Abstract
We report a case of Histoplasma capsulatum endocarditis in which Histoplasma antigen assay and fungal blood cultures were negative. The diagnosis was made by microscopic examination and culture of the excised valve. Histoplasma capsulatum should be considered in the differential diagnosis of culture-negative endocarditis in regions where it is endemic and in travelers.
CASE REPORT
The patient, a 59-year-old female living in northeastern Ohio, with a history significant for coronary artery disease, hypertension, bicuspid aortic valve, and aortic stenosis, had an aortic bioprosthetic valve replacement in 2004. In April 2010, she presented to her primary care physician with fever, chills, dry cough, and shortness of breath persisting for 10 days and was prescribed amoxicillin-clavulanate for presumed bronchitis. Her symptoms continued to worsen, and she presented to the emergency room in our institution. On examination, her vital signs were significant for a temperature of 101°F, respiratory rate of 22 breaths/min, heart rate of 105 beats/min, blood pressure of 129/50 mm Hg, and oxygen saturation of 100% on 2 liters nasal cannula supplemental oxygen. The physical exam was remarkable for oral caries and an aortic systolic ejection murmur. There were no peripheral stigmata of infective endocarditis or signs of heart failure. A complete blood count showed a white blood cell count of 8,400 cells/mm3 with 82% neutrophils, hemoglobin of 11.2 g/dl, and a platelet count of 206,000/mm3. Other investigations were remarkable for an erythrocyte sedimentation rate of 108 mm/h (normal, <30 mm/h), C-reactive protein level of 5.96 mg/dl (normal, <0.8 mg/dl), and creatinine level of 1.37 mg/dl. Liver function tests were normal. Chest X ray was normal, but transesophageal echocardiography (TEE) showed a 5- by 6-mm vegetation on the aortic valve with mild aortic regurgitation. Numerous blood cultures, including three fungal cultures using 10-ml Isolator tubes, were negative. The presumptive diagnosis was culture-negative endocarditis associated with recent antibiotic use. Initially, the patient was started on vancomycin, gentamicin, ceftriaxone, and rifampin. Subsequently, ceftriaxone was switched to meropenem due to the concern for drug fever. Despite antibiotic therapy, the patient continued to have persistent fevers and rigors. A magnetic resonance image (MRI) of the brain and a computed tomography (CT) of the abdomen and pelvis did not reveal embolic lesions or abscesses. Fourteen days after the initial TEE, a repeat TEE demonstrated enlargement of the vegetation on the aortic valve with no definite periannular abscess. The patient underwent an aortic valve replacement, during which vegetations were found on all three aortic leaflets. The aortic annulus, left ventricular free wall, and septum were not involved. Direct microscopic examination of the vegetations stained with calcofluor white-KOH disclosed numerous small, oval yeasts. Histopathology of the excised valve showed chronic inflammation consistent with infection of the bioprosthetic valve, with fibrosis and degeneration, and fibrinous vegetations on all three valve leaflets. Nests of small, 3- by 5-μm, oval yeasts were noted in one of the vegetations in sections stained with hematoxylin and eosin, tissue Gram, and Gomori methenamine silver (GMS) stains (Fig. 1). The culture yielded growth of a yeast after 4 days, which was identified after 11 days of incubation as Histoplasma capsulatum based on dimorphic growth and the presence of tuberculate macroconidia in the mold phase. The identity of the culture as H. capsulatum was confirmed by a DNA probe performed by the Fungus Testing Laboratory, University of Texas, San Antonio. Subsequent testing of the patient 18 days after surgery showed the presence of H. capsulatum serum antibody, with positive yeast and mycelial phase complement fixation tests at titers of 1:8 and a positive mycelial phase immunodiffusion assay (testing performed by LabCorp, Burlington, NC). However, both urinary and serum antigen tests for H. capsulatum, obtained 6 days after valve replacement, were negative (testing performed by ARUP Laboratories, Salt Lake City, UT). The patient was treated with liposomal amphotericin B, 240 mg per day for 6 weeks following surgery, followed by therapy with oral itraconazole. The patient's postoperative course was complicated by a subdural hematoma necessitating emergency evacuation; however, this was not determined to be embolic in etiology. H. capsulatum was not isolated from the culture of cerebrospinal fluid. The patient was subsequently transferred to a long-term-care facility for rehabilitation and is clinically doing well 8 weeks after her valve replacement.
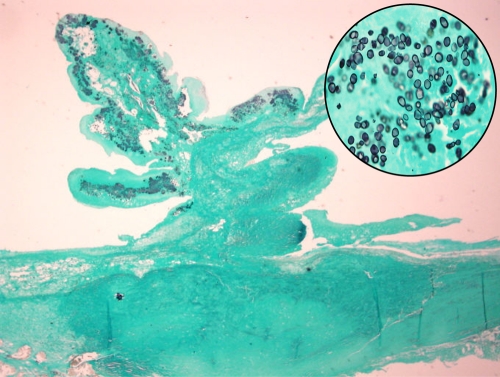
FIG. 1.
GMS stain showing a valve leaflet with vegetation. Original magnification, ×12.5. The inset shows budding yeast forms in the vegetation. Original magnification, ×1,000.
Histoplasma capsulatum exposure is very common in areas where the fungus is endemic, which include the Ohio and Mississippi River valleys, with most infections being asymptomatic (8). Infection is also seen in persons traveling to areas where H. capsulatum is endemic (10). Less than 1% of those infected develop clinical disease, with most of these presenting with pulmonary disease. Endocarditis is a rare manifestation of disseminated disease, with fewer than 50 cases reported (2, 3). Infections have been reported on both native and prosthetic valves. Diagnosis is often delayed because >80% of cases have negative blood cultures, and the lack of a timely diagnosis and appropriate antifungal therapy leads to high mortality (2).
Prior antibiotic therapy is presumed to be the most common reason for culture-negative endocarditis. However, patients with culture-negative endocarditis can have infection caused by uncommon or rare pathogens that do not grow in routinely used blood culture systems. Bartonella species, Coxiella burnetii, and Brucella species have been the most commonly identified bacteria in most series of culture-negative endocarditis caused by fastidious organisms (4, 7). However, the local prevalence of infection with pathogens such as C. burnetii and Brucella spp. varies widely in different geographic locations and epidemiologic settings. On the other hand, infection with H. capsulatum occurs commonly in areas in the Midwestern United States and Central America but rarely manifests as endocarditis. Previously, 44 cases of Histoplasma endocarditis have been reported (2). Most recently, Boland et al. reported three cases of prosthetic valve endocarditis due to Histoplasma in their review of all cases of fungal prosthetic valve endocarditis at the Mayo Clinic from 1970 to 2008 (3). Current guidelines for the management of culture-negative endocarditis do not include evaluation for infection with Histoplasma (1). However, given our case and the review of the literature, H. capsulatum should be considered a pathogen for patients with culture-negative endocarditis, especially in areas where H. capsulatum is endemic and in travelers.
Diagnostic methods for Histoplasma capsulatum infection include serology, culture, histopathology, and antigen detection. An early diagnosis of disseminated histoplasmosis can be considered using antigen assays or serology since material for culture is frequently not available and, when available, growth of H. capsulatum can take up to 4 weeks. Since Histoplasma endocarditis is an endovascular infection, the antigen assay should be useful for the diagnosis of endocarditis. However, both urine and serum antigen assays in our patient, performed shortly after valve replacement, were negative. Urine Histoplasma antigen has been reported to be positive only for one patient with endocarditis (2). In other published case reports of Histoplasma endocarditis, the antigen assay was not performed or reported. While the sensitivity in samples from AIDS patients with disseminated histoplasmosis was 100% in urine and 92.3% in serum, it was reported that further studies are needed to assess the sensitivity in disseminated disease in patients with immunosuppressive disorders other than AIDS or with no underlying immunosuppression (6). Although antigen detection appears to be a sensitive diagnostic method for disseminated histoplasmosis in immunocompromised hosts (9), our case suggests that the antigen test may be negative in immunocompetent patients with Histoplasma endocarditis. One case of Histoplasma endocarditis was diagnosed by a DNA probe applied directly to an excised heart valve that contained abundant yeast forms on microscopic examination (5).
In conclusion, Histoplasma endocarditis is a rare manifestation of disseminated disease, with infections occurring on both native and prosthetic valves. Our case illustrates several of the problems associated with this diagnosis, which is potentially delayed because of negative blood culture and antigen test results, especially in immunocompetent patients. The consideration of infection with H. capsulatum should be included as part of the management of patients with culture-negative endocarditis who reside in or have traveled to regions where Histoplasma is endemic.
Acknowledgments
We have no conflicts of interest and thank Caryn Good Seward for assistance.
Footnotes
Published ahead of print on 6 October 2010.
REFERENCES
- 1.Baddour, L. M., W. R. Wilson, A. S. Bayer, V. G. Fowler, Jr., A. F. Bolger, M. E. Levison, P. Ferrieri, M. A. Gerber, L. Y. Tani, M. H. Gewitz, D. C. Tong, J. M. Steckelberg, R. S. Baltimore, S. T. Shulman, J. C. Burns, D. A. Falace, J. W. Newburger, T. J. Pallasch, M. Takahashi, and K. A. Taubert. 2005. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111:e394-e434. [DOI] [PubMed] [Google Scholar]
- 2.Bhatti, S., L. Vilenski, R. Tight, and R. A. Smego, Jr. 2005. Histoplasma endocarditis: clinical and mycologic features and outcomes. J. Infect. 51:2-9. [DOI] [PubMed] [Google Scholar]
- 3.Boland, J. M., H. H. Chung, F. J. Robberts, W. R. Wilson, J. M. Steckelberg, L. M. Baddour, and D. V. Miller. 6 April 2010. Fungal prosthetic valve endocarditis: Mayo Clinic experience with a clinicopathological analysis. Mycoses. [Epub ahead of print.] doi: 10.1111/j.1439-0507.2010.01884x. [DOI] [PubMed]
- 4.Botelho-Nevers, E., F. Thuny, J. P. Casalta, H. Richet, F. Gouriet, F. Collart, A. Riberi, G. Habib, and D. Raoult. 2009. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch. Intern. Med. 169:1290-1298. [DOI] [PubMed] [Google Scholar]
- 5.Chemaly, R. F., J. W. Tomford, G. S. Hall, M. Sholtis, J. D. Chua, and G. W. Procop. 2001. Rapid diagnosis of Histoplasma capsulatum endocarditis using the AccuProbe on an excised valve. J. Clin. Microbiol. 39:2640-2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Connolly, P. A., M. M. Durkin, A. M. Lemonte, E. J. Hackett, and L. J. Wheat. 2007. Detection of Histoplasma antigen by a quantitative enzyme immunoassay. Clin. Vaccine Immunol. 14:1587-1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fournier, P. E., F. Thuny, H. Richet, H. Lepidi, J. P. Casalta, J. P. Arzouni, M. Maurin, M. Celard, J. L. Mainardi, T. Caus, F. Collart, G. Habib, and D. Raoult. 2010. Comprehensive diagnostic strategy for blood culture-negative endocarditis: a prospective study of 819 new cases. Clin. Infect. Dis. 51:131-140. [DOI] [PubMed] [Google Scholar]
- 8.Kauffman, C. A. 2007. Histoplasmosis: a clinical and laboratory update. Clin. Microbiol. Rev. 20:115-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams, B., M. Fojtasek, P. Connolly-Stringfield, and J. Wheat. 1994. Diagnosis of histoplasmosis by antigen detection during an outbreak in Indianapolis, Ind. Arch. Pathol. Lab. Med. 118:1205-1208. [PubMed] [Google Scholar]
- 10.Wilmshurst, P. T., G. E. Venn, and S. J. Eykyn. 1993. Histoplasma endocarditis on a stenosed aortic valve presenting as dysphagia and weight loss. Br. Heart J. 70:565-567. [DOI] [PMC free article] [PubMed] [Google Scholar]