Abstract
Objective
Physician practices may adopt and use electronic prescribing (eRx) in response to mandates, incentives, and perceived value of the technology. Yet, for the most part, diffusion has been limited and geographically confined, and even when adopted, use of eRx in many practices has been low. One explanation for this phenomenon is that decision-makers in the practices possess different technological viewpoints (frames) related to eRx and these frames have formed the basis for the adoption decision, expectations about the technology, and patterns of use. In this study eRx technological frames were examined.
Design
Focus groups, direct observation, and semi-structured interviews were conducted with physicians, practice managers, nurses, and other medical staff.
Measurements
Focus groups were observed, taped, transcribed, and analyzed to reveal themes. These themes guided the observational visits and subsequent interviews. A triangulation process was used to confirm the findings.
Results
Seven frames emerged from the qualitative analysis ranging from positive to neutral to negative: (1) eRx as an efficiency and effectiveness enhancing tool; (2) eRx as the harbinger of new practices; (3) eRx as core to the clinical workflow; (4) eRx as an administrative tool; (5) eRx: the artifact; (6) eRx as a necessary evil; and (7) eRx as an unwelcome disruption.
Conclusion
Frames provide a unique perspective within which to explore the adoption and use of eRx and may explain why perceptions of value vary greatly. Some frames facilitate effective use of eRx while others impose barriers. Electronic prescribing can be viewed as a transitional technology on the path to greater digitization at the physician practice level. Understanding the impact of technological frames on the effectiveness of eRx use may provide lessons for the implementation of future health information technology innovations.
Keywords: eRx, electronic prescribing, technological frames, adoption, use
Introduction
Health information technology (HIT) potentially addresses quality and cost concerns plaguing the US healthcare system.1 2 Proponents argue that greater adoption of HIT—Electronic Medical Record (EMR), CPOE (Computerized Physician Order Entry), and related systems—will improve efficiency and safety. Yet, uptake has been slow and effective use rates disappointing. Possibly, care providers do not adopt or effectively use HIT because they simply perceive little value to be gained.3 4
We draw on the concept of ‘technological frames’ to understand the adoption decision and user perceptions of electronic prescribing (eRx). Technological frames are the cognitive structures through which technology users make sense of the nature and role of technology, its use, and the consequences of use.5 6 These perceptions help decision-makers understand what an innovation can do for them7 and can either create barriers to adoption or facilitate effective use. Because frames exist at the level of the individual (but may also be shared across the organization) and are formed on the basis of prior experience and knowledge, specific biases are likely to carry over from one innovation to the next.8 Thus, not only do frames provide individuals with a means of interpreting and adapting to technology, they define users' expectations and bring preconceived notions and potentially unwarranted positive/negative feelings to the adoption and use process.9–11 Using frames allows us to identify contexts where the implementation and effective use of the technology is likely to be more challenging.
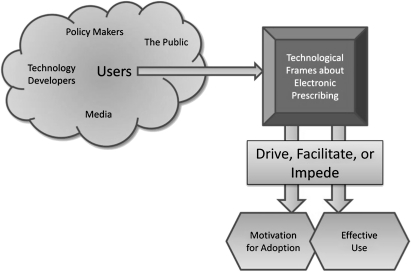
We use the term adoption for the acquisition and implementation of eRx. We define effective use as utilization of eRx in a way that (1) fundamentally displaces a manual or paper-based process, (2) was intended by its designers, and (3) provides the greatest likelihood of delivering on anticipated value objectives.i We note that practices adopt eRx for different reasons, ranging from a desire to improve efficiencies to a response to external mandate. Thus the expectations of users and what benefits they perceive are likely to vary (figure 1).
Figure 1.
The influence on electronic prescribing (eRx) users and technological frames.
Although recent mandates are accelerating adoption of eRx, most research puts ambulatory care practitioner adoption at less than 10%.12 Results have been mixed,13 14 but some studies suggest eRx can address non-clinical inefficiencies, reduce cost through formulary decision-support,15 and improve clinical effectiveness by reducing adverse drug events.16 This variability may in part be due to the technological frames related to eRx and the value proposition assigned to it by the users.
Finally, while several definitions of eRx exist,17 18 an explicit conceptualization is not universally accepted.ii In light of this ambiguity, we sought to understand how these definitions are internalized and resolved by technology users. Thus, our research questions are: (1) What technological frames do individuals have about eRx? (2) How do individuals' frames about eRx influence the manner in which the technology is used? (3) Which frames facilitate effective use of technology and which frames pose obstacles?
Methodology
Study design
We designed and executed a three-stage qualitative study with the intent of obtaining a more grounded understanding of eRx. In the first stage, we conducted four focus groups with members of physician practices: two with groups of physicians and two with groups of office managers (OM) and staff to examine their attitudes towards the technology and patterns of use. By the end of the third session, we were acquiring very little ‘new’ information and appeared to have reached theoretical saturation insofar as novel insights were concerned. Nonetheless, we completed the final session to confirm that we had indeed reached saturation.
The second stage consisted of detailed interviews with adopters and non-adopters of eRx. In this portion of the study, our goal was to delve more deeply into the beliefs and behaviors of the subjects as a means of informing the final stage of the study in which we performed day-long observations at two urban practices, shadowing the clinicians and staff as they interacted with patients, prescribed medications, responded to refill requests, and managed charts (see online appendix OA1 for more details on data collection). The project was approved by institutional review boards at the University of Maryland and Brigham and Women's Hospital.
Analytical approach
To understand variation in the conceptualization of eRx, that is, the frames held by individual users, we used qualitative methodologies 19–22 to analyze focus group and interview transcripts and researchers' notes from the field visits (see table 1). In qualitative research, to reach an appropriate degree of internal validity, multiple sources of data should be used, such as focus groups, direct observation, and interviews.23 We applied a triangulation methodology where data obtained from one collection method were cross-validated with data from the other two methods to identify the full range of conceptualizations that existed.24 We began this process with two of the co-authors and two PhD-trained research assistants experienced with qualitative methods independently reviewing the transcripts of the focus groups. The goal was to immerse oneself in the data and search for patterns or surprising inconsistencies between people/groups while also identifying keywords, topics, and/or themes.25
Table 1.
Stage of research and source and description of data
| Stage of research | ||||||
| 1: Focus groups | 2: Interviews | 3: Site observations | ||||
| Description | Physicians (2 groups) | Office managers (2 groups) | Adopters | Non-adopters | Indiana | Maryland |
| Number and type of participants | 13 MDs 1 Nurse practitioner |
5 OMs 7 Medical assts |
2 OMs | 1 MD | Interviewed/ shadowed: 6 MDs 3 Residents 1 OM 4 Nurses 1 Medical asst |
Interviewed/ shadowed: 4 MDs 3 Nurses 1 OM |
| Number and type of practices represented | 14 Total 5 Internal med 7 Pediatrics 1 Family practice 1 Endocrinology |
7 Total 4 Internal med 1 Pediatrics 1 Family practice 1 Rheumatology |
1 Pediatric (4 MDs, 4 NPs) 1 Family practice (2 MDs) |
1 Family practice (1 MD) |
1 Family medicine residency practice | 1 Pediatric practice |
| Descriptive data and notes | The practice sizes varied from 1 to 79 doctors (mean=6.7; median=2; mode=1; standard deviation=16.9). The population of the cities represented in our sample of practices ranged from 2635 to 67 097 (mean=31 372; median=28 748; standard deviation=19 805) | The pediatric practice was part of a physician-hospital organization (PHO) consisting of three offices | Non-adopter, practicing medicine 40+ years, believes it is too time consuming to learn to use eRx | We collected unstructured observational notes and created workflow diagrams | ||
After receiving input from each of the researchers and following discussions with the other co-authors,26 the research assistants combined all of the newly generated information and created a table that included the themes and representative quotes. Using this table as a reference, the second stage of data collection began in which we interviewed adopters and non-adopters. The initial themes provided a basis for the interviews and site visits; however, we did not specifically direct the conversations toward any of the aforementioned topics or themes. We chose not to formally code our data because we did not want to hold too firmly to our initial classifications. As several qualitative researchers have noted, coding schemes provide a ‘powerful conceptual grid’ that is difficult to escape27 28 and deflects attention away from uncategorized activities. Rather than compiling all of the data from the three sources (focus groups, interviews, site visits) and analyzing it in its entirety after all steps were complete, our approach followed an analytical induction process in which we developed some broad hypotheses prior to beginning the study that were based on assumptions, prior knowledge, and literature.29 Following several iterations between the researchers and assistants we revised our hypotheses—which eventually became the frames—as more data were collected and emerging interpretations were formulated.30 The two co-authors who were not deeply involved with the data analysis then performed additional credibility checks through a process of peer debriefing on the frames extracted during the analysis.31
Results
While conducting the focus group sessions, it became evident that participants' perceptions differed regarding the value of eRx and the concerns they had about it. While many noted the benefits, some perceived the technology to be of limited value and believed that it detracted from, rather than added to the practice of medicine. Following several iterations between the researchers and assistant, we refined the themes and ultimately seven distinct frames about eRx emerged, ranging from positive to neutral to negative (see figure OA1).
We define positive frames as those that create an environment conducive to the effective use of eRx, and negative frames as those that impede effective use of the technology. The three neutral frames represent a continuum of how effectively the technology is being incorporated, from better (core to the workflow) to intermediate (administrative tool) to not so effective (the artifact). Although the frames are not mutually exclusive, we found evidence to suggest that each has unique distinguishing characteristics. In addition, it was not uncommon to find mixed frames within a single practice. In some cases, staff members held very positive frames while the clinicians had negative or neutral frames. In others, the reverse was true.
In the next section we describe each of the frames observed within our study. We have taken great care to validate our themes and avoid ‘anecdotalism’24 by using multiple researchers and data from three different sources. We independently audited each other's interpretations as a means of convincing ourselves and our audience that the findings are genuinely based on a critical investigation of all data and not on a few select data points.32
Positive frames
eRx as an efficiency- and effectiveness-enhancing tool
Efficiency is frequently one of the first effects to be noted when IT is used in place of previously non-automated processes.33 In our observations, eRx was often noted to significantly influence the productivity of the practice in a positive way. Office personnel were discovering valuable new ways to use it and thinking ahead to what features they would like to see in the future. Several people commented that eRx improved both quality and safety (see box 1 for direct quotes from subjects).
Box 1. Efficiency- and effectiveness-enhancing.
“Well when it first started, one of the things was increasing efficiency. The legibility issue. It helps to decrease the patients losing their prescriptions—because that was happening. It helps with reducing the tampering of prescriptions.” (Clinician Focus Group A)
“The patient's happy, the doctor's only clicking, you're only clicking, not having to wait on hold, not having to talk to the pharmacist, not having to leave a message—hoping the pharmacist got it.” (OM Focus Group A)
“Some docs access from home and check drug allergies… can check stuff in off-hours.” (OM Focus Group B)
eRx as the harbinger of new practices
In this frame, people viewed eRx as one component toward the important step of ‘connecting everything together’. The term ‘transition’ was mentioned several times in the context that people viewed eRx as a somewhat simple first step towards adopting more advanced information technologies such as EMRs. They observed that this was going to be the way medical practice would operate in the future. In contexts where such frames exist, the uptake of eRx was significant and there appeared to be few barriers to use. As with the first frame, this frame created an environment where eRx implementation was generally viewed as desirable.
Neutral frames
eRx as core to the clinical workflow
It has been argued that IT is an agent of change, particularly in professional jobs.34 One significant frame that emerged from our analysis suggested that eRx triggered changes in workflow. This pattern is reflected in extensive use of the technology, seamlessly integrated into the practice workflow. Our analysis suggests that the frame is driven by key decision-makers such as a physician-owners or practice managers, and these opinion leaders encourage other doctors and staff to adopt a similar frame (see box 2).
Box 2. Core to the clinical workflow.
“We've changed our workflow dramatically. And the medical secretaries did all the prescriptions… Once we switched to e-prescribing, and it was something that I actually wanted to get out of the hands of the medical secretaries because they are not medically trained, for example, a lot of them didn't come from medical backgrounds or (understand) medical terminology—they've learned it over the years… So nursing does the e-prescribing now. And the way we do ours is ours comes in through EDI… Some [pharmacies] will do it and some don't but we get ours directly from the computer in the pharmacy, so we're not getting as many faxes. So we can pull it up in the morning, see what the prescriptions are, we can have anywhere from 50–100.” (OM Focus Group A)
Actions that emerged as a result of this frame included carrying laptops and personal digital assistants (PDAs) everywhere within the practice: clinicians and staff folded the laptops or left them open and walked with them cradled in the crook of their arm. In several cases, we observed the doctor greeting the patient, then sitting down with the computer at a desk near the patient. While some doctors had the computer opened or immediately opened it on arrival in the room, most did not open it immediately but instead engaged in conversation. After information was received, the doctor used the laptop to enter pertinent information in the chart. After information was documented, in most cases, the doctor engaged in a brief physical exam. While discussing prescriptions with the patient, the doctor altered the script in the exam room with the patient involved in the conversation. The doctor then confirmed the location of the pharmacy of choice and sent the script. Other examples reinforcing the ‘core workflow’ frame were queuing up refill and renewal notices by the medical staff, allowing the treating physician to approve the requests electronically in batches. One medical assistant informally responded “I don't even think about it…I'm really not sure how this office would run without it”; it is important to note that integration into the workflow does not necessarily translate into improvement in processes. In fact, some suggested a somewhat ambivalent view of the changes in workflow. One doctor pulled a paper prescription pad from his coat and stated, “it's still a lot easier and faster to just pull this out and write it up”, yet he was quick to point out the advantages of eRx. While this theme could be regarded to be positive in nature, there were some instances when it was neutral and even negative.
eRx as an administrative tool
Embedded within this frame is the conceptualization of eRx being used primarily by the office staff; physicians are either reluctant to learn or do not believe that it is the best use of their time. As opposed to the example noted above wherein the pharmacy electronically sends renewals and refills to the doctor's office, in this case the medical assistants will consolidate all prescriptions and put them in the doctor's queue, allowing her/him to conduct batched approvals. Interestingly, we noted that both staff and clinicians conceptualized eRx using this frame (see box 3 and OA2.1).
Box 3. Administrative tool.
“…out of the 12 doctors, there's probably 5 of them that won't do any [e]prescribing. Won't even send any prescriptions to the printer. Especially if it's a controlled substance or if the patient is doing mailaway.”
Question from moderator:“So the doctors who were not using it. They're not even using it in a chauffeured manner in the sense that they're telling you or somebody else to go enter it?”
“…they can tell nursing to enter it. But for the most part, they do not. And the medical secretaries don't have access to it. They would probably be more inclined to tell the medical secretaries to do it and less inclined to tell nursing to do it.” (OM Focus Group A)
eRx: the artifact
We found that viewing eRx purely as a device or tool generated specific feelings and influenced use. Further, the form-factor itself elicited strong feelings, with some envisioning eRx as a PDA-based device, while others viewed it as a PC-based software application. The frames varied with respect to individual conceptualizations of the artifact (see box 4).
Box 4. The artifact.
“the instrumentation that we used…was like ‘this big’ <indicating with her hand a screen size about four inches square> and the doctors were like…we're out of here. They wanted no part of it! [laughing from the group]… But since it has evolved to the [laptops/tablet PCs], we're happy about that so that's what (we) do.” (OM Focus Group A)
An interesting dynamic we observed among the individuals participating in the OM focus groups was that they typically mimed an interaction with a keyboard and/or mouse when they conveyed their use of the system. Often we heard phrases like, “we just click, click, click and it's sent” while moving and clicking an invisible mouse. The clinicians, on the other hand, demonstrated their use by either holding the actual PDA device or mimicking their behavior by holding a tiny invisible device in their hand.
There were multiple variations across users from the perspective of this frame. With the administrative staff, we observed two divergent views. Some staff viewed eRx as a ‘tethered’ activity in which their use would be confined to a physical space in the practice. Other staff acknowledged that certain workstations were reserved for eRx (ie, “that's where the medical assistants queue up the scripts”), but they did not limit their view of eRx to a specific location. They did, however, suggest that their use of eRx was limited to interactions with a large-screen terminal found on laptops or desktop PCs. In contrast, clinicians believe the technology to be something more mobile—in some cases a small tablet PC but more often a PDA device—that oftentimes provides the clinician with remote capabilities allowing them to log-in away from the office. In most cases with the clinicians, the frame of reference seemed to suggest a small-screen device. This contrast is notable because it generated opportunities for comments that were specific to the user. For example, clinicians commented on the mobility of the technology (eg, one doctor said his PDA was as much a part of his attire as his stethoscope), but also the annoyance of using a ‘tiny screen’. The staff never commented on small screens but a few nurses mentioned that they ‘sit at the computer’ longer now.
Negative frames
eRx as a necessary evil
The public discourse on HIT in general and eRx in particular has been surrounded by much talk about mandates and incentives to promote use. Thus, it is not surprising that both adopters and non-adopters viewed digitization of healthcare as inevitable. In the case of adopters of eRx, people engaged with the technology because of fiat, mandate, or the desire to receive an incentive for something that they viewed as inevitable. Potential users who had not begun to use eRx experienced significant pressure to adopt, but were often resistant. Illustrative comments included: “We have to do it, but we don't have to like it” (Clinician Interview A); and “This is the way it is all going…whether we like it or not” (Clinician Focus Group A). Overall, users with this frame expressed the sentiment of apathy towards the technology. They may adopt it because they have limited choice in the decision, but their use of it is limited. An office manager described this apathy: “[the eRx package] is up on our computers all day long. But we still use sticky notes and write notes on the chart. No one can believe it.”
eRx as an unwelcome disruption
Health information technology applications have been classified as disruptive innovations.35 36 The adjective ‘disruptive’ is used in prior work to describe technological innovations in two ways. From one perspective, disruptive innovations are typically inferior to the practice or process they replace in the short term, they introduce new performance dimensions to an industry, and their benefits are not immediately evident to the user population37–40 (see box 5). A second perspective asserts that technologies are disruptive as a result of the upheaval they create in established work patterns and routines.36 Our analysis revealed both views of a disruptive technology as prevalent among users: some clinicians and OMs believe that eRx use impedes their work, and they see limited or no value in it (see OA2.2).
Box 5. Unwelcome disruption.
“The problem with all of this (digitization) is that it is so impersonal. It takes all the joy out of practicing medicine. I want to build a relationship with the patient. It isn't all about the medication, they want to share their pain, anxiety, family issues…we can't change the tide…we can't do anything about this…[the move to digital].” (Clinician Interview A)
“Nothing is free” …in response to a query asking whether he would use eRx if it were free. “If it is free, then that means it doesn't work well—otherwise why would they give it away. Plus, later they would make me pay for it.” (Clinician Interview B)
Finally, we encountered an interesting subset of clinicians who had very strong feelings about eRx. We term these clinicians, ‘near-retirement doctors’ who have grandfathered themselves out in that they will retire at the point when eRx becomes fully mandated (see box 6).
Box 6. Unwelcome disruption: Near-retirement.
“I think it is very hard to get the old-school doctors to jump on-board. The doctor I worked for before this pediatrician was 85 before he retired. And there is no way, ever, that you're going to get him to e-prescribe, or medical records, or anything. And I think he retired when he should have because that's the way: you write a prescription, you hand it to the patient, that is it.” (OM Focus Group A)
“…there's really a lot of people in that 5-year plan [referring to his belief that eRx will be mandated within five years]… and there is a lot of people who will not switch over… the truth is, they're biding their time to continue the practice until they retire.” (Clinician Focus Group A)
Table 2 summarizes the technological frames described above, the expectations associated with each, issues that should be considered, and representative quotes from the observations.
Table 2.
Electronic prescribing (eRx) frames, anticipated outcomes, and issues to consider
| Frame | Expectations of value | Issues to consider | Representative quote |
| eRx as an efficiency and effectiveness enhancing tool | Improved productivity Improved safety |
Research needed to conclusively identify if value exists and how to achieve benefits | “Some docs access from home and check drug allergies…can check stuff in off-hours…” |
| eRx as the harbinger of new practices | Practice transformation | Incremental approach to full digitization but can result in HIT resistance if not successful. | eRx is an important step in “connecting everything together…” |
| eRx as core to the clinical workflow | Re-engineered workflow | There may be initial user resistance to change due to new job roles and definitions. May incur costs of retraining | “I don't even think about it…I'm really not sure how this office would run without it” |
| eRx as an administrative tool | Facilitation of staff work | Doctors and staff must have a shared meaning of the use of eRx or conflict and misunderstanding may result | Doctor commented… “that sort of clerical work should be handled by the nurses…” |
| eRx: the artifact | Clinicians: no near term change Staff: more computer time and possibly more mobility in the future |
Users will resist use due to displeasure with current form-factor but this issue may change with time | Doctor said… “PDA is as much a part of my attire as my stethoscope.” Few nurses commented… they ‘sit at the computer longer now’ |
| eRx as a necessary evil | No consequential impact | Over time these users will either become reluctant advocates or will abandon. This is likely not a sustainable position | “This is the way it is all going…whether we like it or not.” |
| eRx as an unwelcome disruption | Increased workload De-personalization of practice |
Designers of hardware/software must strive to build products that streamline and integrate into work processes. Research needs to identify benefits so the value proposition is more tangible | “The problem with all of this (digitization) is that it is so impersonal. It takes all the joy out of practicing medicine. I want to build a relationship with the patient.” |
Discussion
Technological frames reflect how people cognitively construe a technology. These frames can be positive, negative, or neutral, and often materialize at multiple levels within and across individuals.41 42 The frames we identified provide a mechanism for segmenting the population of users to better address the specific barriers they may experience relative to adoption and effective use of eRx and of future HIT innovations. We first underscore the point that different frames can exist in the same practice at any point in time. When all users within a practice hold similar frames, frame congruence is said to exist.7 In such settings, the behavior of the practice toward the target innovation will be driven by this dominant frame. In situations where there is variability in the frames users hold, the cognitions of the key decision-maker (eg, the physician-owner) may drive initial adoption and use behavior. However, it is important to note that even if the key decision-maker holds a positive frame, if other users find the technology to be of little value and/or disruptive, overall effective use will be challenging.
Users who hold a strongly positive frame about eRx expect, and in many instances, experience the productivity enhancements and quality improvements that arise as a result of using eRx. In general, their positive attitude toward and experience with the technology facilitates implementation and effective use. Individuals who hold this frame are willing to spend the time and effort required to learn to use the technology productively. Our data suggest that early use of eRx may help build the confidence and self-efficacy that others have noted as being important for the adoption of any type of advanced technology that requires changes in workflow and common practice.43 44
Holders of neutral frames perceive eRx to be a tool that is useful for facilitating clinical and staff work in the practice, but not necessarily contributing in major ways to improving the quality of healthcare. This stands in distinction to the positive frames, for which holders perceive a potential for eRx to improve efficiency (frame 1) or at least see eRx as a central component in the prescribing process (frame 2). As a consequence, motivating clinicians to adopt and engage in effective use of eRx in such settings may prove to be challenging. Yet, the frames that users of the technology hold will evolve over time with technological developments and greater experience with use.7 For example, with the advent of higher resolution screens, very small devices are now able to transmit images that are much sharper and more readable.
We also discovered frames that view eRx as a necessary evil and an unwelcome disruption. When physicians hold either of these frames, they are resistant to the use of eRx and do not see any value in the technology. It may be the case that these users hold negative views because they see eRx as a transitional technology on the way to even more disruptive technologies that they envision will cause undesirable changes to their work practices. As can be expected, because ‘use’ here is not driven by perceptions of benefits but rather as something that is non-voluntary, this frame engenders the type of use that does not fully exploit all the capabilities of eRx. In such settings, effective use is unlikely to occur because users do not perceive the technology as delivering any value.
Prior research suggests that in group settings, divergent technological frames may result in conflict and various appropriations of the technology that may negatively impact performance.7 Two forms of dissent were present within practices—people who resisted in active ways and those who resisted in passive ways.45 Active resistors not only refused to adopt eRx but they also tried to convince others of the negative consequences of adoption. Passive dissenters took less vocal stances with respect to their actions and feelings related to eRx. As an illustration, some simply opted-out of use by delegating responsibility to subordinates. Others complained about processes that were clearly better than the paper-based alternative but not yet optimal in their minds. In these types of settings, it might be beneficial to reorganize groups or offer more extensive training if users' frames are highly disparate.7 It is important for those who implement technology to realize that once frames are institutionalized, they tend to produce organizational inertia and resistance to change.7
A further interesting discovery was what we have termed ‘misuse’ of eRx. Elements of this phenomenon appeared in multiple frames. For example, a few doctors (and nurses' and OMs' perceptions of their doctors) suggested that eRx could ‘encourage’ unethical and sometimes unlawful behavior. Financial incentives for use were discussed in a number of different contexts. We also encountered a few situations in which nurses, medical assistants, and other staff were given authorization to ‘sign-in’ as the clinician in order to send or approve a prescription. Within the focus groups, these comments were not frequent and were often met with objections from other participants such as, ‘We do not allow that in our practice!’ To the extent that a given individual's frame includes substantial misuse of eRx, their adoption and use of the technology is likely to be less effective than ideal.
The e-HI CIMM report isolates specific benefits of eRx as improved medication safety, enhanced practice efficiency, cost savings, more effective medication management, increased patient adherence, and improved integrity of the prescribing process.46 It is striking that our study showed no evidence of a majority of these benefits as either anticipated or currently being experienced. Although respondents spoke about medication safety and efficiency, the perception of cost savings did not surface. Further, we did not hear any discussion about the effect of eRx on patient adherence. There was some conversation related to its effects on the overall integrity of the prescription process. For example, several noted increased legibility and a very small number alluded to the potential of eRx to reduce tampering. This again suggests that there is a gap between the benefit perceptions of those responsible for diffusing the technology and those responsible for actually using it.
Our study is subject to certain limitations inherent to qualitative research, but we have considered the four areas of rigor or trustworthiness (generalizability, credibility, confirmability, and dependability) for qualitative studies to ensure that we have minimized these limitations.47 48 Additional details are provided in the online appendix (OA3). Analytical induction is less constraining for researchers than a coding scheme, but it can potentially lead to a priori interpretations that are not entirely malleable. We also recognize that additional validation of our frames is necessary.
Conclusion
Our investigation shows that technological frames provide a basis for understanding why some practices adopt eRx rapidly while others continue to resist or delay adoption. When decision makers have no frame on which to base adoption and use decisions (eg, they have little knowledge of the technology and no experience with its use), they will delay or defer the adoption decision until they are able to acquire knowledge about the system.8 When forced to adopt a technology by external mandate, users may actively resist the technology, misuse it, or otherwise not utilize it in the manner intended by its designers. Thus, the gains realized from technology use are likely to be minimal.
Creating an organizational culture that is positively framed may be a precursor to meaningful use. This frame could be accomplished through strong and frequent messaging about the value of eRx that impacts users in a more visceral way than an operational benefit such as improvements in workflow. One suggestion is to post messages (posters, emails, notepads, etc) about the social welfare aspect of using eRx or identify situations in which safety could have been compromised had it not been for eRx. Thus, practice managers must pay attention to insuring that the benefits and relative advantage of eRx over non-automated prescribing are clearly, consistently, and unambiguously communicated and that the possible limitations are acknowledged in a way that reassures prescribers. In addition, technology vendors must continue to seek guidance from users through all phases of development and implementation in order to fully incorporate best practices in workflow, organizational culture, and usability within the IT design to engender positive frames.
Footnotes
Funding: This study was funded by a grant from the Agency for Healthcare Research and Quality, # R18 HS017151-01.
Competing interests: None.
Ethics approval: The project was approved by institutional review boards at the University of Maryland and Brigham and Women's Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
The American Reinvestment and Recovery Act of 2009 has recently introduced the term ‘meaningful use’ in the context of when physicians would be eligible for health IT use incentives. The definition of meaningful use is still evolving. In this study we focus on effective use, as defined in the paper.
The American Health Information Management Association (AHIMA) provides a definition that states: ‘An electronic prescription order/fulfillment route that directly interfaces with physician workstations and mail order or retail pharmacies’.17 The CMS recently published the definition: ‘a prescriber's ability to electronically send an accurate, error-free and understandable prescription directly to a pharmacy from the point-of-care’.18
References
- 1.Pan E, Johnston D, Adler-Milstein J, et al. The Value of Healthcare Information Exchange and Interoperability. Boston, MA: Center for Information Technology Leadership, 2004 [Google Scholar]
- 2.Blumenthal D, DesRoches C, Donelan K, et al. Health Information Technology in the United States: The Information Base for Progress. Boston, MA: Institute for Health Policy, George Washington University Medical Center, and Robert Wood Johnson Foundation, 2006 [Google Scholar]
- 3.Ash JS, Berg M, Coiera E. Some Unintended Consequences of Information Technology in Health Care: The nature of patient care information system related errors. J Am Med Inform Assoc 2004;11:104–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Estabrooks C, O'Leary K, Ricker K, et al. The Internet and Access to Evidence: How are nurses positioned? J Adv Nurs 2003;42:73–81 [DOI] [PubMed] [Google Scholar]
- 5.Gioia DA. Symbols, scripts and sensemaking: Creating meaning in the organizational experience. In: Sims HP, Gioia DA, eds. The thinking organization. San Francisco, CA: Jossey-Bass, 1986:49–74 [Google Scholar]
- 6.Harrison M, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc 2007;14:542–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orlikowski WJ, Gash DC. Technological frames: making sense of information technology in organizations. ACM T Inform Syst 1994;12:174–207 [Google Scholar]
- 8.Murff H, Kannry J. Physician Satisfaction with Two Order Entry Systems. J Am Med Inform Assoc 2001;8:499–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moen A, Brennan PF. HEALTH@HOME: The Work of health information management in the household (HIMH): Implications for consumer health informatics (CHI) innovations. J Am Med Inform Assoc 2005;12:648–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elsbach KD, Barr PS, Hargadon AB. Identifying situated cognition in organizations. Organ Sci 2005;16:422–33 [Google Scholar]
- 11.Chattopadhyay P, Glick WH, Huber GP. Organizational actions in response to threats and opportunities. Acad Manage J 2001;44:937–55 [Google Scholar]
- 12.National Progress Report on E-Prescribing. Washington, DC: SureScripts, 2007 [Google Scholar]
- 13.Gandhi TK, Weingart SN, Seger AC, et al. Outpatient prescribing errors and the impact of computerized prescribing. J Gen Intern Med 2005;20:837–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gandhi T, Weingart S, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med 2003;348:1556–64 [DOI] [PubMed] [Google Scholar]
- 15.Fischer MA, Vogeli C, Stedman M, et al. Effect of Electronic Prescribing With Formulary Decision Support on Medication Use and Cost. Arch Intern Med 2008;168:2433–9 [DOI] [PubMed] [Google Scholar]
- 16.Tierney WM, Miller ME, Overhage JM, et al. Physician Inpatient Order Writing on Microcomputer Workstations: Effects on resource utilization. JAMA 1993;269:379–83 [PubMed] [Google Scholar]
- 17.Electronic prescribing. 2009. http://library.ahima.org/xpedio/groups/public/documents/ahima/bok1_021589.hcsp?dDocName=bok1_021589 (accessed 18 Feb 2009).
- 18.ePrescribing. 2009. http://www.cms.hhs.gov/eprescribing/ (accessed 1 Mar 2009).
- 19.Friedman CP, Wyatt JC. Subjectivist approaches to evaluations. In: Friedman CP, Wyatt JC, eds. Evaluation methods in medical informatics. New York: Springer-Verlag, 1997:205–21 [Google Scholar]
- 20.Morgan DL. Focus groups as qualitative research. 2nd edn Thousand Oaks, CA: Sage Publications, 1997 [Google Scholar]
- 21.Sofaer S. Qualitative methods: what are they and why use them? Health Serv Res 1999;34(5 Part 2):1101–18 [PMC free article] [PubMed] [Google Scholar]
- 22.Office of Behavioral and Social Sciences Research Qualitative Methods in health research: opportunities and considerations in application and review. Washington, DC: National Institutes of Health, 1999. Report No: 02-5046. [Google Scholar]
- 23.Dubé L, Paré G. Rigor in information systems positivist case research: current practices, trends, and recommendations. MIS Quart 2003;27:597–636 [Google Scholar]
- 24.Silverman D. Interpreting qualitative data: methods for analysing talk, text and interaction. London: Sage, 1993 [Google Scholar]
- 25.Hammersley M, Atkinson P. Ethnography: principle in practice. London: Tavistock, 1983 [Google Scholar]
- 26.Bernard H. Research methods in anthropology: qualitative and quantitative approaches. Walnut Creek, CA: Altamira Press, 2001 [Google Scholar]
- 27.Atkinson P. The ethnography of a medical setting: reading, writing and rhetoric. Qual Health Res 1992;2:451–74 [Google Scholar]
- 28.Weber M. Methodology of the social sciences. New York: Free Press, 1949 [Google Scholar]
- 29.Robinson WS. The logical structure of analytic induction. Am Sociol Rev 1951;16:812–18 [Google Scholar]
- 30.Gilgun J. We shared something special: the moral discourse of incest perpetrators. J Marr Fam 1995;57:265–81 [Google Scholar]
- 31.Tobin G, Begley C. Methodological rigour within a qualitative framework. J Adv Nurs 2004;48:388–96 [DOI] [PubMed] [Google Scholar]
- 32.Fisher B. The revolution in breast cancer surgery: science or anecdotalism? World J Surg 1985;9:655–66 [DOI] [PubMed] [Google Scholar]
- 33.Melville N, Kraemer K, Gurbaxani V. Review: Information technology and organizational performance: An integrative model of IT business value. MIS Quart 2004;28:283–322 [Google Scholar]
- 34.Iacono S, Kling R. Changing office technologies and transformations of clerical jobs: a historical perspective. In: Kraut RE, ed. Technology and the Transformation of White-Collar Work. Hillsdale, NJ: Lawrence Erlbaum, 1987:53–75 [Google Scholar]
- 35.Koch C. Off the chart: CIO Magazine, 2003 [Google Scholar]
- 36.Lapointe L, Rivard S. A multilevel model of resistance to information technology implementation. MIS Quart 2005;29:461–91 [Google Scholar]
- 37.Christensen CM. The innovator's dilemma. Boston, MA: Harvard Business School Press, 1997 [Google Scholar]
- 38.Adner R. When are technologies disruptive? a demand-based view of the emergence of competition. Strategic Manage J 2002;23:667–88 [Google Scholar]
- 39.Debruyne M, Reibstein DJ. Competitor see, competitor do: incumbent entry in new market niches. Mark Sci 2005;24:55–66 Winter. [Google Scholar]
- 40.King A, Tucci CL. Incumbent entry into new market niches: the role of experience and managerial choice in the creation of dynamic capabilities. Manage Sci 2002;48:171–86 [Google Scholar]
- 41.Block L, Keller P. When to accentuate the negative: the effects of perceived efficacy and message framing on intentions to perform a health-related behavior. J Mark Res 1995;32:192–203 [Google Scholar]
- 42.Levin I, Schneider S, Gaeth G. All Frames are not created equal: a typology and critical analysis of framing effects. Organ Behav Hum Decis Process 1998;76:149–88 [DOI] [PubMed] [Google Scholar]
- 43.Brown SH, Coney RD. Changes in physicians' computer anxiety and attitudes related to clinical information system use. J Am Med Inform Assoc 1994;1:381–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Larum H, Ellingsen G, Faxvaag A. Doctors' use of electronic medical records systems in hospitals: cross sectional survey. BMJ 2001;323:1344–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marakas G, Hornik S. Passive resistance misuse: overt support and covert recalcitrance in IS implementation. Eur J Inform Syst 1996;5:208–19 [Google Scholar]
- 46.Electronic Prescribing Becoming Mainstream Practice A collaborative report from the eHealth Initiative and the Center for Improving Medication Management. Washington, DC and Alexandria, VA: eHI and CIMM, 2008 [Google Scholar]
- 47.Guba EG. Criteria for assessing the trustworthiness of naturalistic inquiries. Educ Commun Technol J 1981;29:75–91 [Google Scholar]
- 48.Guba EG, Lincoln YS. Fourth Generation Evaluation. Newbury Park, CA: Sage, 1989 [Google Scholar]