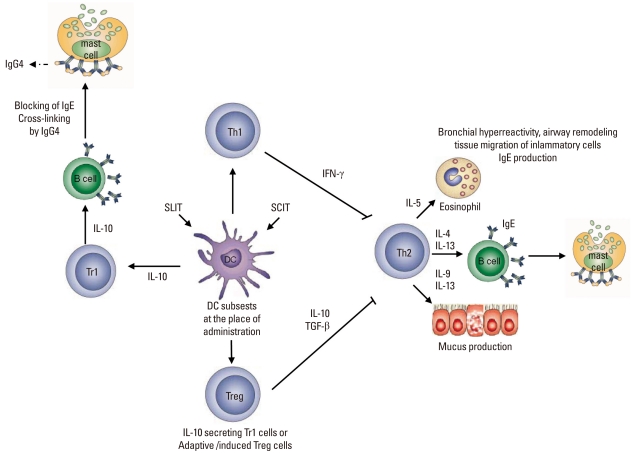
Figure.
Mechanisms of allergen-specific immunotherapy. Both subcutaneous and sublingual SITs first affect the regional antigen-presenting cell, namely the local dendritic cell subset in the place of administration and draining lymph nodes. Although in vivo mechanisms are not clearly known, these dendritic cells induce Treg (CD4+CD25+FoxP3+) cells and Tr1 cells (IL-10+). Treg cells and regulatory cytokines (such as interleukin-10 (IL-10) and transforming growth factor-β, TGFβ) may contribute to the control of allergen-induced immune responses in several different ways. TReg cells utilize multiple suppressor factors to regulate the immune response. IL-10 and TGF-β suppress IgE production and IL-10 induces inflammatory immunoglobulin isotype, IgG4. These two cytokines directly suppress allergic inflammation induced by effector cells such as mast cells, basophils and eosinophils. TReg cells influence the generation of dendritic cells and promote the development of IL-10-producing dendritic cells. In addition, TReg cells inhibit Th2 cells, which can no longer provide cytokines such as IL-3, IL-4, IL-5, and IL-9. These cytokines are required for the differentiation, survival and activity of mast cells, basophils, eosinophils and mucus producing cells, as well as for the tissue homing of Th2 cells. SIT, specific immunotherapy; SLIT, sublingual immunotheraphy; SCIT, subcutaneous immunotheraphy; Treg, T regulatory cells.