Abstract
Purpose
We have shown previously that oral feeding of green tea polyphenols (GTP) to transgenic adenocarcinoma of the mouse prostate mice in a purely chemopreventive setting significantly inhibits prostate cancer development. To translate this to a human situation, the present study was designed to identify the stage of prostate cancer that is most vulnerable to chemopreventive intervention by GTP.
Experimental Design
GTP infusion (0.1% in drinking water) to transgenic adenocarcinoma of the mouse prostate was initiated at ages representing different stage of the disease: (a) 6 weeks (group 1, normal prostate), (b) 12 weeks (group 2, prostatic intraepithelial neoplasia), (c) 18 weeks (group 3, well-differentiated adenocarcinoma), and (b) 28 weeks (group 4, moderately differentiated adenocarcinoma). At age 32 weeks, subsets of animals were evaluated by magnetic resonance imaging, ultrasound, and prostate weight and for serum insulin-like growth factor (IGF)-I/IGF binding protein-3 and IGF signaling.
Results
Tumor-free survival was extended to 38 weeks (P < 0.001) in group 1, 31 weeks (P < 0.01) in group 2, and 24 weeks (P < 0.05) in group 3 compared with 19 weeks in water-fed controls. Median life expectancy was 68 weeks in group 1, 63 weeks in group 2, 56 weeks in group 3, and 51 weeks in group 4 compared with 42 weeks in the control mice. IGF-I and its downstream targets including phosphatidylinositol 3-kinase, pAkt, and phosphorylated extracellular signal-regulated kinase were significantly inhibited only when intervention was initiated early when prostatic intraepithelial neoplasia lesions were common.
Conclusions
Our studies indicate that chemopreventive potential of GTP decreases with advancing stage of the disease and underscore the need to design appropriate chemoprevention clinical trails.
Among all cancers, prostate cancer is an ideal candidate disease for chemoprevention because it is typically diagnosed in men ages >50 years and has a high latency period (1, 2). Therefore, even a slight delay in the progression of this disease by chemopreventive intervention could result in a substantial reduction in the incidence of the disease and, more importantly, improve the quality of life of the patients (1, 2). Evidences collected from geographic, epidemiologic, and migration studies suggest that frequent consumption of green tea is associated with lower frequencies of prostate cancer in Asian population in general compared with those in western societies (3–7). Laboratory and preclinical animal studies also indicate a protective role of green tea against prostate cancer (reviewed in refs. 8–12).
We have shown previously that oral infusion of a decaffeinated polyphenolic fraction isolated from green tea at a human achievable dose (equivalent to 6 cups of green tea a day) beginning at age 8 weeks significantly inhibits prostate cancer development, progression, and its metastasis and enhances tumor-free and overall survival in the transgenic adenocarcinoma of the mouse prostate (TRAMP) mice (13–15). Initial clinical trials of green tea polyphenols (GTP) involving human prostate cancer patients have produced mixed results. Choan et al. (16) evaluated the efficacy and toxicity of green tea on hormone-refractory prostate cancer. Patients with hormone-refractory prostate cancer were prescribed green tea extract capsules at a dose level of 250 mg twice daily. Although treatment was generally well tolerated, 9 of 15 patients had progressive disease within 2 months of starting therapy and 6 patients developed progressive disease after additional 1 to 4 months of therapy. The study concluded that green tea had minimal clinical activity against hormone-refractory prostate cancer. A phase II trial explored the antineoplastic effects of green tea’s (6 g/d green tea, orally in 6 divided doses) in 42 patients with hormone-refractory prostate cancer (17). Tumor response, defined as a decline (≥50%) in the baseline prostate-specific antigen value, occurred in only 2% of the cohort (95% confidence interval, 1–14%), which was not sustained beyond 2 months. The study suggested that green tea carries limited antineoplastic activity, as defined by a decline in prostate-specific antigen levels, among patients with hormone-refractory prostate cancer (17).
A recent proof-of-principle clinical trial assessed the safety and efficacy of green tea consumption in volunteers with high-grade prostatic intraepithelial neoplasia (HGPIN; ref. 18). Tumor incidence was significantly lower in green tea-treated men compared with placebo-treated men. A 2-year follow-up of patients from the same study indicated that green tea effects were long-lasting (19). This study brought into focus the importance of early intervention with green tea and highlighted the significance of green tea in a purely chemopreventive setting.
We hypothesized that green tea feeding is more effective at early stages of prostate cancer development than at the later stages. This study, therefore, was designed to assess the effectiveness of oral feeding of GTP at defined stages of prostate cancer development and progression in the autochthonous transgenic TRAMP model. Alternatively, this preclinical study was intended to assess the appropriateness of the stage of prostate cancer patients that could benefit from green tea consumption.
Materials and Methods
Materials
Decaffeinated GTP (>95% enriched preparation) was a kind gift from Mitsui Norin and contained epigallocatechin-3-gallate (62%), epicatechin-3-gallate (24%), epigallocatechin (5%), and epicatechin (6%). Antibodies against pAkt and phosphorylated extracellular signal-regulated kinase (ERK) were purchased from Cell Signaling Technology; anti-phosphatidylinositol 3-kinase (PI3K) antibody was purchased from Upstate (now Millipore) and β-actin antibody was from Sigma. Antibodies against insulin-like growth factor (IGF)-I and IGF binding protein (IGFBP)-3 were purchased from Santa Cruz Biotechnology.
Animals
The male and female TRAMP mice developed on a pure C57BL/6 background, heterozygous for the probasin-Tag transgene, were bred and maintained in the Animal Care Facility (School of Medicine and Public Health, University of Wisconsin-Madison). Transgenic males for these studies were routinely obtained as [TRAMP × C57BL/6] F1 or as [TRAMP × C57BL/6] F2 offspring. The identity of transgenic mice was established by the PCR-based DNA screening as described previously (20, 21). All experiments were conducted in accordance with the NIH Guide for the Care and Use of Laboratory Animals and approved by the Institutional Animal Care and Use Committee.
Study design
Throughout the experiment, the animals were housed under standard animal housing conditions and had free access to laboratory chow and drinking fluid ad libitum. Oral feeding of GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease: (a) 6 weeks (group 1), when mice have normal prostate pathology; (b) 12 weeks (group 2), when mice histologically display PIN; (c) 18 weeks (group 3), when severe PIN and well-differentiated adenocarcinoma (WDA) are observed; and (d) 28 weeks (group 4), when mice display moderately differentiated adenocarcinoma (MDA) and metastasis is common. Control groups that received water alone were run in parallel. Freshly prepared solution of GTP in tap water was supplied every Monday, Wednesday, and Friday to experimental animals and the control animals were supplied with only tap water throughout the experiment. This feeding regimen is well tolerated by animals and has been used in mice in many previous studies from this (13–15) and other (22–26) laboratories and is equivalent to an approximate consumption of 4 to 6 cups of green tea a day by an average adult human. Eighteen animals were assigned to each group including the control water-fed group. Animals were monitored biweekly for tumor development by abdominal pelvic palpation and survival. At age 32 weeks, 5 animals from each group were randomly selected and evaluated by magnetic resonance imaging (MRI) and ultrasound. Blood was collected by puncturing the retro-orbital plexus and animals were later killed by cervical dislocation, and the genitourinary apparatus containing the seminal vesicles, urinary bladder, and the prostates were carefully removed. Dorsolateral prostate was carefully dissected under the microscope for further studies. Ten animals from each group were allowed to remain in the protocol for evaluation of overall survival.
MRI
Five animals from each group were randomly selected and monitored for tumor growth by MRI at age 32 weeks. Imaging was done by using a whole-body Varian 4.7T (Magnetic Resonance Systems) horizontal bore imaging/spectroscopy system (7.0 cm i.d.) equipped with isoflurane gas anesthesia system. Tumor volumes were determined by manual image segmentation by manually outlining tumor boundaries in parallel slices separated by 50 μm in the two-dimensional images. The areas of the outlined contours were summed and multiplied by the interslice distance to compute tumor volume.
Ultrasound imaging
Ultrasound imaging was done using the Vevo 770 microimaging system (Visualsonics) with a 30 MHz transducer for three-dimensional image visualization and advanced analysis software. Mice were anesthetized by inhalation of isoflurane with 1% to 3% oxygen and ventral hair was removed using a mild depilatory cream. Mice were placed on a thermostatically controlled heating pad to help maintain mouse body temperature. A water-based ultrasonic gel was applied between the imaging probe transducer and the mouse skin and the abdominal area was imaged. Orientation of the prostate gland on ultrasound was accomplished by visualizing the bladder, which is less echogenic and appears as a dark area.
IGF-I and IGFBP-3 assay
Serum was separated from the whole blood obtained from the retro-orbital venous plexus with heparinized capillary tubes, and IGF-I and IGFBP-3 levels were determined by commercially available ELISA kits (Diagnostic Systems Laboratories) according to the manufacturer’s protocol.
Preparation and analysis of tissue
At the time of sacrifice, the lower genitourinary apparatus, including the bladder, seminal vesicles, and prostate, was removed en bloc. The genitourinary wet weight was recorded to the nearest 0.01 g. The dorsolateral prostate was dissected under a dissecting microscope and weighed.
Immunoblot analysis
The dorsolateral prostate removed from both treated and control groups was homogenized in lysis buffer [50 mmol/L Tris-HCl, 150 mmol/L NaCl, 1 mmol/L EGTA, 1 mmol/L EDTA, 20 mmol/L NaF, 100 mmol/L Na3VO4, 0.5% NP-40, 1% Triton X-100, 1 mmol/L phenylmethylsulfonyl fluoride, 10 μg/mL aprotinin, and 10 μg/mL leupeptin (pH 7.4)] at 4°C to prepare cell lysates. The protein concentration was determined by a commercially available BCA protein estimation kit (Pierce Biotechnology) and following the manufacturer’s protocol. Appropriate amount of protein (25–50 μg) was resolved over 8% to 14% Tris-glycine polyacrylamide gel and then transferred onto the nitrocellulose membrane. The blots were blocked using 5% nonfat dry milk and probed using appropriate primary and horseradish peroxidase-labeled secondary antibodies. The blots were washed and the protein was detected by chemiluminescence using enhanced chemiluminescence kit (Amersham Life Science) followed by autoradiography with XAR-5 film (Amersham Life Science). For every immunoblot, equal loading of protein was confirmed by stripping the blot and reprobing with β-actin antibody.
Histology and immunohistochemical analysis
Sections (4 μm) were cut from paraffin-embedded prostate tissues. Immunostaining was done using specific antibodies with appropriate dilutions and replaced with either normal host serum or block for negative controls followed by staining with appropriate biotin-conjugated secondary antibodies and by incubation with avidin-horseradish peroxidase conjugate. The slides were developed in diaminobenzidine and counterstained with a weak solution of hematoxylin stain. The stained slides were dehydrated and mounted in Permount and visualized on a Zeiss-Axiophot DM HT microscope. Images were captured with an attached camera linked to a computer.
Statistical analysis
Five tumors from each group were randomly selected for all histology and immunohistochemical analyses. Data are expressed as mean with 95% confidence intervals for 5 mice. Statistical significance of differences in all measurements between control and GTP-treated groups was determined by one-way ANOVA followed by Tukey’s post hoc analysis for multiple comparisons. Student’s paired t test was used for pair wise group comparisons, as needed. All statistical tests were two-sided, and P < 0.05 was considered statistically significant. Kaplan-Meier method was used to estimate survival, and differences were analyzed by the log-rank test.
Results
Effect of oral feeding of GTP in TRAMP mice on tumor-free and overall survival
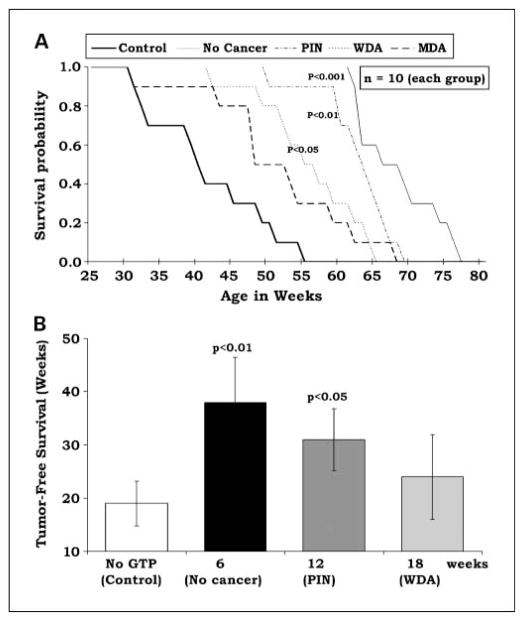
Our earlier studies have shown that oral feeding of GTP when initiated early at age 8 weeks in animals with no prostate abnormality increases tumor-free and overall survival in the TRAMP model (13). The present study was designed to investigate the effect on tumor development when oral GTP feeding was initiated at ages representing different stages of disease progression. In control animals that did not receive GTP, overall survival was 42 weeks (Fig. 1A) and tumor-free survival was 19 weeks (Fig. 1B). When initiated at age 6 weeks, oral GTP extended overall survival to 68 weeks (P < 0.001, no cancer; Fig. 1A) and tumor-free survival to 38 weeks (P < 0.01, no cancer; Fig. 1B). When initiated at age 12 weeks, overall survival was extended to 63 weeks (P < 0.01, PIN; Fig. 1A) and tumor-free survival was extended to 31 weeks (P < 0.05, PIN; Fig. 1B). When oral GTP was initiated at age 18 weeks, overall survival was extended to 56 weeks (P < 0.05, WDA; Fig. 1A) and tumor-free survival was 24 weeks (nonsignificant, WDA; Fig. 1B). When initiated at age 28 weeks, oral GTP did not result in a statistically significant change in overall survival (MDA; Fig. 1A). These data indicate that effective chemopreventive potential of oral GTP decreases when tested in animals with increasing tumor grade. In terms of overall and tumor-free survival, GTP was most effective when given to animals with no cancer or at early stages of PIN development. It was moderately effective when given during the development of adenocarcinoma and least protective when given at advanced stages of tumor development. It is important to mention here that no differences in food or water intake were observed between different groups. Average food intake for each mouse in each group was 2.86 ± 058 g/mouse/d.
Fig. 1.
Effect of oral feeding of GTP on overall and tumor-free survival. Oral GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease as described in the text. A control group that received water alone was run in parallel. A, animals were allowed to remain in the protocol until death to ascertain overall survival by Kaplan-Meier analysis. Survival probability by log-rank test. B, animals were monitored biweekly for tumor development by abdominal pelvic palpation to analyze tumor-free survival. Time in weeks is the start of oral feeding of GTP. Mean ± SD.
Effect of oral feeding of GTP on tumor volume in TRAMP mice as evaluated by MRI
Oral feeding of GTP was initiated in different groups of TRAMP mice as detailed above. When mice reached age 32 weeks, they were evaluated for prostate cancer development and tumor growth by longitudinal MRI analysis. Five animals from each experimental group and the control group were randomly selected and subjected to MRI using a whole-body 4.5 T imager with a custom-built small animal receiver coil. As evident from MRI, at age 32 weeks, the control water-fed TRAMP mice and the GTP-fed mice from MDA group 4 were found to have fully developed tumors that occupied a large part of the abdomen (Fig. 2A). In sharp contrast, TRAMP mice from GTP-fed groups (no cancer, PIN and WDA) had relatively low tumor burden; however, tumor burden increased with delay in chemopreventive intervention with GTP. Using the three-dimensional rendering of prostate tissue/tumors to determine the volume of the tumor in vivo suggested that animals that received GTP at an advanced stage of cancer progression (MDA) did not exhibit significant differences in tumor volumes compared with controls (Fig. 2B).
Fig. 2.
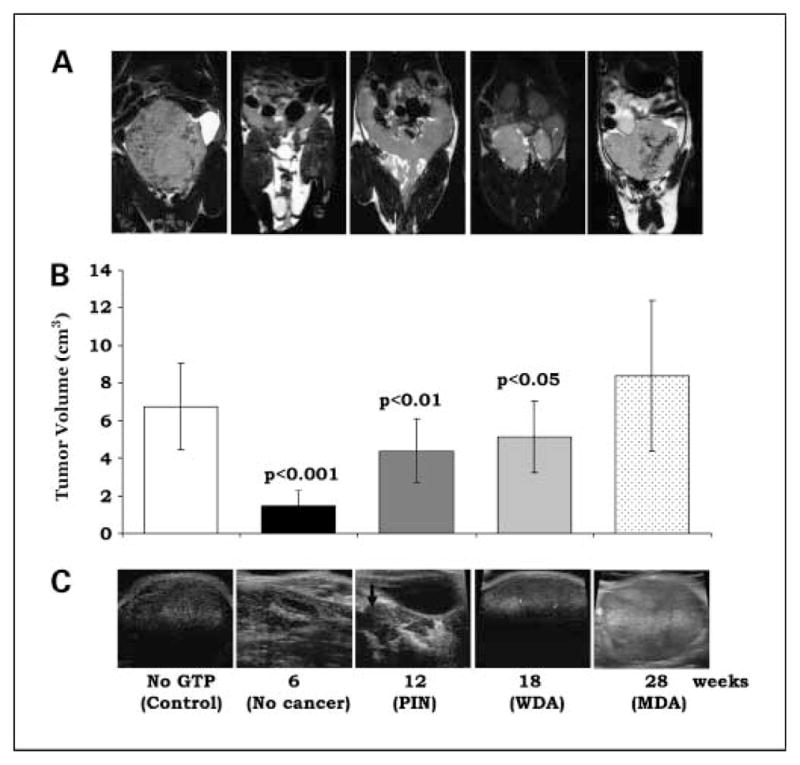
Effect of oral feeding of GTP on prostate cancer development in TRAMP mice. Tumor growth was evaluated by longitudinal MRI analysis and by two- and three-dimensional ultrasound imaging. A, representative MRI of the pelvic region of TRAMP mice at age 32 wk subjected to oral infusion of GTP started at age 6 wk (no cancer), 12 wk (PIN), 18 wk (HGPIN and cancer), and 28 wk (cancer and metastasis). B, mean ± SD tumor volumes in cm3 as evaluated by two-dimensional MRI-based imaging. C, representative ultrasound images of the abdominal region of TRAMP mice subjected to oral infusion of GTP starting at age 6, 12, 18, and 28 wk.
Effect of oral feeding of GTP on prostate cancer development in TRAMP mice evaluated by ultrasound imaging
The Vevo 770 microultrasound is an excellent tool to identify and quantify normal and diseased prostate anatomy in small animal models in vivo in real-time. As seen in Fig. 2B, tumor sizes as visualized at age 32 weeks in control water-fed and experimental GTP-fed mice in groups showed significant differences. No tumors were seen in animals that received GTP when initiated early when no cancer is observed (Fig. 2C, 6 weeks, no cancer). When initiated at PIN stage, a few small tumors could be seen at 32 weeks (Fig. 2C, 12 weeks, PIN). Large tumors were observed in animals where GTP intervention was significantly delayed (Fig. 2C, WDA and MDA).
Effect of oral feeding of GTP on tumor weight in TRAMP mice as evaluated by genitourinary weight
Water-fed control and GTP-fed mice from all experimental were killed at age 32 weeks and the urogenital apparatus containing the seminal vesicles, bladder, and the prostates was removed en bloc and weighed and photographed. Mice from GTP-fed groups (no cancer, PIN and WDA) had significantly lower urogenital apparatus weights compared with the control; however, the degree of inhibition was greater in mice where GTP was initiated very early when no cancer is seen and decreased in groups where GTP was initiated at PIN and WDA stages (Fig. 3A and B). There was no difference in urogenital apparatus weights between control mice and those from the group where GTP was initiated at MDA stage, suggesting lack of tumor growth inhibition at later stages of tumor development.
Fig. 3.
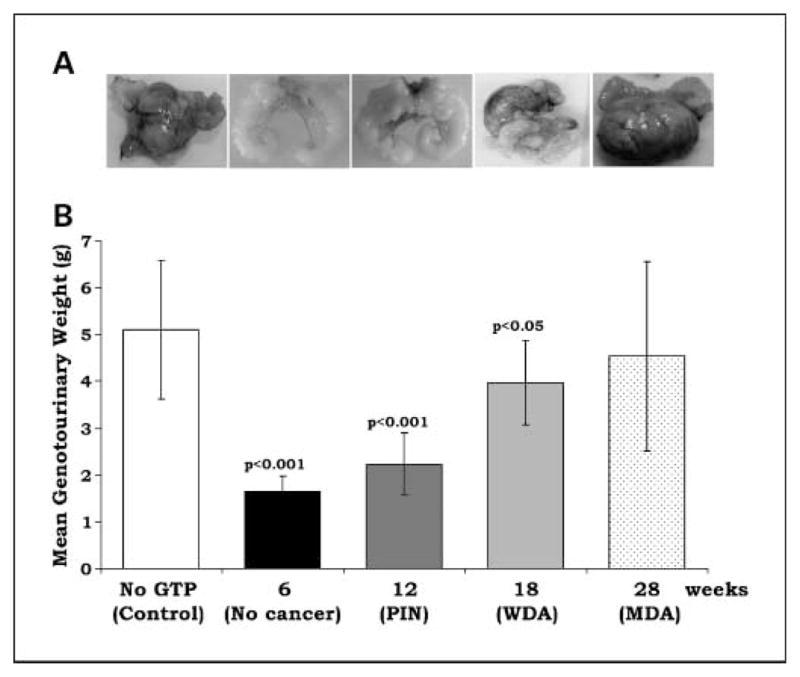
Effect of oral feeding of GTP in TRAMP on genitourinary apparatus weight recorded at age 32 weeks. Oral GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease as described in the text. At age 32 weeks, animals from each group were evaluated for genitourinary weight. A, representative images of the genitourinary apparatus of TRAMP mice subjected to oral infusion of GTP starting at (no cancer), age 12 weeks (PIN), 18 weeks (HGPIN and cancer), and 28 weeks (cancer and metastasis).
B, mean ± SD genitourinary weight.
Effect of oral feeding of GTP on serum IGF-I and IGFBP-3 levels
We have observed previously an increase in serum IGF-I levels with concomitant decrease in serum IGFBP-3 levels in TRAMP mice during cancer progression (13, 14). Because IGFs are known to be produced locally by most tissues, in which they act in an autocrine or a paracrine manner, we determined serum IGF-I and IGFBP-3 levels in the water-fed control and GTP-fed groups. At age 32 weeks, blood was obtained from mice of each group and serum was separated for estimation of IGF-I and IGFBP-3 levels. We observed that maximum inhibition in serum IGF-I levels was observed in mice belonging to group 1 where chemopreventive intervention with GTP started early at age 6 weeks, when no cancer is observed. With progressive delay in chemopreventive intervention with GTP, there was also decrease in IGF-I inhibition (Fig. 4A). No differences in IGF-I levels were observed between control mice and mice from MDA group where GTP intervention started late when advanced tumors are present and metastasis is common (Fig. 4A). We observed a similar trend when IGFBP-3 levels were monitored. Maximum restoration of IGFBP-3 levels was observed in group where GTP intervention started early and this restoration in IGFBP-3 levels showed a continuous decrease with delay in GTP intervention. No significant differences in IGFBP-3 levels were observed between control mice and those belonging to MDA group (Fig. 4B). These data also suggest that chemopreventive efficacy of green tea decreases with increasing stage of disease progression.
Fig. 4.
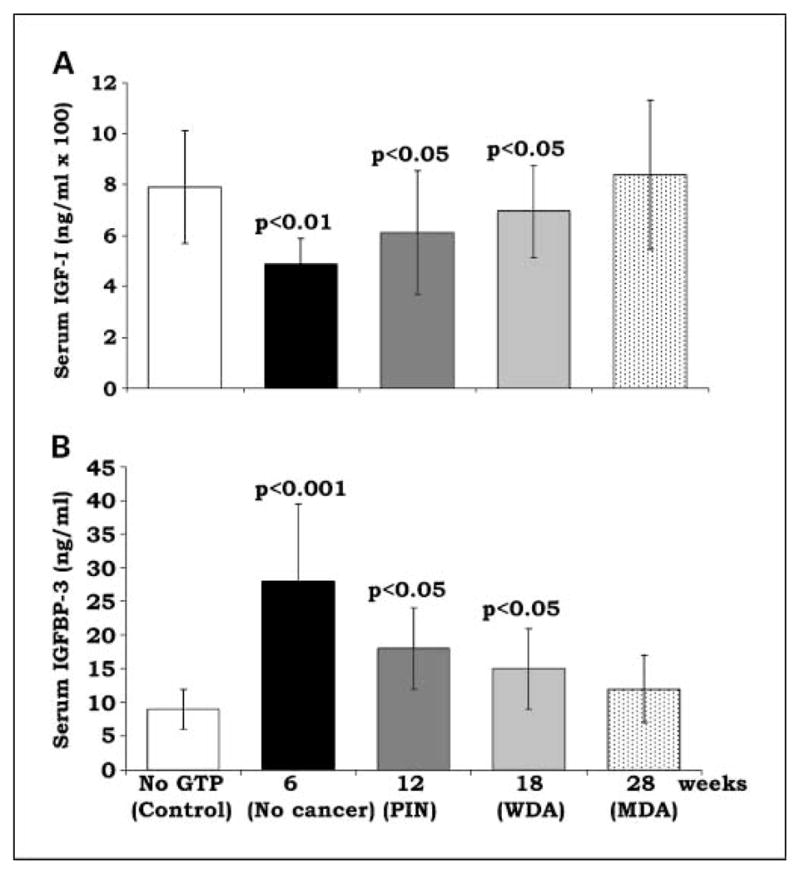
Effect of oral feeding of GTP in TRAMP on serum IGF-I and IGFBP-3 levels. Oral GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease as described in the text. A control group that received water alone was run in parallel. At age 32 wk, blood was collected and serum was separated for (A) IGF-I and (B) IGFBP-3 levels.
Mean ± SD.
Effect of oral GTP feeding to TRAMP mice on IGF-I signaling
Intrinsic induction of IGF-I can trigger multiple signal transduction pathways that include the mitogen-activated protein kinase (ERK) pathway and the PI3K-dependent pathway implicated in the cell survival signals. We therefore analyzed the expression of PI3K, Akt, and ERK1/2 in the dorsolateral prostate/tumors of TRAMP mice from control and experimental groups. We observed that maximum inhibition of PI3K/Akt/ERK was observed in mice belonging to group 1 where chemopreventive intervention with GTP started early at age 6 weeks, when no cancer is observed (Fig. 5A). With progressive delay in chemopreventive intervention with GTP, there was also decrease in inhibition of phosphorylation of PI3K/Akt/ERK (Fig. 5A and B). These data further reinforce and suggest that chemopreventive efficacy of green tea decreases with advancing stage of the disease.
Fig. 5.
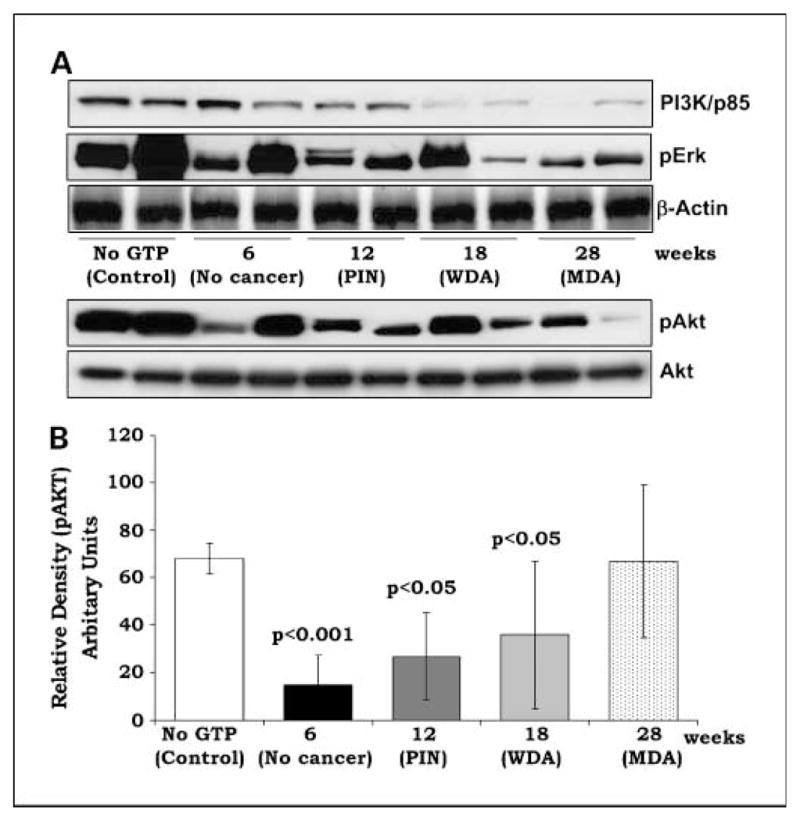
Effect of oral feeding of GTP to TRAMP on downstream IGF signaling. Oral GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease as described in the text. A, at age 32 wk, the dorsolateral prostate was dissected and tissue lysates were prepared and subjected to immunoblotting for PI3K/p85, pAkt, and phosphorylated ERK. Five samples from each group were analyzed by immunoblotting under identical conditions; however, only two representative bands from each are shown. B, bands for pAkt were subjected to densitometric analysis to ascertain quantitatively the change compared with control. Mean ± SD relative density of five bands from each group normalized to whole Akt.
Effect of oral feeding of GTP to TRAMP mice on prostate pathology and tissue IGF-I immunostaining
At age 32 weeks, prostate tissues were processed for routine pathologic analysis by H&E staining. Mice that started GTP feeding at stage with no cancer exhibited mostly normal pathology with sparse areas of early PIN lesions (Fig. 6A, b). Mice from group 2 that started GTP feeding at the stage of PIN lesions exhibited mostly HGPIN lesions with areas of WDA (Fig. 6A, c–d). Mice from group 3, which received oral GTP starting at stages that represented severe hyperplasia and adenocarcinoma, had tumors with areas of WDA to MDA (Fig. 6A, e). Increased IGF-I expression was seen in the tissues of animals belonging to control and the MDA group (Fig. 6B, a and f). Animals in groups where GTP was initiated at 6 and 12 weeks (Fig. 6B, b–d) had significantly low expression of IGF-I in the epithelial cells; however, IGF-I expression was observed in the surrounding stroma (Fig. 6B, b–d). Animals in group WDA where GTP was initiated at later stage also exhibited significantly higher expression of IGF-I (Fig. 6B, e). These observations further suggest that GTP efficacy, when measured in terms of its potential to inhibit IGF-I, decreases with advancing stage of the disease.
Fig. 6.
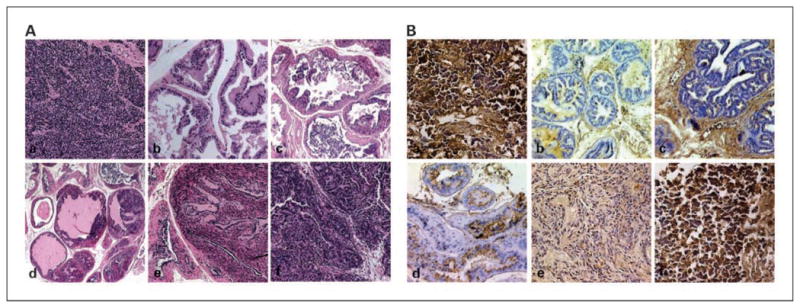
Effect of oral feeding of GTP to TRAMP mice on prostate pathology and IGF-I immunostaining. Oral GTP (0.1% in drinking water ad libitum) was initiated in animals at ages representing different stages of the disease as described in the text. At age 32 wk, the dorsolateral prostate was dissected and subjected to pathologic evaluation by routine H&E staining as described in the text and also subjected to IGF-I expression by immunostaining. A, representative photomicrographs of the prostate tissue from control water-fed TRAMP mouse (a) showing poorly differentiated adenocarcinoma also evident in (f), which received GTP starting at age 28 wk. b to e, sections from different GTP-treated groups showing normal pathology in mice that received GTP starting at 6 wk (b) compared with mice that received GTP starting at12 wk (c and d) showing low-grade PIN to HGPIN lesions and 18 wk (e) showing well to moderate differentiation. Magnification, ×200. B, photomicrographs showing sections from each group stained by immunohistochemistry for IGF-I expression. Control water-fed mice (a) and mice that received GTP starting at age 28 wk (f) show high expression for IGF-I. GTP-treated mice (b–e) show comparatively low expression of IGF-I with the degree of inhibition depending on the stage of GTP intervention.
Discussion
In 2008, prostate cancer is expected to be diagnosed in 186,320 men and to cause 28,660 deaths, making this the most common and second deadliest cancer in U.S. men (27). Prostate cancer progresses slowly through well-defined stages characterized by initial hyperplasia and subsequent development of adenocarcinoma. This slow progression allows a window of opportunity to either stop or delay the progression of the disease. One way to manage prostate cancer is through chemoprevention (1, 2, 9, 28). Because chemopreventive agents are likely to be used chronically by essentially healthy people, naturally occurring and nontoxic dietary substances make ideal candidates assuring safety on long-term use (28). At present, many such agents are being evaluated in preclinical models with the hope that some of these alone or in combination could be recommended for prevention of prostate cancer (1, 29). Among such agents, green tea has shown considerable promise in preclinical models and potentially beneficial effects in some human trials (13–26). In patients with advanced prostate cancer, green tea was found to have limited efficacy (16, 17); however, observations from recent proof-of-principle clinical trial and a 2-year follow-up of patients from the same trial suggest that green tea had exceptionally remarkable effects when given to patients at an early stage of the disease (18, 19). This study assumes much significance because it highlights the implication of early intervention with green tea, which is also consistent with ours (13–15) and other (22–26) studies in purely chemopreventive setting. In addition, epidemiologic studies and geographic observations also indicate a lower incidence of prostate cancer in populations that regularly consume green tea starting at early stage of life (7). In light of these observations, we believe that prevention of early procarcinogenic environment in the prostate is essential for its further development and progression to prostate cancer.
Our data indicate that green tea is more beneficial when intervention is started at an early stage of the disease. We looked at several parameters including overall survival, tumor-free survival, tumor volumes, and genitourinary weight and biochemical parameters such as serum IGF-I and IGFBP-3 levels. All of these data indicated that effective inhibition and delay in the progression of the disease is achieved when GTP intervention is started early. We have observed previously that IGF-I, including its related downstream signaling, is the prime target of GTP-mediated inhibition of prostate carcinogenesis (13, 14). The present study corroborated our previous observations and suggests that inhibition of IGF-I and its downstream activated PI3K/Akt may in fact be necessary for effective prevention of the disease. There is increasing evidence from epidemiologic, experimental, and clinical data suggesting that inhibition of IGF signaling, particularly via the PI3K/Akt-activated pathways, may be a target for chemoprevention (10, 28). IGF levels are increased in many cancers, and levels of IGF-binding protein-3 (which inhibits IGF signaling) are decreased (10, 30, 31). Furthermore, Akt activation in transgenic mice leads to the rapid development of HGPIN (32).
The failure of GTP to effectively inhibit IGF signaling and tumor growth at later stages of the disease in the current study may be related to insufficient GTP to neutralize the circulating IGF-I levels. Because these studies were done only at a dose of 0.1%, which mimics a real-life scenario of 4 of 6 cups of green tea a day, we believe a higher dose of GTP, which may be difficult to achieve through tea feeding, may have made some difference at later stages too. However, higher doses were not studied to offset any associated side effects with the use of GTP (33). Another argument that seems more relevant relates to the role of IGF itself in the TRAMP model. Expression of IGF-I mRNA and serum IGF-I was not increased in androgen-independent disease in the TRAMP model, suggesting that IGF-I is probably more important for early cancer development than in advanced disease (34, 35). In TRAMP, the expression of IGF-I mRNA in the prostate, evaluated on a “per cell” basis, increased with prostate cancer progression and serum IGF-I was also found to be precociously elevated early during cancer progression (34, 35). We also observed that serum IGFBP-3 levels were restored by oral feeding of GTP in the TRAMP. IGFBP-3 is reduced in the serum and prostatic tissue of prostate cancer patients and this decrease in IGFBP-3 may serve to potentiate IGF-I-induced growth. Prostate-specific antigen, often elevated in prostate cancer patients, is a protease that cleaves IGFBP-3 and potentiates IGF-I action in the presence of IGFBP-3 (36). Thus, the observed changes in IGFBP-3 expression may alter IGF ligand bioavailability in prostate cancer (37, 38).
Our findings support the assumption that GTP feeding could be more beneficial to patients diagnosed with early PIN lesions (23). Available data support the conclusion that the presence of PIN on prostate biopsy predicts for an increased risk for prostate cancer and that some PIN lesions give rise to prostate cancer. This approach may also be promising in individuals (a) at high-risk for developing prostate cancer, (b) with HGPIN, and (c) under watchful waiting with low-grade cancer.
The AACR Task Force on Cancer Chemoprevention advocates that when a diagnosis of HGPIN is combined with other risk factors, such as serum prostate-specific antigen, age, race, and/or family history, cohorts of men at very high risk for developing prostate cancer are identified who have prostate cancer incidence rates of 40% over 3 years and 80% over 10 years (28). Also, prostate cancer incidence can be estimated in cohorts of patients with HGPIN, prostate-specific antigen abnormalities, and other risk factors, allowing phase III placebo-controlled trials that have prostate cancer incidence as the primary endpoint (28). Such trials will evaluate prostate cancer risk reduction and will validate extent of HGPIN as a suitable efficacy endpoint (28). A 30% reduction in prostate cancer incidence in the HGPIN patients who are safely treated with GTP compared with control patients should likely constitute a clinical benefit. In summary, we provide data to support a large clinical trial of green tea for patients with early lesions and at risk for developing prostate cancer and to stop or delay the progression of the disease at its outset.
Translational Relevance.
In this preclinical study our findings support the assumption that green tea feeding could be more beneficial to patients diagnosed with early prostatic intraepithelial neoplasia (PIN) lesions. The AACR Task Force on Cancer Chemoprevention advocates that when a diagnosis of high-grade PIN is combined with other risk factors, such as serum prostate-specific antigen, age, race, and/or family history, cohorts of men at very high risk for developing prostate cancer are identified, who have prostate cancer incidence rates of 40% over 3 years and 80% over 10 years. Green tea intervention could be undertaken by identifying a cohort of such patients that will allow a large phase III placebo-controlled trial that has prostate cancer incidence as the primary endpoint. A 30% reduction in prostate cancer incidence in the high-grade PIN patients who are safely treated with green tea compared with control patients should likely constitute a clinical benefit.
Acknowledgments
Grant support: USPHS grants RO1 CA 7 8809, RO1 CA 101039, and RO1 CA 120451and O’Brien Center grant P50 DK065303-01 (H. Mukhtar).
We thank Timothy Hacker (Cardiology Unit) for help with ultrasound imaging, Mary Elizabeth Meyerand (Medical Physics, small animal imaging) for assistance with MRI, and June Sowatzke for help with TRAMP breeding and genotyping.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Syed DN, Khan N, Afaq F, Mukhtar H. Chemoprevention of prostate cancer through dietary agents: progress and promise. Cancer Epidemiol Biomarkers Prev. 2007;16:2193–203. doi: 10.1158/1055-9965.EPI-06-0942. [DOI] [PubMed] [Google Scholar]
- 2.Adhami VM, Mukhtar H. Anti-oxidants from green tea and pomegranate for chemoprevention of prostate cancer. Mol Biotechnol. 2007;37:52–7. doi: 10.1007/s12033-007-0047-8. [DOI] [PubMed] [Google Scholar]
- 3.Boyle P, Severi G. Epidemiology of prostate cancer chemoprevention. Eur Urol. 1999;35:370–6. doi: 10.1159/000019911. [DOI] [PubMed] [Google Scholar]
- 4.Hsing AW, Tsao L, Devesa SS. International trends and patterns of prostate cancer incidence and mortality. Int J Cancer. 2000;85:60–7. doi: 10.1002/(sici)1097-0215(20000101)85:1<60::aid-ijc11>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 5.Peto J. Cancer epidemiology in the last century and the next decade. Nature. 2001;411:390–5. doi: 10.1038/35077256. [DOI] [PubMed] [Google Scholar]
- 6.Angwafo FF. Migration and prostate cancer: an international perspective. J Natl Med Assoc. 1998;90:S720–3. [PMC free article] [PubMed] [Google Scholar]
- 7.Jian L, Xie LP, Lee AH, Binns CW. Protective effect of green tea against prostate cancer: a case-control study in southeast China. Int J Cancer. 2004;108:130–5. doi: 10.1002/ijc.11550. [DOI] [PubMed] [Google Scholar]
- 8.Khan N, Mukhtar H. Tea polyphenols for health promotion. Life Sci. 2007;81:519–33. doi: 10.1016/j.lfs.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siddiqui IA, Afaq F, Adhami VM, Mukhtar H. Prevention of prostate cancer through custom tailoring of chemopreventive regimen. Chem Biol Interact. 2008;171:122–32. doi: 10.1016/j.cbi.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Adhami VM, Afaq F, Mukhtar H. Insulin-like growth factor-I axis as a pathway for cancer chemoprevention. Clin Cancer Res. 2006;12:5611–4. doi: 10.1158/1078-0432.CCR-06-1564. [DOI] [PubMed] [Google Scholar]
- 11.Khan N, Afaq F, Saleem M, Ahmad N, Mukhtar H. Targeting multiple signaling pathways by green tea polyphenol (-)-epigallocatechin-3-gallate. Cancer Res. 2006;66:2500–5. doi: 10.1158/0008-5472.CAN-05-3636. [DOI] [PubMed] [Google Scholar]
- 12.Siddiqui IA, Afaq F, Adhami VM, Ahmad N, Mukhtar H. Antioxidants of the beverage tea in promotion of human health. Antioxid Redox Signal. 2004;6:571–82. doi: 10.1089/152308604773934323. [DOI] [PubMed] [Google Scholar]
- 13.Gupta S, Hastak K, Ahmad N, Lewin JS, Mukhtar H. Inhibition of prostate carcinogenesis in TRAMP mice by oral infusion of green tea polyphenols. Proc Natl Acad Sci U S A. 2001;98:10350–5. doi: 10.1073/pnas.171326098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adhami VM, Siddiqui IA, Ahmad N, Gupta S, Mukhtar H. Oral consumption of green tea polyphenols inhibits insulin-like growth factor-I-induced signaling in an autochthonous mouse model of prostate cancer. Cancer Res. 2004;64:8715–22. doi: 10.1158/0008-5472.CAN-04-2840. [DOI] [PubMed] [Google Scholar]
- 15.Siddiqui IA, Shukla Y, Adhami VM, et al. Suppression of NFκB and its regulated gene products by oral administration of green tea polyphenols in an autochthonous mouse prostate cancer model. Pharm Res. 2008;25:2135–42. doi: 10.1007/s11095-008-9553-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choan E, Segal R, Jonker D, et al. A prospective clinical trial of green tea for hormone refractory prostate cancer: an evaluation of the complementary/alternative therapy approach. Urol Oncol. 2005;23:108–13. doi: 10.1016/j.urolonc.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 17.Jatoi A, Ellison N, Burch PA, et al. A phase II trial of green tea in the treatment of patients with androgen independent metastatic prostate carcinoma. Cancer. 2003;7:1442–6. doi: 10.1002/cncr.11200. [DOI] [PubMed] [Google Scholar]
- 18.Bettuzzi S, Brausi M, Rizzi F, Castagnetti G, Peracchia G, Corti A. Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer Res. 2006;66:1234–40. doi: 10.1158/0008-5472.CAN-05-1145. [DOI] [PubMed] [Google Scholar]
- 19.Brausi M, Rizzi F, Bettuzzi S. chemoprevention of human prostate cancer by green tea catechins: two years later. A follow-up update Eur Urol. 2008;54:472–3. doi: 10.1016/j.eururo.2008.03.100. [DOI] [PubMed] [Google Scholar]
- 20.Greenberg NM, DeMayo F, Finegold MJ, et al. Prostate cancer in a transgenic mouse. Proc Natl Acad Sci U S A. 1995;92:3439–43. doi: 10.1073/pnas.92.8.3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenberg NM, DeMayo FJ, Sheppard PC, et al. The rat probasin gene promoter directs hormonally and developmentally regulated expression of a heterologous gene specifically to the prostate in transgenic mice. Mol Endocrinol. 1994;8:230–9. doi: 10.1210/mend.8.2.8170479. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy S, Caporali A, Enkemann S, et al. Green tea catechins suppress the DNA synthesis marker MCM7 in the TRAMP model of prostate cancer. Mol Oncol. 2007;1:196–204. doi: 10.1016/j.molonc.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harper CE, Patel BB, Wang J, Eltoum IA, Lamartiniere CA. Epigallocatechin-3-gallate suppresses early stage, but not late stage prostate cancer in TRAMP mice: mechanisms of action. Prostate. 2007;67:1576–89. doi: 10.1002/pros.20643. [DOI] [PubMed] [Google Scholar]
- 24.Sartor L, Pezzato E, Donà M, et al. Prostate carcinoma and green tea: (−) epigallocatechin-3-gallate inhibits inflammation-triggered MMP-2 activation and invasion in murine TRAMP model. Int J Cancer. 2004;112:823–9. doi: 10.1002/ijc.20496. [DOI] [PubMed] [Google Scholar]
- 25.Caporali A, Davalli P, Astancolle S, et al. The chemopreventive action of catechins in the TRAMP mouse model of prostate carcinogenesis is accompanied by clusterin over-expression. Carcinogenesis. 2004;25:2217–24. doi: 10.1093/carcin/bgh235. [DOI] [PubMed] [Google Scholar]
- 26.Scaltriti M, Belloni L, Caporali A, et al. Molecular classification of green tea catechin-sensitive and green tea catechin-resistant prostate cancer in the TRAMP mice model by quantitative real-time PCR gene profiling. Carcinogenesis. 2006;27:1047–53. doi: 10.1093/carcin/bgi287. [DOI] [PubMed] [Google Scholar]
- 27.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 28.Kelloff GJ, Lippman SM, Dannenberg AJ, et al. Progress in chemoprevention drug development: the promise of molecular biomarkers for prevention of intraepithelial neoplasia and cancer— a plan to move forward. Clin Cancer Res. 2006;12:3661–97. doi: 10.1158/1078-0432.CCR-06-1104. [DOI] [PubMed] [Google Scholar]
- 29.Surh YJ. Cancer chemoprevention with dietary phytochemicals. Nat Rev Cancer. 2003;3:768–80. doi: 10.1038/nrc1189. [DOI] [PubMed] [Google Scholar]
- 30.Chan JM, Stampfer MJ, Ma J, et al. Insulin-like growth factor-I (IGF-I) and IGF binding protein-3 as predictors of advanced-stage prostate cancer. J Natl Cancer Inst. 2002;94:1099–106. doi: 10.1093/jnci/94.14.1099. [DOI] [PubMed] [Google Scholar]
- 31.Kulik G, Klippel A, Weber MJ. Antiapoptotic signalling by the insulin-like growth factor I receptor, phosphatidylinositol 3-kinase, and Akt. Mol Cell Biol. 1997;17:1595–606. doi: 10.1128/mcb.17.3.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Majumder PK, Yeh JJ, George DJ, et al. Prostate intraepithelial neoplasia induced by prostate restricted Akt activation: the MPAKT model. Proc Natl Acad Sci U S A. 2003;100:7841–6. doi: 10.1073/pnas.1232229100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lambert JD, Sang S, Yang CS. Possible controversy over dietary polyphenols: benefits vs risks. Chem Res Toxicol. 2007;20:583–5. doi: 10.1021/tx7000515. [DOI] [PubMed] [Google Scholar]
- 34.Foster BA, Kaplan PJ, Greenberg NM. Peptide growth factors and prostate cancer: new models, new opportunities. Cancer Metastasis Rev. 1998–1999;17:317–24. doi: 10.1023/a:1006162410436. [DOI] [PubMed] [Google Scholar]
- 35.Kaplan PJ, Mohan S, Cohen P, Foster BA, Greenberg NM. The insulin-like growth factor axis and prostate cancer: lessons from the transgenic adenocarcinoma of mouse prostate (TRAMP) model. Cancer Res. 1999;59:2203–9. [PubMed] [Google Scholar]
- 36.Koistinen H, Paju A, Koistinen R, et al. Prostate-specific antigen and other prostate-derived proteases cleave IGFBP-3, but prostate cancer is not associated with proteolytically cleaved circulating IGFBP-3. Prostate. 2002;50:112–8. doi: 10.1002/pros.10039. [DOI] [PubMed] [Google Scholar]
- 37.Neuhouser ML, Schenk J, Song YJ, et al. Insulin-like growth factor-I, insulin-like growth factor binding protein-3 and risk of benign prostate hyperplasia in the prostate cancer prevention trial. Prostate. 2008;68:1477–86. doi: 10.1002/pros.20819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Finne P, Auvinen A, Koistinen H, et al. Insulin-like growth factor I is not a useful marker of prostate cancer in men with elevated levels of prostate-specific antigen. J Clin Endocrinol Metab. 2000;85:2744–7. doi: 10.1210/jcem.85.8.6725. [DOI] [PubMed] [Google Scholar]