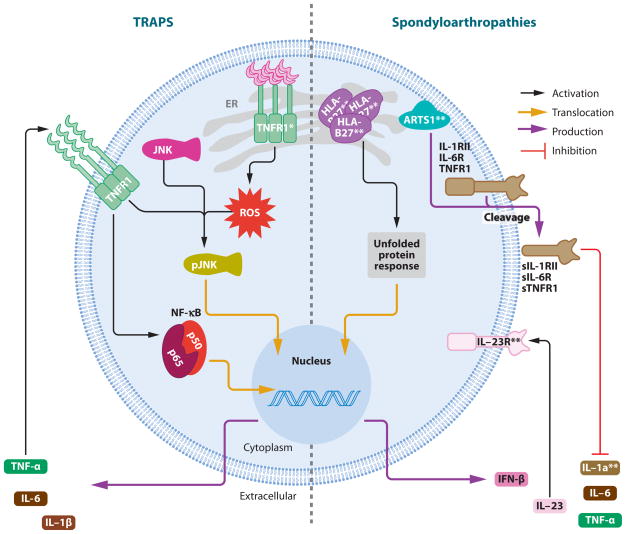
Figure 4.
Mechanisms of autoinflammatory protein folding disorders. Left: TNF-receptor associated periodic syndrome (TRAPS). TNF-receptor type 1 (TNFR1) accumulates in the endoplasmic reticulum (ER) when mutated (indicated by asterisk). This accumulation leads to increased reactive oxygen species (ROS) activation, and subsequent MAPK phosphorylation ( JNK and p38), which makes the cells more susceptible to inflammatory stimuli. TRAPS patients, who are heterozygous for TNFR1 mutations, still carry the wild-type TNFR1, which is thought to play a role in propagating the inflammatory cascade. Right: spondyloarthropathies, ankylosing spondylitis. An HLA-B27 variant is strongly associated with ankylosing spondylitis and may accumulate in the ER, leading to an unfolded protein response. Weaker gene associations include ARTS1 (ER-associated aminopeptidase 1, ERAP1), which could affect the pathogenic presentation of antigenic peptide fragments or the cleavage of membrane bound receptors, and IL-23R/IL-1α, which argue for the role of proinflammatory cytokines in this disease.