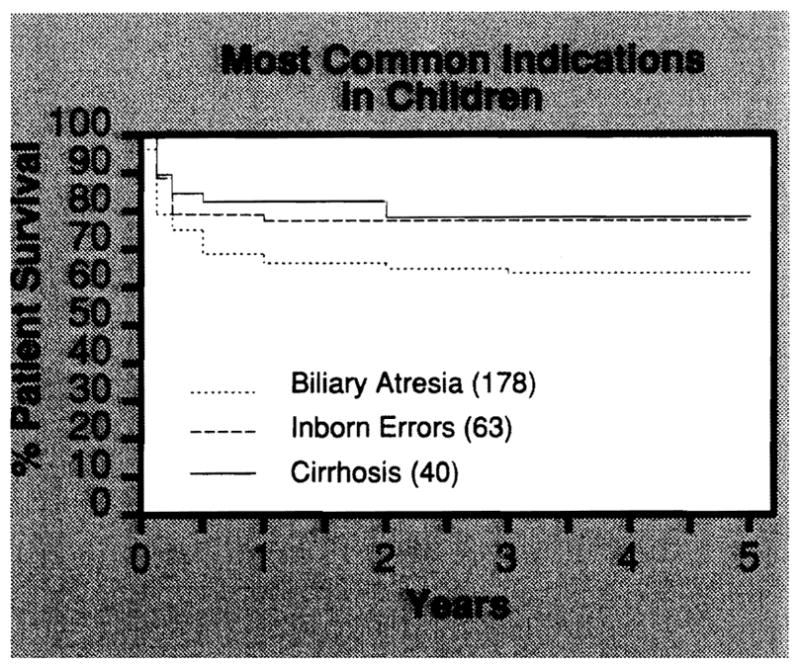
Actuarial survival rates for the 3 most common indications for transplantation in children. Cirrhosis includes postnecrotic hepatitis and cryptogenic cirrhosis.
Figure 4.
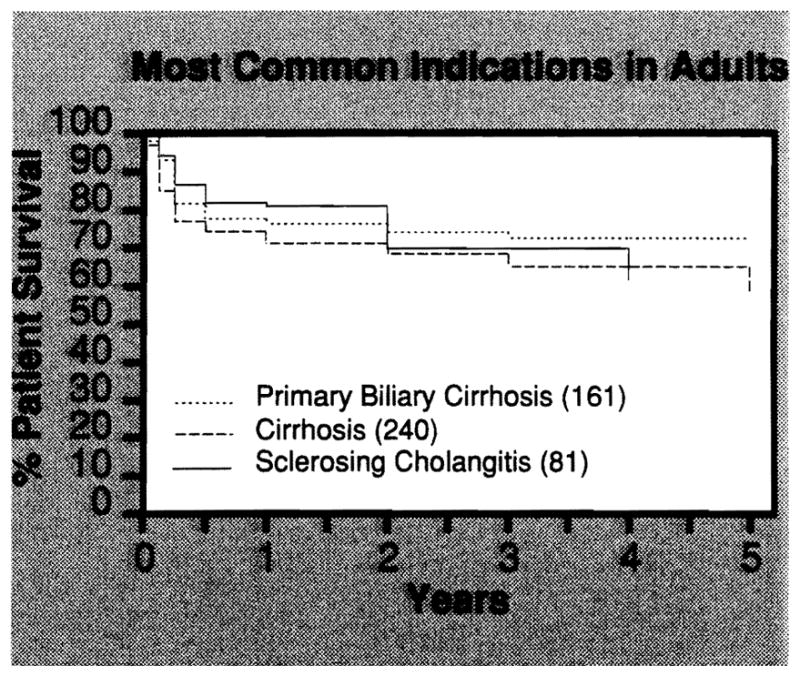
Actuarial survival rates for the 3 most common indications for liver transplantation in adults. Cirrhosis includes postnecrotic cirrhosis and cryptogenic cirrhosis but not Laennec’s cirrhosis
Recurrence of Disease
Liver cancer
Transplantation for most forms of primary liver cancer has proven disappointing (4). For all but a few types of liver cancer, recurrence of cancer has been common within one year after transplantation. Patients with epithelioid hemangioendothelioma have generally done well as have patients with small incidental hepatocellular cancers discovered at transplantation for other liver disorders such as postnecrotic cirrhosis or tyrosinemia. Patients with the fibrolamellar variant of hepatocellular cancer have tended to have the longest palliation after transplantation, sometimes lasting several years. However, most patients with hepatocellular cancer too extensive for conventional resection and patients with bile duct cancers have benefited little if any from transplantation.
Of the 83 patients transplanted for sclerosing cholangitis, 75 had no evidence of bile duct cancer complicating their disease and 57 of these patients survive. One-year actuarial survival for patients with benign disease is 80.2%. Eight patients were transplanted and found to have malignant bile duct lesions in the resected liver. Only 3 patients have survived and one-year actuarial survival for patients with malignant disease is only 33.3% (p<0.02).
Our experience with tumors metastatic to the liver is limited to 7 cases including 2 pancreatic glucagonomas (pancreatic origin), 2 intestinal carcinoids, a pancreatic gastrinoma, a small bowel, leiomyosarcoma, and one adenocarcinoma of unknown origin. One patient with a carcinoid died at 3 months free of tumor and the second patient died with tumor at 6 months after transplantation. The 2 patients with metastatic glucagonomas are alive and presumably free of tumor in the liver at 10 and 13 months. One of these patients is suspected of still having a primary lesion in the pancreas. The patient with metastatic small bowel leiomyosarcoma is alive and tumor free at 15 months after transplantation. The patient with metastatic adenocarcinoma died with tumor 21 months after transplantation.
Postnecrotic cirrhosis
Many patients with postnecrotic cirrhosis have benefited from transplantation and the survival rate for these patients is 70% at one year and 63.2% at 5 years. However, there is a high risk of recurrent infection in B-virus carriers (HBsAg positive). The one-year survival rate for B-virus carriers with chronic aggressive hepatitis is 47.8% compared with 77.0% for noncarriers (p<0.01) (Fig. 5). In contrast 6 of 7 patients transplanted for acute fulminant B-virus-induced hepatic necrosis are surviving 18 months to more than 2 years after transplantation.
Figure 5.
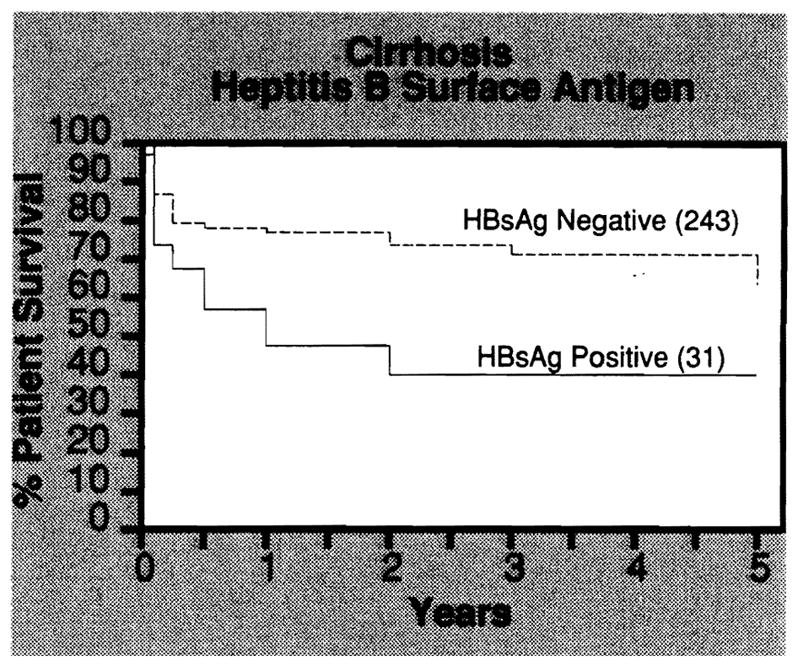
Actuarial survival rates for patients transplanted with cirrhosis classified according to hepatitis B surface antigen (HBsAg) status. A high incidence of recurrent hepatitis B after transplantation in HBsAg-positive patients resulted in significantly lower survival of these patients (p<0.01).
Primary biliary cirrhosis
Primary biliary cirrhosis is a disease of unknown etiology characterized by jaundice, fatigue, prurititis, osteoporosis (hepatic rickets), and progresses slowly to liver failure. It most commonly afflicts middle-aged and older women. Although the disease is uncommon, it is one of the most common indications for liver replacement in adults. Of the 161 patients transplanted for primary biliary cirrhosis, 122 are surviving including 85 patients now beyond one year after transplantation. Only 2 patients have died more than a year after transplantation and so far there are no confirmed cases of recurrent primary biliary cirrhosis in the transplanted liver.
Laennec’s cirrhosis
Alcoholic cirrhosis has been a controversial indication for liver transplantation since the disease is self induced and the risk of recidivism has been thought to be high. Furthermore, many patients with advanced alcoholic liver disease have systemic manifestations of alcoholism such as neurological degeneration that are irreversible and contraindicate transplantation. However, there is no effective alternative therapy available for patients with end-stage alcoholic liver disease and provided the patient is an acceptable operative risk and free of irreversible complications, transplantation may be worthwhile.
Forty-one of the 1,000 patients transplanted in this series suffered from alcohol-induced liver disease. Twenty-eight are surviving 30 days to one year after transplantation. Although our experience to date has been encouraging, longer follow-up will be needed to determine the effectiveness of liver transplantation and the incidence of recidivism in these patients. Perioperative mortality is less than 10% and therefore these patients have not been a prohibitive surgical risk.
Transplantation in Older Patients
In the past several years, significant numbers of patients over age 60 have been referred for transplantation, most often with primary biliary cirrhosis or postnecrotic cirrhosis. Forty-eight patients over 60 have been transplanted with 29 surviving. One-year actuarial survival for patients over 60 is 55.7%. The 2 oldest patients, a 67-year-old man and a 76-year-old woman, both with primary biliary cirrhosis, are well and fully rehabilitated 24 and 13 months after transplantation, respectively.
One of the most troublesome complications in older patients surviving more than 6 months after transplantation has been debilitating osteoporosis. Many of these patients suffer from “hepatic rickets” and osteoporosis is further aggravated by the steroid immunosuppression. It is advantageous in these patients to use as little steroid as possible. Fortunately, rejection is often easier to control in older patients and it is frequently possible to use minimal doses of prednisone.
IMMUNOLOGICAL FACTORS INFLUENCING GRAFT SURVIVAL
Until recently lack of sufficient case numbers made it difficult to assess the importance of immunological factors, such as ABO blood group differences, preformed anti-HLA cytotoxic antibody, or HLA matching on graft outcome, in liver transplantation. However, with the increased experience of the last several years it is now possible to study these factors.
ABO Blood Groups
The ABO blood groups cannot be breached in renal transplantation without high risk of hyperacute graft rejection. It has been known for many years that transplantation of the liver across ABO blood groups does not produce hyperacute rejection(5). However, we have found that there is a small but significant penalty for transplanting the liver across ABO blood groups. Graft survival between ABO-identical donor-recipient pairs is significantly higher than survival of grafts between ABO-compatible but nonidentical or ABO-incompatible donor-recipient pairs (Fig. 6) (6,7). Even when the data are adjusted to remove patients transplanted under high risk, urgent conditions, the difference is still observed (7).
Figure 6.
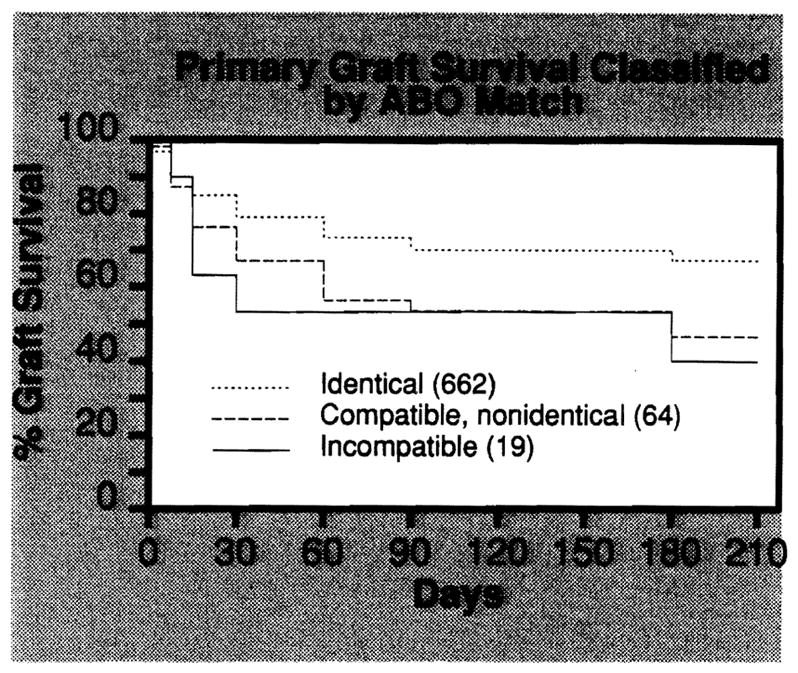
Actuarial survival of primary liver grafts based on donor-recipient ABO compatibility. Grafts between ABO-identical donor-recipient pairs fare better than grafts between ABO-mismatched or incompatible pairs. Adapted from Gordon et al., Transplant Proc, in press
At the present time, we recommend that ABO-mis-matched or incompatible grafts only be used when transplantation is urgent or donor availability is severely limited, such as for small children.
Preformed lymphocytotoxic antibody
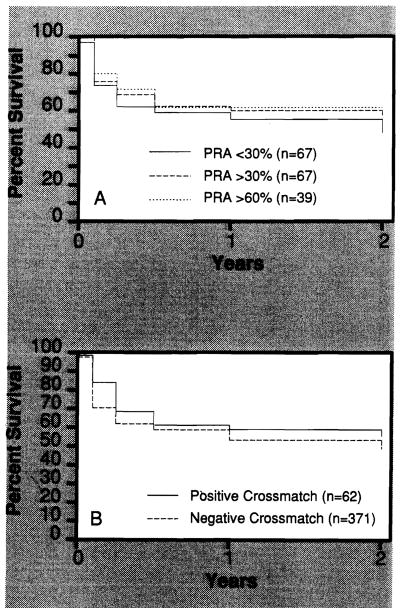
High levels of panel reactive antibody (PRA) have been associated with increased rates of graft rejection in kidney transplantation (8). However, we have not demonstrated a similar relationship of PRA to graft survival in liver transplantation (Fig. 7A).
Figure 7.
Figure 7A. Actuarial survival of primary liver grafts based on recipient panel-reactive antibody (PRA). 7B. Actuarial survival of primary liver grafts based on the donor-specific cytotoxic antibody crossmatch. Adapted from Gordon, et al, Surgery 100:705–715, 1986.
A donor-specific lymphocytotoxic antibody crossmatch is routinely performed prior to kidney transplantation and a positive crossmatch is usually prohibitive (9,10). Sequential liver-kidney transplants have been performed in patients with a strongly positive donor-specific antibody crossmatch. When the liver is transplanted first in such cases, it is capable of clearing enough circulating preformed antibody to protect a kidney immediately transplanted from the same donor (11).
There is usually insufficient time to crossmatch liver recipients prior to transplantation but we have routinely collected sera and crossmatched the patients retrospectively. A statistical comparison of liver graft survival demonstrates no significant difference for transplantation between donor-recipient pairs with a positive or negative antidonor lymphocyte antibody crossmatch (Fig. 7B) (12). It is likely that hyperacute rejection of the liver does in fact occur in certain uncommon and still poorly defined circumstances but it cannot be reliably predicted by the conventional antibody crossmatch. Additional studies are under way to determine if there are selected specificities and target cells which can predict antibody-mediated rejection of the liver.
HLA matching
Liver transplantation is performed without regard to HLA matching and therefore analysis of the effect of HLA antigens can only be done retrospectively. In any single series the number of high grade matches is relatively small. Nevertheless, some interesting trends are suggested in our first analysis of this series.
Grafts transplanted with no mismatch at the A locus have not done as well (p<0.03) as grafts transplanted with a one or 2 HLA-A mismatches (Fig. 8) (13). Similar data for matching at HLA-DR approaches statistical significance (p = 0.08) (Fig. 9). A longer follow-up of an even larger, multicenter series of patients is necessary to confirm these initial observations.
Figure 8.
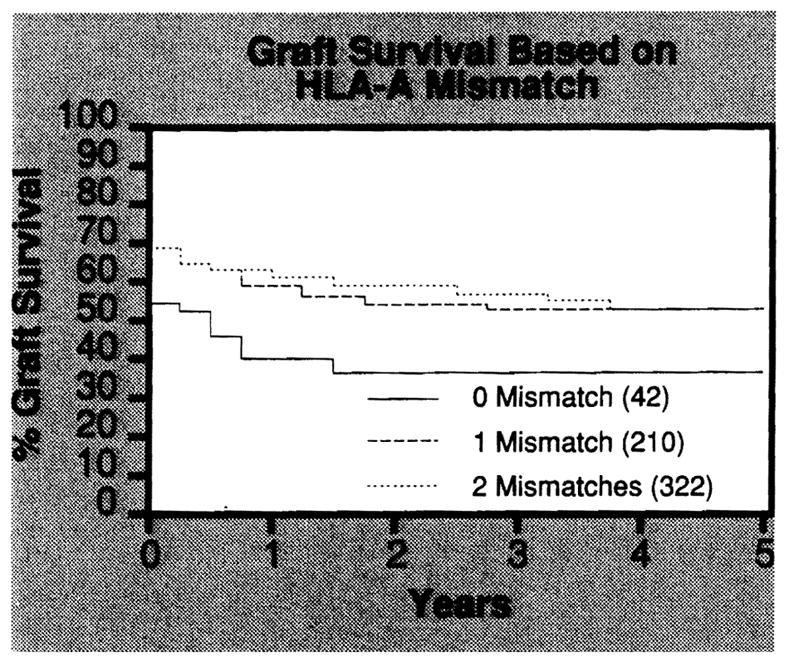
Actuarial survival of liver grafts based on number of mismatches at the HLA-A locus. The long-term survival of grafts with zero mismatch at HLA-A was significantly less (p<0.03) than survival of grafts with one or 2 mismatches. Adapted from Markus et al, Transplant Proc, in press.
Figure 9.
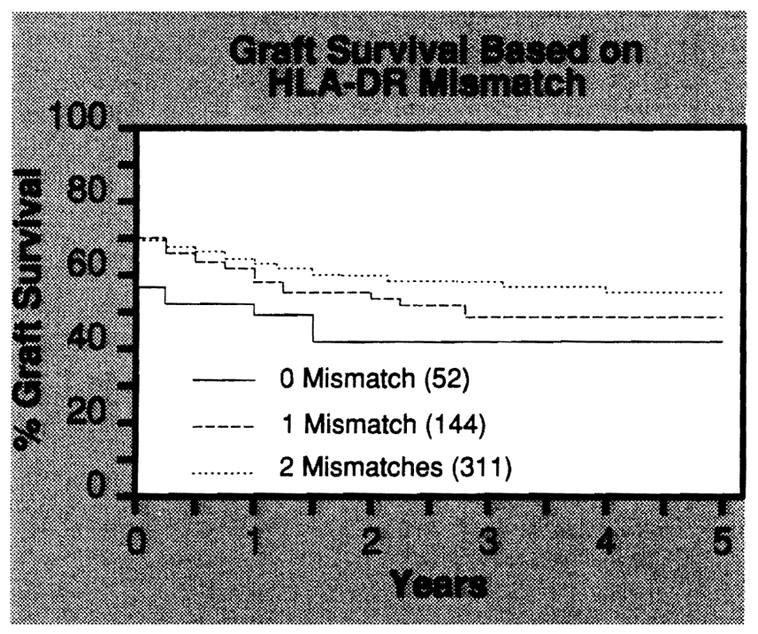
Actuarial survival of liver grafts based on number of mismatches at the HLA-DR locus. The long-term survival of grafts with zero mismatch at HLA-DR was less than survival of grafts with one or two mismatches, but the differences are not statistically significant (p = 0.08). Adapted from Markus et al, Transplant Proc, in press.
It has been suggested that this paradoxical effect of HLA matching might represent a dualistic effect of HLA antigens involving self-recognition (MHC restricted processing of autoantigens) on the one hand and alloreactivity on the other. Some of the more common causes of end-stage liver disease, such as primary biliary cirrhosis, sclerosing cholangitis, and viral hepatitis, involve immune mechanisms which might be facilitated by HLA matches. However, we have no direct evidence that disease recurrence facilitated by HLA matching is responsible for graft loss.
Acknowledgments
This study was supported by Research Project Grant No. AM-29961 from the National Institutes of Health, Bethesda, Maryland. L.M. is the recipient of a Centennial Fellowship from the Medical Research Council of Canada.
References
- 1.Starzl TE, et al. Evolution of liver transplantation. Hepatology. 1982;2:614–636. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fung JJ, Demetris AJ, Porter KA, et al. Use of OKT3 with cyclosporine and steroids for reversal of acute kidney allograft rejection. Nephron. 1987;96:19–33. doi: 10.1159/000184431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fung JJ, Markus BH, Gordon RD, et al. Impact of Orthoclone OKT3 on liver transplantation. Transplant Proc. 1987;19:37–44. [PMC free article] [PubMed] [Google Scholar]
- 4.Iwatsuki S, Gordon RD, Shaw BW, Jr, Starzl TE. Role of liver transplantation in cancer therapy. Ann Surg. 1985;202:401–407. doi: 10.1097/00000658-198510000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Starzl TE. Experience in hepatic transplantation. Philadelphia: WB Saunders Company; 1969. (with the assistance of CW Putnam) [Google Scholar]
- 6.Gordon RD, Iwatsuki S, Esquivel CO, et al. Liver transplantation across ABO blood groups. Surgery. 1986;100:342–348. [PubMed] [Google Scholar]
- 7.Gordon RD, Iwatsuki S, Esquivel CO, et al. Experience with ABO blood groups in liver transplantation. Transplant Proc. (in press) [PMC free article] [PubMed] [Google Scholar]
- 8.Opelz G. Effect of HLA matching, blood transfusions, and presensitization in cyclosporine-treated kidney transplant recipients. Transplant Proc. 1985;6:2179–2183. [Google Scholar]
- 9.Kissmeyer-Nielsen F, Olsen S, Peterson VP, Fjeldborg O. Hyperacute rejection of kidney allografts, associated with pre-existing humoral antibodies against donor cells. Lancet. 1966;2:662–665. doi: 10.1016/s0140-6736(66)92829-7. [DOI] [PubMed] [Google Scholar]
- 10.Patel R, Terasaki PI. Significance of the positive crossmatch test in kidney transplantation. N Engl J Med. 1969;14:735–739. doi: 10.1056/NEJM196904032801401. [DOI] [PubMed] [Google Scholar]
- 11.Fung JJ, Griffin M, Duquesnoy R, Shaw B, Starzl T. Sucessful sequential liver-kidney transplantation in a patient with preformed lymphocytotoxic antibodies. Transplant Proc. 1987;19:767–768. [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon RD, Fung JJ, Markus B, et al. The antibody crossmatch in liver transplantation. Surgery. 1986;100:705–715. [PMC free article] [PubMed] [Google Scholar]
- 13.Markus BH, Duquesnoy RJ, Gordon RD, et al. Association of HLA compatibility and decreased liver transplant survival. Transplant Proc. (in press) [PMC free article] [PubMed] [Google Scholar]