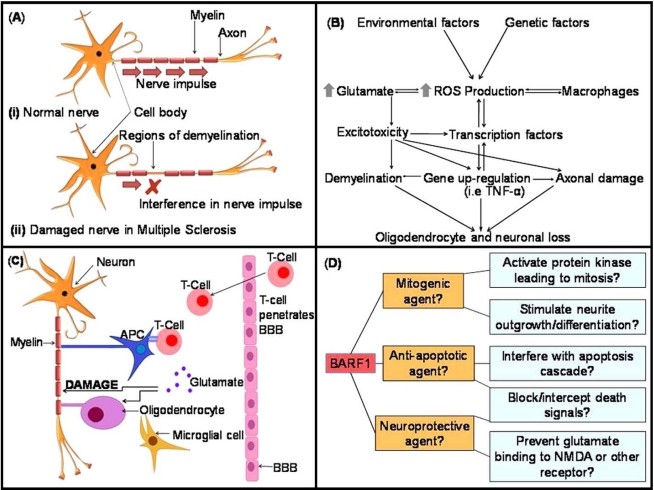
Fig. (1).
(A). Schematic of signal transduction in (i) a normal neuron in a healthy brain, versus (ii) a damaged demyelinated neuron in a patient affected by MS. In MS the immune system attacks the white matter of the brain in a combined insult involving auto-reactive T cells, B cells, macrophages and activated microglia. Inflammation leads to the formation of plaques, followed by the destruction of the protective myelin sheath. Myelin damage leads to impaired signal transduction or blockage, resulting in the clinical symptoms of MS. Removal or damage of the myelin sheath leaves the nerve axon exposed and subject to direct injury [24, 29, 31, 43]. (B). The primary sources of ROS and the cellular occurrences that may lead to oligodendrocyte and neuronal loss in EAE and MS. Modified from ref. [24]. (C). Autoimmune damage causes the supportive astrocytes to be lost or damaged, and repopulation by activated microglia follows. Activated microglia release glutamate, further increasing glutamate levels, which in turn promotes excitotoxic neuronal death by excessive NMDA receptor activation. The activation of T-cells specific against CNS-derived antigens follows. T-cells penetrate the BBB and release further glutamate [29, 39, 40, 45]. APC= Antigen presenting cell. (D). Possible effects of BARF1 protein on cells of the CNS and proposed mechanisms based on previous observations in a variety of cell types.