Abstract
Introduction
Eccentric contractions are thought to induce greater low frequency fatigue (LFF) and delayed onset muscle soreness (DOMS) than concentric contractions. This study induced a similar amount of eccentric quadriceps muscle fatigue during either a concentric or eccentric fatigue task to compare LFF and DOMS.
Methods
Subjects (n=22) performed concentric or eccentric fatigue tasks using 75% of the pre-fatigue maximal voluntary contraction (MVC) torque, and both tasks ended when the MVC eccentric torque decreased by 25% pre-fatigue.
Results
When subjects reached the failure criterion during the eccentric and concentric tasks, the concentric MVC was 78 ± 9.8% and 64 ± 8.4% of initial, respectively. LFF was greater after the concentric than the eccentric protocols (22 ± 12.4% and 15 ± 7.6% increase, respectively; p < 0.01). DOMS was over 100% greater for the eccentric protocol.
Discussion
These results indicate that DOMS is not dependent on the events that contribute to LFF.
Keywords: Muscle fatigue, Excitation - contraction coupling, Muscle damage, Delayed onset muscle soreness
INTRODUCTION
Multiple physiological mechanisms contribute to force loss during muscle fatigue.1,2 The type of contraction during repetitive activity determines the mechanism of muscle fatigue.3,4 Dynamic concentric and eccentric tasks are difficult to compare because of the varied force-generating capabilities during each task. Several previous studies report that concentric tasks induce a greater loss of force than do eccentric tasks when subjects are asked to perform repetitive maximal voluntary contractions (MVCs).5–9 However, controlling for the amount of eccentric muscle fatigue across both contraction types has not been studied previously.
Historically, lengthening contractions are believed to induce more muscle damage than shortening contractions.10–12 When muscle fibers are lengthened in an eccentric task, active actin-myosin bonds are disrupted mechanically rather than undergoing ATP-dependent detachment and reattachment.13 This forceful disruption of active cross-bridges creates high stresses on cross-bridge proteins and triggers acute inflammatory responses and muscle pain 24 and 48 hours after exercise.11 Therefore, delayed onset muscle soreness (DOMS) is greater after eccentric (ECC) exercise than concentric (CON) exercise14–16, but direct comparison between these protocols is often difficult to interpret because each contraction type produces different peak torques.
Low frequency fatigue (LFF) is believed to be a primary source of peripheral fatigue during lengthening contractions.15,17,15 LFF is characterized as long lasting, and can be defined as a preferential decrease in the force elicited with electrical stimulation at a low frequency, compared to a high frequency.18 The proposed mechanism of LFF is a fatigue-induced reduction in Ca2+ release from the sarcoplasmic reticulum (SR) per action potential.19 Although both CON and ECC tasks can induce LFF,20–22 studies without controlled criteria for task failure support that ECC tasks induce greater LFF than do CON tasks.16,17 Because it takes hours or days to recover from LFF, it is suggested that damage to structural proteins during eccentric contractions is also linked to LFF.19,23
Studies show that, in addition to the high mechanical stress on the structural elements that occurs with repetitive ECC contractions, metabolite changes (such as calcium and inorganic phosphate) can reduce the amount of Ca2+ release from the SR.24–27 Because CON contractions have been known to have higher metabolite turnover than ECC contractions,28 different physiological mechanisms may contribute to LFF after CON exercise in comparison with post-ECC exercise. We have previously found that the amount of LFF was similar if the same amount of isomeric fatigue was induced by sustaining either 35% MVC or 65% MVC, indicating that the amount of LFF may be fatigue-dependent.29 Moreover, Dundon, Cirillo and Semmler21 have recently shown that the amount of LFF was similar even after dynamic (CON or ECC) contractions of the biceps if the same amount of isometric fatigue was induced, indicating the importance of controlling for the amount of fatigue induced across different contraction types. However, to our knowledge, no previous studies have induced a similar amount of eccentric muscle fatigue to a weight-bearing muscle (quadriceps) in order to compare both concentric and eccentric contractions. Because the quadriceps muscle is repetitively active eccentrically during gait, it may experience muscle specific adaptations as a result of regular eccentric exercise.30 Controlling for the extent of ECC fatigue in the quadriceps may therefore result in new observations on the relationship between DOMS and LFF. Moreover, there are known differences in activation strategies during isometric and dynamic muscle contractions.31
Accordingly, the goal of this study was to induce a similar amount of eccentric muscle fatigue through either a concentric or an eccentric task contraction in the quadriceps muscle in order to compare the effects of task on low frequency fatigue and delayed onset muscle soreness. We hypothesized that low frequency fatigue and delayed-onset muscle soreness are independent of contraction type.
MATERIALS AND METHODS
Subjects and general design
Thirty-two healthy male subjects (22 for exercise and 10 for control groups) participated in this study. Only male subjects were recruited to eliminate gender differences in endurance time.32,33 Those in the exercise group [age = 24. 9 ± 3.7 (mean ± SD) yr; height = 181.5 ± 6.6 cm; weight = 78.4 ± 7.8 kg] were enrolled in the CON and ECC exercise tasks. All subjects reviewed and signed a consent form approved by the institutional review board at the University of Iowa.
Eleven of the 22 exercise subjects began with the CON task, while the remaining 11 began with the ECC task. One week after the first testing session (CON or ECC task), each subject completed the opposite task (CON or ECC). A group of subjects who were not assigned to the exercise group (n = 10) served as controls to verify the stability of all measurements within a session. The subjects were in good health without any current or previous knee problems, injuries, and/or surgeries.
At the first session, all subjects were familiarized with the experimental set-up and were asked to practice non-fatiguing submaximal and maximal isokinetic concentric and eccentric contractions of the knee extension muscles. On a separate day, after the familiarization session, subjects in the exercise group participated in the two exercise sessions (CON or ECC) separated by 1 week. Both CON and ECC MVCs were performed before and after fatigue regardless of the exercise session (CON or ECC). The pre and post-fatigue MVCs were completed in an order that was based on the protocol (ECC or CON) that they were performing. If the fatigue protocol was ECC, then the ECC MVCs were performed first and vice versa for the CON task. Subjects in the control group participated in one testing session on a separate day after the familiarization session. The control subjects received all testing procedures in the absence of any fatigue protocol. The order of MVC type (CON or ECC) in the control session was counterbalanced, so half of the control subjects performed CON MVCs first. All subjects were asked to refrain from any strenuous physical activity for the duration of the study.
Instrumentation and experimental set-up
Torque recording
Subjects sat upright on a Kin-Com 125E+ (Chattex Corp; Chattanooga, TN) computer-controlled isokinetic dynamometer. In this study, the right leg was used for all subjects, as they were all right handed. The subjects were strapped with a seat belt, shoulder and thigh straps to stabilize the trunk and the thigh. The knee joint axis was aligned with that of the Kin-Com’s mechanical axis for each subject. Sufficient space was maintained between the popliteal fossa and the Kin-Com seat for each subject to prevent discomfort and occlusion of blood flow. The Kin-Com force transducer was positioned on the anterior aspect of the tibia at a level just superior to the lateral malleolus, and the output of the transducer was displayed on an oscilloscope for visual feedback. The distance from the transducer to the mechanical axis of the Kin-Com was used as a moment arm for torque calculations. For voluntary contractions, the range of motion of 50° to 90° (0° = full knee extension) was used with a work/rest velocity of 13° sec−1/7° sec−1. During each protocol, the rest occurred during the 7° sec−1 time, the limb was passively returned to the starting position, resulting in a duty cycle of ~3.1 sec exercise/~5.7 sec rest. It has been shown that, at a slow speed (20° sec−1), central activation levels are similar for concentric and eccentric contractions for knee extension.34 Strong verbal encouragement was given to the subjects while they performed all MVCs. For isometric contractions elicited by electrical stimulations (see below), the knee was locked in 90° of flexion.
Electrical stimulation
The quadriceps was electrically stimulated to quantify the amount of LFF by calculating a ratio of the double pulse torque (doublet) to the single pulse torque (D/S ratio), using two gel adhesive pads (3.5 × 5 cm; VersaStim by Con-Med Corp; Utica, NY). The stimulation pads were applied at 40% and 80% of the distance from the anterior superior iliac spine to the superior patellar pole. Acustom designed stimulator (constant current; 50 μA – 200 mA range with <5% current variations; total capability 400 V) with a built in isolation unit was used for all stimulation protocols. The D/S ratio is an effective method to quantify LFF consistent with the literature using trains of high and low frequency stimulation.35–37 In addition, the D/S ratio is less likely to induce muscle fatigue,38 and, because of its greater comfort when compared to longer stimulation trains, minimizes post stimulus co-activation artifact. Moreover, it has been previously shown that the D/S ratio is a reproducible and sensitive means to quantify the amount of LFF for the human quadriceps.29
At the beginning of each session, a maximal stimulation intensity was determined by increasing the intensity until no further increase in peak torque was elicited with a 500 micro-second single pulse (mean pre-fatigue twitch torque = 61.3 ± 8.7 Nm). Once the maximal intensity was determined, this intensity was maintained throughout the session. A doublet was elicited by delivering two pulses separated by 6 ms (166 Hz), and these two pulses always preceded the single pulse by 3 s. The subjects received 18 pairs of single and double pulses for each measurement.
Visual analog scale (VAS)
VAS was used to assess the extent of pain/soreness felt in the tested quadriceps muscle.39,40 Subjects were asked to place a mark on a horizontal 100 mm line to indicate the maximum amount of pain/soreness experienced during the 24 and 48 hrs after the fatigue protocol. The starting (0 mm) and endpoint (100 mm) on the 100 mm line corresponded to “no pain/soreness at all” and “worst pain/soreness imaginable”, respectively.
Procedures
Pre-fatigue measurements
Before subjects were seated on the Kin-Com, they biked comfortably for 5 min to warm up their quadriceps. After the warm-up, they were seated on and secured to the Kin-Com. Stimulating electrodes were placed on the thigh, and the maximal stimulating intensity was determined as described above. The subjects performed 17 (either CON or ECC) contractions; the first 14 were low-level contractions to warm up the muscle. The subjects were instructed to provide less than a 30% effort, and at least 1-minute rest separated each contraction. The last 3 contractions were maximal. Then, the subjects repeated the same procedure in the contraction type that had not been performed (CON or ECC). The highest peak torque among the last 3 CON and ECC MVCs was used to calculate the target torque of 75% CON and 75% ECC contractions, respectively, for the fatigue protocol, and the target torque was displayed on the oscilloscope. Seventy-five percent was chosen, because 100% MVC would be too centrally demanding and a lower percent of MVC would last longer in time and increase the likelihood of central fatigue.41,42 Next, the quadriceps was electrically stimulated to obtain the D/S ratio.
Fatigue protocol
For the CON fatigue protocol (Figure 1A), subjects performed CON contractions of the quadriceps at the target torque of pre-fatigue 75% CON contraction. Similarly, for the ECC fatigue protocol (Figure 1B), the subjects performed ECC contractions at the target torque of pre-fatigue 75% ECC contractions. For both CON and ECC protocols, subjects were asked to reach the target as quickly as possible once the work phase had started and to maintain the target torque throughout the work phase. In both cases (CON and ECC protocols), the protocol was terminated when the subjects were not able to reach the 75% of the pre-fatigue ECC contraction maximal torque.
Figure 1.
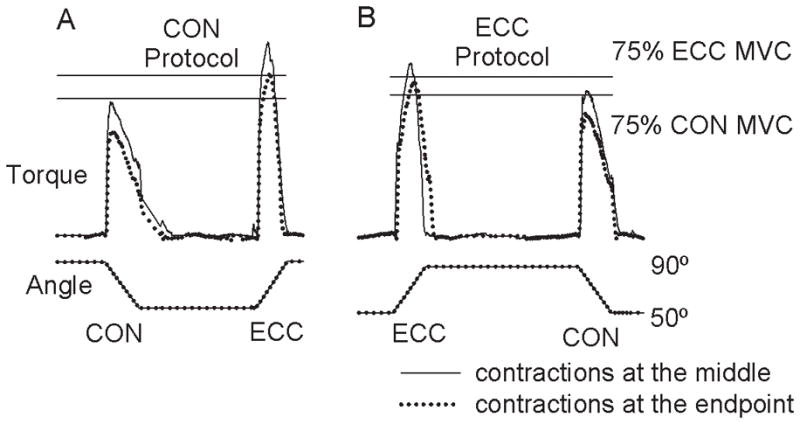
Representative data recorded during concentric (A) and eccentric (B) fatigue protocols. From the top, knee extension torque and knee angle are shown. The two horizontal lines “75% ECC MVC” and “75% CON MVC” are the target lines used in the protocols, each of which corresponds to 75% of pre-fatigue eccentric and concentric MVC torques, respectively. The solid and dotted torque lines indicate the torque recorded at the middle and end of the fatigue protocols. In the CON protocol (A), the subject performed repetitive, fatiguing 75% CON MVCs with single ECC MVCs performed periodically (only 1 for each is shown). The protocol was continued if the ECC MVCs exceeded the target torque, and this was the case even after the subject was not able to reach the target torque concentrically (the dotted line on the left). Similarly, in the ECC protocol (B), the subject performed 75% ECC contractions until the eccentric contraction torque fell to the 75% ECC MVC line (ECC contraction with a dotted line). After this contraction, one maximal concentric contraction (CON contraction with a dotted line) was recorded.
In order to establish the end point criterion, the subjects were asked to perform 1 CON or ECC MVC every 20th contraction in the ECC or CON protocol, respectively. Pilot data supported that this frequency of assessing ECC torque was sensitive enough to use as a stopping criterion and not frequent enough to interfere with the CON task. Because no subjects approached the ECC torque-stopping criterion early during either protocol, the first ECC or CON MVC performed in the fatigue protocol was always after the initial 25 contractions. If the ECC MVC torque sampled during the CON protocol exceeded the pre-fatigue 75% ECC MVC torque (the torque in the solid line during the ECC contraction in Figure 1A), the CON protocol was continued even if the subjects were not able to reach the 75% CON MVC torque target. Thus, for both exercise groups, the ending point was always a 25% decrease in eccentric torque.
Post-fatigue measurements
Immediately after the termination of the ECC fatigue protocol, one CON MVC was performed. Then, the knee joint was locked at a 90° angle, and the quadriceps was stimulated to obtain the double pulse to single pulse ratio (D/S ratio). After a rest of 5 min, subjects were asked to perform 5 contractions, the first 4 being at the same low level to warm up the muscle and the last one being maximal for one type of contraction (ECC or CON). This was repeated for the opposite contraction type. The order of the contraction type performed after fatigue was the same as that for the pre-fatigue MVCs in the session. After these post-5-min MVCs, post-5-min D/S ratios were obtained. This set of measurements was repeated at 10, 15 and 20 min post fatigue for the subjects in the exercise group. For the subjects in the control group, the muscle was stimulated only once after performing MVCs following quiet sitting of 20 min. All the subjects returned to the laboratory the next day approximately 24 hr after the termination of the fatigue protocol, and repeated the same measurements. For the subjects in the exercise group, VAS was recorded 24 and 48 hrs after the protocol.
Data analysis
The force was sampled at 1,000 Hz. The volitional maximal and elicited peak force was calculated as the highest value of the force signal and then multiplied by the moment arm to obtain torque for each subject. For the volitional torque analyses, windows of the middle 30° (55° – 85°) of the full 50° – 90° flexion range were used to ensure that the initial data recorded was representative of when either muscle lengthening or shortening occurred. The last pair of CON and ECC MVCs in the fatigue protocols was used as endpoint MVCs, which are shown in Figure 1 with dotted lines.
Each of the last 3 twitch and doublet peak torques was determined, and then the double pulse peak torque was divided by the single pulse peak torque to obtain the D/S ratio. Only the last 3 pairs were used to calculate the ratio, because it was very stable (coefficient of variation less than 2%). Moreover, it has been shown that the potentiated twitch is a more sensitive and reproducible index of contractile fatigue than is the unpotentiated twitch.43
The VAS was analyzed by taking the distance between the starting point (0 mm) and the mark subjects indicated on the VAS line. This indicated the extent of pain/soreness 24 and 48 hrs following fatigue.
Statistical Analysis
Two-way analysis of variance (ANOVA) for repeated measures was used to test the effects of protocol (ECC vs. CON) and time on twitch and doublet peak torque, the D/S ratio, and VAS. Three-way ANOVA for repeated measurements was used on MVC torque to test the effect of protocol, contraction type (ECC vs. CON) and time. One-way repeated ANOVA was performed on the data from the control group to determine whether the measurements were stable across time, and independent t test was used to compare control data with those from the exercise group. Significance was set at 0.05, and post-hoc analysis was performed when necessary. Data are reported as mean ± standard deviation in the text and as mean ± standard error in the figures.
RESULTS
Voluntary torque and fatigue protocol
Before the fatigue protocol, ECC MVC torque (559.2 ± 89.6 Nm and 564.3 ± 82.6 Nm for the CON and ECC exercise sessions, respectively) was about 23% higher than the CON MVC torque (454.2 ± 81.1 Nm and 455.7 ± 90.1 Nm for the CON and ECC exercise sessions, respectively) with no differences across sessions within contraction type. The number of CON and ECC contractions that were necessary to induce a 25% decrease in ECC MVC torque was similar across sessions (58.0 ± 22.6 and 64.1 ± 21.2 for CON and ECC protocols, respectively; p = 0.2). The fatigue protocols lasted approximately 15 min on average. When the fatigue protocol was terminated, the muscle reached the same magnitude of eccentric fatigue regardless of the exercise protocol used. This was confirmed by the observation of no difference in ECC MVC torque at the endpoint of the fatigue protocol across sessions (75.3 ± 3.5% and 74.0 ± 5.0% for the CON and ECC sessions, respectively; p = 0.25, Figure 2). The endpoint CON MVC torque was higher when the muscle was fatigued eccentrically compared to when the muscle was fatigued concentrically (77.6 ± 9.8% of the pre-fatigue CON MVC torque vs. 64.2 ± 8.4% for ECC and CON protocols, respectively; p < 0.05). After a rest of 5 min, all four (ECC and CON MVCs in CON and ECC sessions) recovered to about 83% of their respective pre-fatigue values and stayed at ~ 85% of the respective pre-fatigue values until 20 min post fatigue. There was no difference among these MVC torques between 5 and 20 min post fatigue (p = 0.31). At 24 hr post fatigue, more recovery from the 20 min post fatigue condition was seen in all 4 MVC torques, resulting in values ranging from 89.7 ± 7.8% (CON MVC in ECC session) to 98.5 ± 9.0% (CON MVC in CON session) of the respective pre-fatigue condition.
Figure 2.
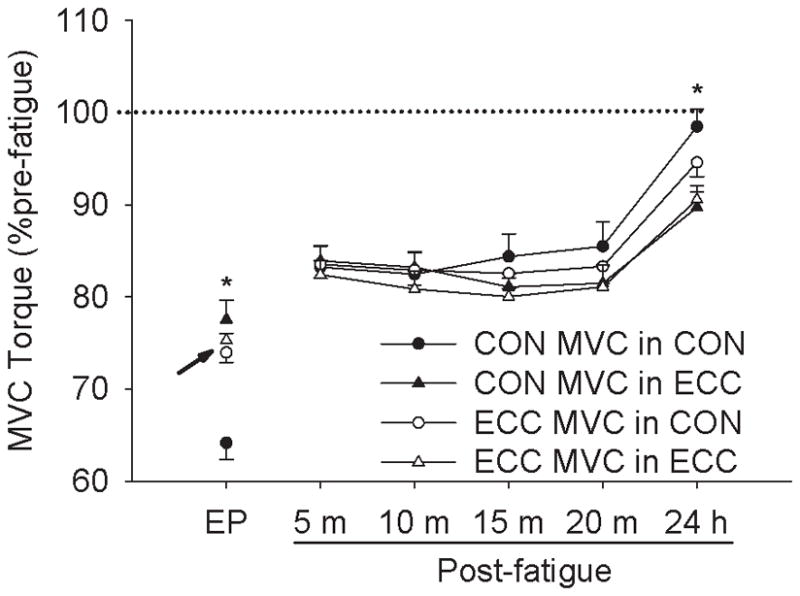
Changes in MVC torque for the two contraction types (concentric and eccentric contractions) in the two protocols (concentric and eccentric exercise protocols) at endpoint (EP) and 5 min (5 m) to 24 hr (24 h) post fatigue protocol as a percentage of respective pre-fatigue values. The arrow indicates the 25% reduction in eccentric torque as the criterion used to terminate the fatigue both the concentric and eccentric protocols.
* indicates significant differences in the CON MVC torque between the two protocols.
Twitch and doublet torque and D/S ratio
Twitch and doublet peak torque
An example of the double and single pulse torque curves during various times for each contraction type is shown in Figure 3. Both CON and ECC fatigue protocols decreased the twitch and doublet torque significantly with no (p > 0.05) change in the control data. However, the twitch and doublet torque both decreased more after the CON protocol than the ECC protocol (56.2 ± 13.6% and 67.5 ± 11.7% pre-fatigue for CON and ECC, respectively for twitch; p < 0.01, and 67.5 ± 12.6% and 76.9 ± 10.1% pre-fatigue for CON and ECC, respectively for doublet; p < 0.01; Figure 4A). The significant differences across sessions that were present immediately after the fatigue protocol in both twitch and doublet were absent by 5 and 15 min post fatigue, respectively. At 24 hr post fatigue, both the twitch and doublet were significantly reduced in the ECC protocol group compared to the CON protocol group (p < 0.05). At 24 hr post fatigue both single and doublet pulse torques were significantly recovered from the respective values at 20 min post fatigue, but only the double pulse torque from the concentric protocol had returned to control values (p > 0.05 for CON vs. Control in the doublet at 24 hr post fatigue).
Figure 3.
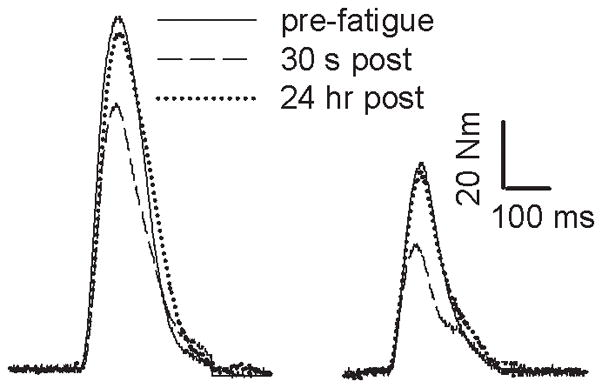
Representative double pulse twitch (doublet; left) and single pulse twitch (right) torque elicited with the knee joint angle at 90° before (pre-fatigue) and after (30 s and 24 hr) the fatigue protocol. For clarity only 3 traces are shown, and the 3-s rest between twitch and doublet has been shortened.
Figure 4.
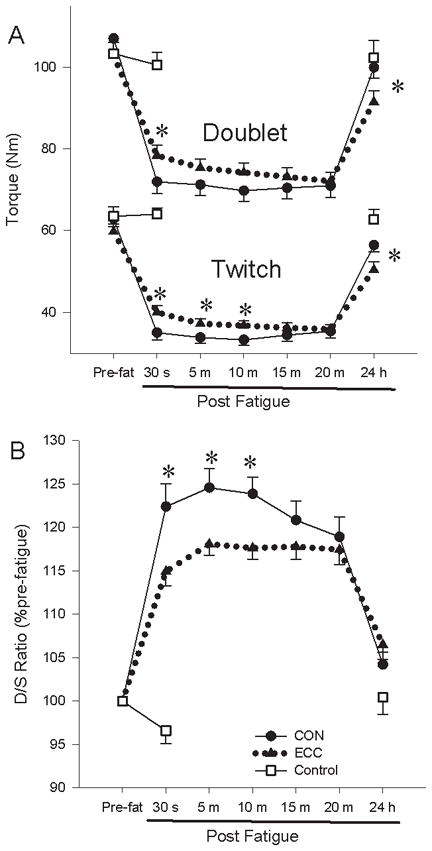
Changes in twitch and doublet peak torque (A) and D/S ratio (B) before (Pre-fat) and immediately (30 s) to 24 hr (24 h) post fatigue in CON, ECC, and control protocols as an absolute torque (A) and as a percentage of respective pre-fatigue values (B).
* indicates significant differences between the two protocols.
D/S ratio
The ratio from the control data showed no (p > 0.05) changes across times, whereas the ratio increased significantly after the fatiguing contractions (Figure 4B). However, the increase in the ratio was greater after the CON protocol than the ECC protocol (122.4 ± 12.4% and 114.9±7.6% pre-fatigue for CON and ECC sessions, respectively; p < 0.01). The ratio was greater for the CON protocol until 10 min post fatigue. After 24 hrs the ratios were not different between the ECC and CON protocols (p = 0.12), but they were significantly greater than control values (p < 0.05).
Visual analog scale
The ECC fatigue protocol induced significantly more pain/soreness than did the CON protocol at both 24 and 48 hrs post fatigue (24 hr = 15 ± 19 mm and 37 ± 20 mm and 48 hr = 12 ± 17 mm and 32 ± 20 mm for CON and ECC sessions, respectively; p < 0.05 for both 24 and 48 hrs; Figure 5). The amount of pain/soreness felt in the quadriceps did not differ (p = 0.32) between 24 and 48 hrs post fatigue in either of the two sessions. To further examine the relationship between exercise-induced muscle soreness/pain and low frequency fatigue, correlation analyses were done between the D/S ratio and VAS. There was no association between the degree of LFF and muscle soreness/pain in either protocol (r2 = 0.01 and 0.02 for CON and ECC protocols, respectively; Figure 6). When both groups were combined, there was no association between LFF and the VAS (r2 = 0.015).
Figure 5.
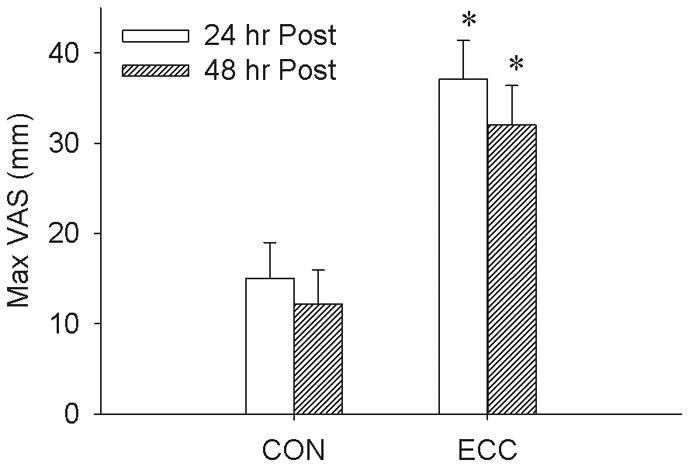
Mean maximal visual analog score at 24 and 48 hr post fatigue as an absolute distance in mm in the CON and ECC exercise protocols.
* indicates significant differences between the two protocols.
Figure 6.
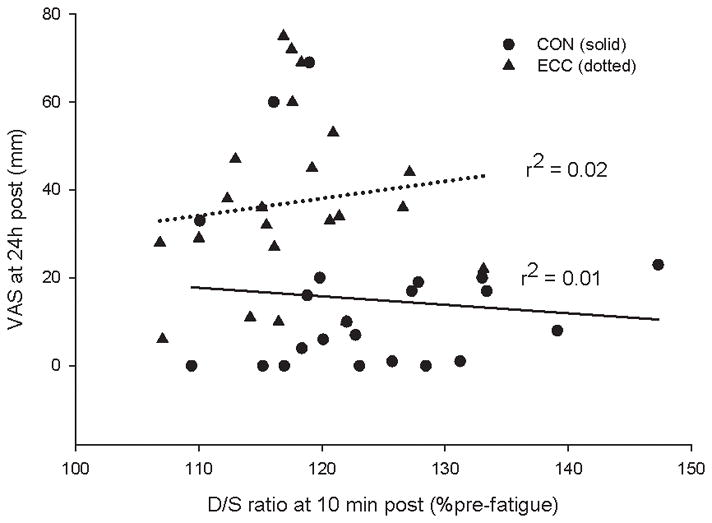
A scatter plot showing the relationship between the D/S ratio measured 10 min post fatigue and the VAS score taken 24 h post fatigue in both CON and ECC exercise protocols. The best-fit lines with their r2 values are presented for the two protocols.
DISCUSSION
A general belief is that ECC contractions are more fatigue resistant than CON contractions.8,9 In this study, we induced the same level of eccentric muscle fatigue with a CON or ECC exercise protocol. The major finding was that greater LFF was necessary to induce a 25% decrease in eccentric torque under the CON protocol, however this type of peripheral fatigue was not the primary contributor to delayed onset muscle pain (damage). This study supports the notion that “how one induces fatigue rather than the amount of muscle fatigue” is an important consideration in understanding muscle damage (DOMS) and injury during exercise. This finding advances the concept that LFF is fatigue dependent.29
Fatigability of concentric and eccentric contractions
In the present study, CON MVC torque decreased to 64% of pre-fatigue in order to decrease the ECC MVC torque to 75% of the pre-fatigue value (Figure 2). Previous studies have been less successful in inducing ECC MVC fatigue during eccentric exercise to enable direct comparisons with concentric exercise.44,9 We attribute our ability to induce a 25% decrease in eccentric torque during repetitive eccentric contractions because we attempted to minimize central fatigue. Preliminary studies supported that by using 1) slower contraction speeds, 2) 75% MVC as the target torque rather than 100% MVC, and 3) subjects that were motivated to give full effort when performing pre and post-fatigue MVCs. These all assisted with obtaining muscle fatigue eccentrically. The significant and prolonged decrease in twitch torque supports the concept that extensive peripheral muscle fatigue contributed to the torque decline. Accordingly, our findings were similar to those of Binder-Macleod and Lee45 who used electrical stimulation to induce comparable force loss by ECC and CON contractions.
Long-lasting peripheral fatigue (low frequency fatigue) and muscle damage
We induced a similar amount of eccentric fatigue by two different exercise protocols (CON and ECC), and both protocols led to long-lasting low frequency fatigue as evident by the increase in the double to single pulse ratio. The eccentric protocol, however, induced over 150% more muscle soreness at 24 and 48 hours post exercise than the concentric exercise protocol. The dissociation between LFF and muscle soreness suggests that the mechanisms that lead to muscle damage (and subsequent soreness) were independent of the mechanisms of LFF.
By design, both protocols caused the same amount of eccentric muscle torque loss, but the CON protocol showed greater LFF. Noteworthy is that the peak twitch and doublet torque as well as the MVCs were all more impaired at 24 hours after the eccentric fatigue protocol. Although it has been shown that the central nervous system can compensate for decreased volitional torque resulting from LFF by increasing motor unit firing frequencies,35 the increased pain after the ECC protocol may have induced volitional and/or reflexive inhibition, leading to a more pronounced decrease in MVCs 24 hours after the ECC protocol. However, Prasartwuth, Taylor, and Gandevia46 showed that the pain after repetitive ECC contractions contributes minimally to the prolonged force loss through reduced voluntary activation in the elbow flexors.
Both eccentric and concentric fatigue protocols induced a long-term loss of muscle force in this study. One of the physiological processes in force generation responsible for LFF is the excitation-contraction coupling system.19 The D/S ratio confirmed that the concentric protocol induced greater LFF than the eccentric protocol (perhaps because of the need to concentrically fatigue to a greater extent in order to induce the required 25% reduction in eccentric torque). However, after 24 hours, the ratio for the concentric and eccentric groups was similarly recovered, but the twitch and MVC torques remained significantly reduced for the eccentrically exercised group. At this same time, the eccentrically exercised group experienced more muscle pain. Thus, a component of the prolonged loss of torque from the eccentric protocol may have been attributable to muscle damage beyond the excitation-contraction coupling system.
The cause of pain/soreness with ECC contractions may be associated with repetitive over-stretching of elastic non-contractile tissues, leading to increases in hydroxyproline and creatinine ratios at peak muscle soreness.47 The 25% decrease in eccentric torque with a concentric protocol required a greater amount of LFF (which was confirmed by our D/S ratios), perhaps because the concentric protocol induced minimal muscle damage (confirmed by 24/48 hr pain assessments). However, the eccentric contractions may have induced some muscle damage so that the 25% eccentric fatigue threshold required less LFF to meet the stopping criterion.
LFF is often associated with muscle damage that occurs with eccentric exercise. Compromised excitation-contraction coupling has been attributed to “damage” to the triads (t-tubules to the terminal cisternae of the SR).19,48 The precise mechanism of the impairment at this site is not fully understood, but repeated high Ca2+ transients and increased production of reactive oxygen species (ROS) has been suggested to attenuate Ca2+ release.49 In addition, it has been suggested that inorganic phosphate, which increases considerably with fatigue, also reduces Ca2+ release from the SR through precipitation of calcium phosphate.25
In this study, the type of damage associated with LFF after the CON protocol does not appear to be the same damage that leads to significant DOMS observed after repetitive ECC contractions. The repetitive ECC contraction-induced damage that results in DOMS has been reported to preferentially reduce torque through a process of redistribution of sarcomere lengths.18,50,49 Therefore, damage to the triad resulting from changes in metabolites and damage to the elastic non-contractile tissues resulting from over-stretching may have contributed to the degree of LFF after the CON and ECC protocols in this study.
It is well documented that CON contractions have higher metabolic turnover,28 whereas ECC contractions are more mechanically stressful.10,12 Recently, LFF was found after both concentric and eccentric exercise of the biceps brachii, with a faster recovery observed with eccentric exercise.22 The authors suggested that increased LFF up to 20 min after fatigue may be more closely related to the changes in muscle metabolites, whereas the more prolonged LFF (beyond 20 min after fatigue) may be related to damage of the structures that are involved in force generation after Ca2+ has been extensively released from the SR. In support of this view, is the finding that submaximal ECC contractions result in less LFF than submaximal CON contractions consistent with greater metabolic demand with shortening contractions.20, 8 However, if the same amount of isometric fatigue is induced, the amount of LFF has been shown to be similar after ECC and after CON fatigue protocols.21 Consequently, our results differ in certain aspects from the study of Dundon and colleagues,21 likely because of the difference in the failure criterion used (~35% decrease in isometric MVC vs. ~25% decrease in ECC MVC used in our study) and that a lower extremity muscle (quadriceps) was examined.
The LFF after the CON protocol (the changes in the D/S ratio from 30 s to 20 min, Figure 4B) may reflect a relatively quick recovery of metabolites in the muscle with rest. It is possible that the accumulation of metabolites causes damage to both the triad and the elastic, non-contractile elements since it has been found that titin, a large elastic protein that keeps the thick filament centered in the sarcomere by anchoring it to the Z line, is also susceptible to proteolytic damage due to increased intracellular Ca2+.51 However, during CON contractions, where actin-myosin bonds undergo ATP-dependent detachment, these elastic, non-contractile elements are likely more protected.
Central fatigue, which was not quantified, could play a differential role during each respective type of fatigue (CON and ECC) in this study.31,52,44 However, we would not expect to observe the magnitude of muscle soreness and LFF during the ECC and the CON protocols, respectively, if central fatigue played a prominent role. Previous reports indicate that the level of peripheral fatigue is positively correlated with the level of voluntary activation.53 With respect to the CON protocol, our D/S ratio confirms that extensive peripheral fatigue developed. With respect to the ECC protocol, the DOMS and D/S ratio indicate that we induced significant peripheral changes with each protocol, a finding that would have been minimized if messages were not delivered to the sarcolemma (central inactivation). Both structural damage (pain) and LFF reflect peripheral changes that appeared to be consistent in this study. However, a limitation of this study is that we do not have direct measures of central activation. Moreover, we are not certain as to the extent of central activation, if measured, that would rise to the level to influence the LFF and DOMS metrics used in this study.
A second potential limitation relates to the overall sensitivity of the D/S ratio used to measure LFF between the two protocols. However, in individuals with spinal cord injury, the doublet pulse activation is sensitive to muscle physiological properties.54 In addition, under isometric conditions, when LFF is expected to be less, the D/S ratio increased only 8–10%29; whereas during the long-term intermittent contractions induced in this study, the D/S ratio increased ~ 25%. Accordingly, the D/S ratio appeared to have adequate sensitivity to detect low frequency fatigue between the two protocols.
Summary and Conclusions
By inducing the same amount of eccentric muscle fatigue via concentric and eccentric protocols, we were able to demonstrate different degrees of low frequency fatigue and delayed onset muscle soreness. Accordingly, even if the same amount and type of fatigue is induced, such as a 25% reduction in eccentric torque, how the fatigue is induced is fundamental to the development of excitation-contraction coupling compromise and delayed onset muscle soreness. These findings help explain why adaptations induced by training need to be specific to the contraction type.
Acknowledgments
National Institutes of Health Award R01-NR 010285-05 (R. K. Shields), Andrew J. Meszaros, Mike J. Stodden, Christopher R. Schroeder, Glenn P. Reifenrath, and Stephen T. Wieskamp.
Abbreviations
- CON
concentric
- D/S ratio
a ratio of double pulse torque (doublet) to single pulse torque (twitch)
- DOMS
delayed onset muscle soreness
- ECC
eccentric
- LFF
low frequency fatigue
- MVC
maximal voluntary contraction
- SR
sarcoplasmic reticulum
- VAS
visual analog scale
Footnotes
DISCLOSURES
The authors have declared that no competing interests exist.
References
- 1.Fitts RH. Cellular mechanisms of muscle fatigue. Physiol Rev. 1994;74:49–94. doi: 10.1152/physrev.1994.74.1.49. [DOI] [PubMed] [Google Scholar]
- 2.Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. 2001;81:1725–1789. doi: 10.1152/physrev.2001.81.4.1725. [DOI] [PubMed] [Google Scholar]
- 3.Bigland-Ritchie B, Rice CL, Garland SJ, Walsh ML. Task-dependent factors in fatigue of human voluntary contractions. Adv Exp Med Biol. 1995;384:361–380. doi: 10.1007/978-1-4899-1016-5_29. [DOI] [PubMed] [Google Scholar]
- 4.Enoka RM, Stuart DG. Neurobiology of muscle fatigue. J Appl Physiol. 1992;72:1631–1648. doi: 10.1152/jappl.1992.72.5.1631. [DOI] [PubMed] [Google Scholar]
- 5.Baudry S, Klass M, Pasquet B, Duchateau J. Age-related fatigability of the ankle dorsiflexor muscles during concentric and eccentric contractions. Eur J Appl Physiol. 2007;100:515–525. doi: 10.1007/s00421-006-0206-9. [DOI] [PubMed] [Google Scholar]
- 6.Grabiner MD, Owings TM. Effects of eccentrically and concentrically induced unilateral fatigue on the involved and uninvolved limbs. J Electromyogr Kinesiol. 1999;9:185–189. doi: 10.1016/s1050-6411(98)00031-5. [DOI] [PubMed] [Google Scholar]
- 7.Hortobagyi T, Barrier J, Beard D, Braspennincx J, Koens P, Devita P, Dempsey L, Lambert J. Greater initial adaptations to submaximal muscle lengthening than maximal shortening. J Appl Physiol. 1996;81:1677–1682. doi: 10.1152/jappl.1996.81.4.1677. [DOI] [PubMed] [Google Scholar]
- 8.Pasquet B, Carpentier A, Duchateau J, Hainaut K. Muscle fatigue during concentric and eccentric contractions. Muscle Nerve. 2000;23:1727–1735. doi: 10.1002/1097-4598(200011)23:11<1727::aid-mus9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 9.Tesch PA, Dudley GA, Duvoisin MR, Hather BM, Harris RT. Force and EMG signal patterns during repeated bouts of concentric or eccentric muscle actions. Acta Physiol Scand. 1990;138:263–271. doi: 10.1111/j.1748-1716.1990.tb08846.x. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong RB, Ogilvie RW, Schwane JA. Eccentric exercise-induced injury to rat skeletal muscle. J Appl Physiol. 1983;54:80–93. doi: 10.1152/jappl.1983.54.1.80. [DOI] [PubMed] [Google Scholar]
- 11.Cheung K, Hume P, Maxwell L. Delayed onset muscle soreness: treatment strategies and performance factors. Sports Med. 2003;33:145–164. doi: 10.2165/00007256-200333020-00005. [DOI] [PubMed] [Google Scholar]
- 12.McCully KK, Faulkner JA. Injury to skeletal muscle fibers of mice following lengthening contractions. J Appl Physiol. 1985;59:119–126. doi: 10.1152/jappl.1985.59.1.119. [DOI] [PubMed] [Google Scholar]
- 13.Flitney FW, Hirst DG. Cross-bridge detachment and sarcomere ‘give’ during stretch of active frog’s muscle. J Physiol. 1978;276:449–465. doi: 10.1113/jphysiol.1978.sp012246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones DA, Newham DJ, Torgan C. Mechanical influences on long-lasting human muscle fatigue and delayed-onset pain. J Physiol. 1989;412:415–427. doi: 10.1113/jphysiol.1989.sp017624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newham DJ, Mills KR, Quigley BM, Edwards RH. Pain and fatigue after concentric and eccentric muscle contractions. Clin Sci (Lond) 1983;64:55–62. doi: 10.1042/cs0640055. [DOI] [PubMed] [Google Scholar]
- 16.Rijkelijkhuizen JM, de Ruiter CJ, Huijing PA, de Haan A. Low-frequency fatigue is fibre type related and most pronounced after eccentric activity in rat medial gastrocnemius muscle. Pflugers Arch. 2003;447:239–246. doi: 10.1007/s00424-003-1172-2. [DOI] [PubMed] [Google Scholar]
- 17.Edwards RHT, Mills KR, Newham DJ. Greater low frequency fatigue produced by eccentric than concentric muscle contractions. J Physiol. 1981;317:17P. [Google Scholar]
- 18.Jones DA. High-and low-frequency fatigue revisited. Acta Physiol Scand. 1996;156:265–270. doi: 10.1046/j.1365-201X.1996.192000.x. [DOI] [PubMed] [Google Scholar]
- 19.Bruton JD, Lannergren J, Westerblad H. Mechanisms underlying the slow recovery of force after fatigue: importance of intracellular calcium. Acta Physiol Scand. 1998;162:285–293. doi: 10.1046/j.1365-201X.1998.0292f.x. [DOI] [PubMed] [Google Scholar]
- 20.Baptista RR, Scheeren EM, Macintosh BR, Vaz MA. Low-frequency fatigue at maximal and submaximal muscle contractions. Braz J Med Biol Res. 2009;42:380–385. doi: 10.1590/s0100-879x2009000400011. [DOI] [PubMed] [Google Scholar]
- 21.Dundon JM, Cirillo J, Semmler JG. Low-frequency fatigue and neuromuscular performance after exercise-induced damage to elbow flexor muscles. J Appl Physiol. 2008;105:1146–1155. doi: 10.1152/japplphysiol.01339.2007. [DOI] [PubMed] [Google Scholar]
- 22.Smith IC, Newham DJ. Fatigue and functional performance of human biceps muscle following concentric or eccentric contractions. J Appl Physiol. 2007;102:207–213. doi: 10.1152/japplphysiol.00571.2006. [DOI] [PubMed] [Google Scholar]
- 23.Westerblad H, Bruton JD, Allen DG, Lannergren J. Functional significance of Ca2+ in long-lasting fatigue of skeletal muscle. Eur J Appl Physiol. 2000;83:166–174. doi: 10.1007/s004210000275. [DOI] [PubMed] [Google Scholar]
- 24.Allen DG, Kabbara AA, Westerblad H. Muscle fatigue: the role of intracellular calcium stores. Can J Appl Physiol. 2002;27:83–96. doi: 10.1139/h02-006. [DOI] [PubMed] [Google Scholar]
- 25.Allen DG, Westerblad H. Role of phosphate and calcium stores in muscle fatigue. J Physiol. 2001;536:657–665. doi: 10.1111/j.1469-7793.2001.t01-1-00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kabbara AA, Allen DG. The role of calcium stores in fatigue of isolated single muscle fibres from the cane toad. J Physiol. 1999;519(Pt 1):169–176. doi: 10.1111/j.1469-7793.1999.0169o.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steele DS, Duke AM. Metabolic factors contributing to altered Ca2+ regulation in skeletal muscle fatigue. Acta Physiol Scand. 2003;179:39–48. doi: 10.1046/j.1365-201X.2003.01169.x. [DOI] [PubMed] [Google Scholar]
- 28.Abbott BC, Bigland B, Ritchie JM. The physiological cost of negative work. J Physiol. 1952;117:380–390. doi: 10.1113/jphysiol.1952.sp004755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iguchi M, Baldwin K, Boeyink C, Engle C, Kehoe M, Ganju A, Messaros AJ, Shields RK. Low frequency fatigue in human quadriceps is fatigue dependent and not task dependent. J Electromyogr Kinesiol. 2008;18:308–316. doi: 10.1016/j.jelekin.2006.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Proske U, Morgan DL. Muscle damage from eccentric exercise: mechanism, mechanical signs, adaptation and clinical applications. J Physiol. 2001;537:333–345. doi: 10.1111/j.1469-7793.2001.00333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Enoka RM, Duchateau J. Muscle fatigue: what, why and how it influences muscle function. J Physiol. 2008;586:11–23. doi: 10.1113/jphysiol.2007.139477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hicks AL, Kent-Braun J, Ditor DS. Sex differences in human skeletal muscle fatigue. Exerc Sport Sci Rev. 2001;29:109–112. doi: 10.1097/00003677-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Wust RC, Morse CI, de Haan A, Jones DA, Degens H. Sex differences in contractile properties and fatigue resistance of human skeletal muscle. Exp Physiol. 2008;93:843–850. doi: 10.1113/expphysiol.2007.041764. [DOI] [PubMed] [Google Scholar]
- 34.Babault N, Pousson M, Ballay Y, Van Hoecke J. Activation of human quadriceps femoris during isometric, concentric, and eccentric contractions. J Appl Physiol. 2001;91:2628–2634. doi: 10.1152/jappl.2001.91.6.2628. [DOI] [PubMed] [Google Scholar]
- 35.de Ruiter CJ, Elzinga MJ, Verdijk PW, van Mechelen W, de Haan A. Changes in force, surface and motor unit EMG during post-exercise development of low frequency fatigue in vastus lateralis muscle. Eur J Appl Physiol. 2005;94:659–669. doi: 10.1007/s00421-005-1356-x. [DOI] [PubMed] [Google Scholar]
- 36.Ratkevicius A, Skurvydas A, Lexell J. Submaximal-exercise-induced impairment of human muscle to develop and maintain force at low frequencies of electrical stimulation. Eur J Appl Physiol Occup Physiol. 1995;70:294–300. doi: 10.1007/BF00865025. [DOI] [PubMed] [Google Scholar]
- 37.Sargeant AJ, Dolan P. Human muscle function following prolonged eccentric exercise. Eur J Appl Physiol Occup Physiol. 1987;56:704–711. doi: 10.1007/BF00424814. [DOI] [PubMed] [Google Scholar]
- 38.Rassier DE, Tubman LA, MacIntosh BR. Staircase in mammalian muscle without light chain phosphorylation. Braz J Med Biol Res. 1999;32:121–129. doi: 10.1590/s0100-879x1999000100018. [DOI] [PubMed] [Google Scholar]
- 39.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 40.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2:175–184. [PubMed] [Google Scholar]
- 41.Behm DG, St-Pierre DM. Effects of fatigue duration and muscle type on voluntary and evoked contractile properties. J Appl Physiol. 1997;82:1654–1661. doi: 10.1152/jappl.1997.82.5.1654. [DOI] [PubMed] [Google Scholar]
- 42.Gandevia SC, Allen GM, Butler JE, Taylor JL. Supraspinal factors in human muscle fatigue: evidence for suboptimal output from the motor cortex. J Physiol. 1996;490 (Pt 2):529–536. doi: 10.1113/jphysiol.1996.sp021164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kufel TJ, Pineda LA, Mador MJ. Comparison of potentiated and unpotentiated twitches as an index of muscle fatigue. Muscle Nerve. 2002;25:438–444. doi: 10.1002/mus.10047. [DOI] [PubMed] [Google Scholar]
- 44.Loscher WN, Nordlund MM. Central fatigue and motor cortical excitability during repeated shortening and lengthening actions. Muscle Nerve. 2002;25:864–872. doi: 10.1002/mus.10124. [DOI] [PubMed] [Google Scholar]
- 45.Binder-Macleod SA, Lee SC. Catchlike property of human muscle during isovelocity movements. J Appl Physiol. 1996;80:2051–2059. doi: 10.1152/jappl.1996.80.6.2051. [DOI] [PubMed] [Google Scholar]
- 46.Prasartwuth O, Taylor JL, Gandevia SC. Maximal force, voluntary activation and muscle soreness after eccentric damage to human elbow flexor muscles. J Physiol. 2005;567:337–348. doi: 10.1113/jphysiol.2005.087767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abraham WM. Factors in delayed muscle soreness. Med Sci Sports. 1977;9:11–20. [PubMed] [Google Scholar]
- 48.Takekura H, Fujinami N, Nishizawa T, Ogasawara H, Kasuga N. Eccentric exercise-induced morphological changes in the membrane systems involved in excitation-contraction coupling in rat skeletal muscle. J Physiol. 2001;533:571–583. doi: 10.1111/j.1469-7793.2001.0571a.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Westerblad H, Allen DG. Recent advances in the understanding of skeletal muscle fatigue. Curr Opin Rheumatol. 2002;14:648–652. doi: 10.1097/00002281-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Morgan DL. New insights into the behavior of muscle during active lengthening. Biophys J. 1990;57:209–221. doi: 10.1016/S0006-3495(90)82524-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Verburg E, Murphy RM, Stephenson DG, Lamb GD. Disruption of excitation-contraction coupling and titin by endogenous Ca2+-activated proteases in toad muscle fibres. J Physiol. 2005;564:775–790. doi: 10.1113/jphysiol.2004.082180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fang Y, Siemionow V, Sahgal V, Xiong F, Yue GH. Distinct brain activation patterns for human maximal voluntary eccentric and concentric muscle actions. Brain Res. 2004;1023:200–212. doi: 10.1016/j.brainres.2004.07.035. [DOI] [PubMed] [Google Scholar]
- 53.Nordlund MM, Thorstensson A, Cresswell AG. Central and peripheral contributions to fatigue in relation to level of activation during repeated maximal voluntary isometric plantar flexions. J Appl Physiol. 2004;96:218–225. doi: 10.1152/japplphysiol.00650.2003. [DOI] [PubMed] [Google Scholar]
- 54.Dudley-Javoroski S, Littmann AE, Iguchi M, Shields RK. Doublet stimulation protocol to minimize musculoskeletal stress during paralyzed quadriceps muscle testing. J Appl Physiol. 2008;104:1574–1582. doi: 10.1152/japplphysiol.00892.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]


