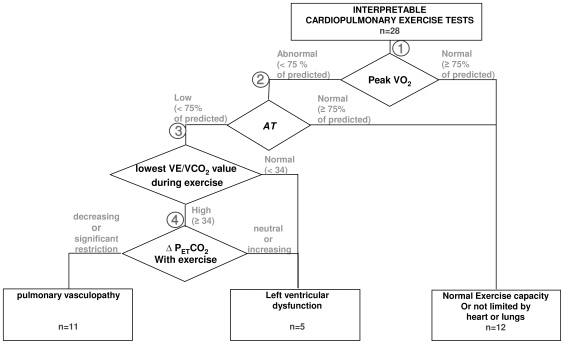
Figure 1. Categorizing referred SSc patients with normal and reduced exercise capacity, using cardiopulmonary exercise testing.
Exercise intolerance was attributed to left ventricular dysfunction or pulmonary vascular disease. Normal is defined as either: a) normal in all cardiovascular and ventilatory aspects of exercise gas exchange, including normal ventilation-perfusion matching and normal peak VO2, or b) reduced peak VO2 with normal AT and no gas exchange abnormalities suggestive of heart, lung or pulmonary vascular disease. Diamonds (branch-points) address specific data: Branch-point 1: Right branch: If the peak VO2 is ≥75% of predicted with normal VE/VCO2 and PETCO2 @ AT and non-ventilatory limitation, the patient is considered to have normal heart and lung function. Left branch includes all with peak VO2 <75%. Branch-point 2: If the AT is normal and ventilation-perfusion matching and lung mechanics are normal (right branch), the patient is considered to be limited by poor effort and not limited by heart or lung disease. If the AT is reduced (left branch), the patient is likely to have left ventricular dysfunction or pulmonary vasculopathy. Branch-point 3: The VE/VCO2 @AT was used to assess matching of ventilation to perfusion. All patients with pulmonary vasculopathy would have ventilation/perfusion mismatching and an elevated VE/VCO2. A cut-off value of ≥34 was selected. If not elevated, they were considered to have left ventricular dysfunction. Branch point 4: PETCO2 usually increases from the beginning of exercise to the AT in patients with normal cardiopulmonary function and patients with left ventricular dysfunction (right branch). However, it usually decreases in patients with pulmonary arterial hypertension (left branch). Nine of the 11 patients classified as pulmonary vasculopathy had a decreasing PETCO2. Two had either no change or increasing PETCO2 from the start of exercise to the AT, possibly due to lung restriction. However, they hyperventilated above their AT. If the patient had moderate to severe restriction and marked decrease in DLCO, this signified interstitial lung disease with pulmonary vasculopathy.