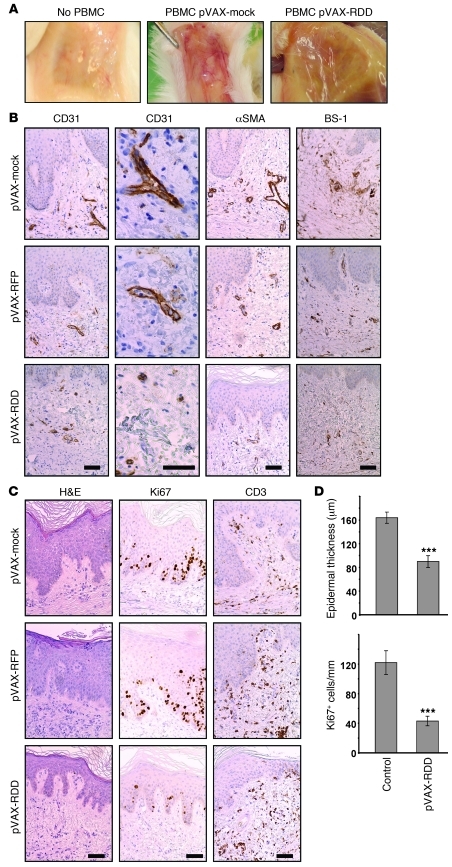
Figure 4. RDD gene therapy prevents the development of psoriasis in the hu/SCID xenotransplantation model.
(A) Uninvolved skin from psoriasis patients was transplanted onto immunodeficient Prkdcscid mice, and recipient mice were injected intraperitoneally with PBS (left panel) or 107 activated PBMCs from the same donors to induce psoriasis (middle and right panels). Two days prior to injection of PBMCs, the mice were subjected to gene therapy with pVAX-mock or pVAX-RDD. The macroscopic aspect of the blood vessels on the underside of the skin transplants demonstrates that gene therapy with RDD markedly reduced cutaneous vascularization. Original magnification, ~×3 (B) Prkdcscid mice were treated as described in A, and the transplanted human skin was analyzed by immunohistochemistry using the indicated reagents detecting blood vessels. Somatic gene therapy with pVAX-RDD, but not that with pVAX-mock or pVAX-RFP, reduces number and size of cutaneous blood vessels of both human (CD31 and αSMA) and murine (BS-1) origin. Scale bar: 50 μm. (C) Human skin transplants from Prkdcscid mice were further analyzed by H&E staining (left panels) and by immunohistochemistry using the indicated antibodies detecting proliferating cells (Ki67) or T cells (CD3). Both the epidermal thickness and the number of proliferating epidermal keratinocytes are reduced in transplants from mice treated by RDD gene therapy. Scale bar: 50 μm. (D) Quantitative morphometric analysis of transplants from Prkdcscid mice. The top graph depicts epidermal thickness as determined by blinded measurements. The bottom graph shows the number of proliferating epidermal cells in mice subjected to RDD gene therapy compared with that of the controls. ***P < 0.001. Values represent mean ± SD.