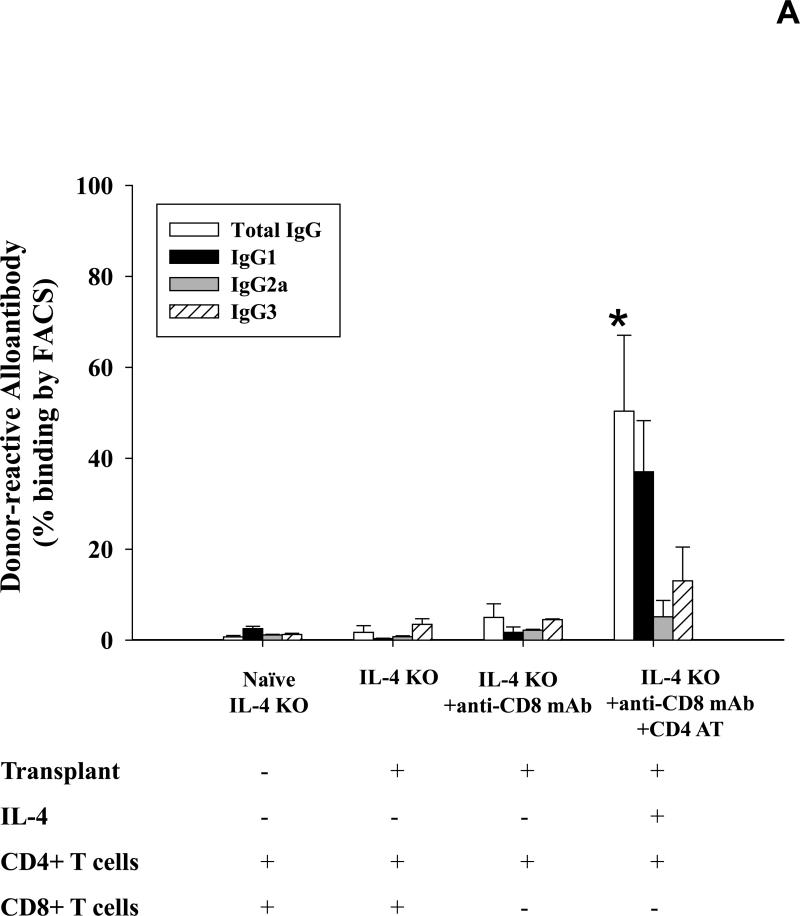
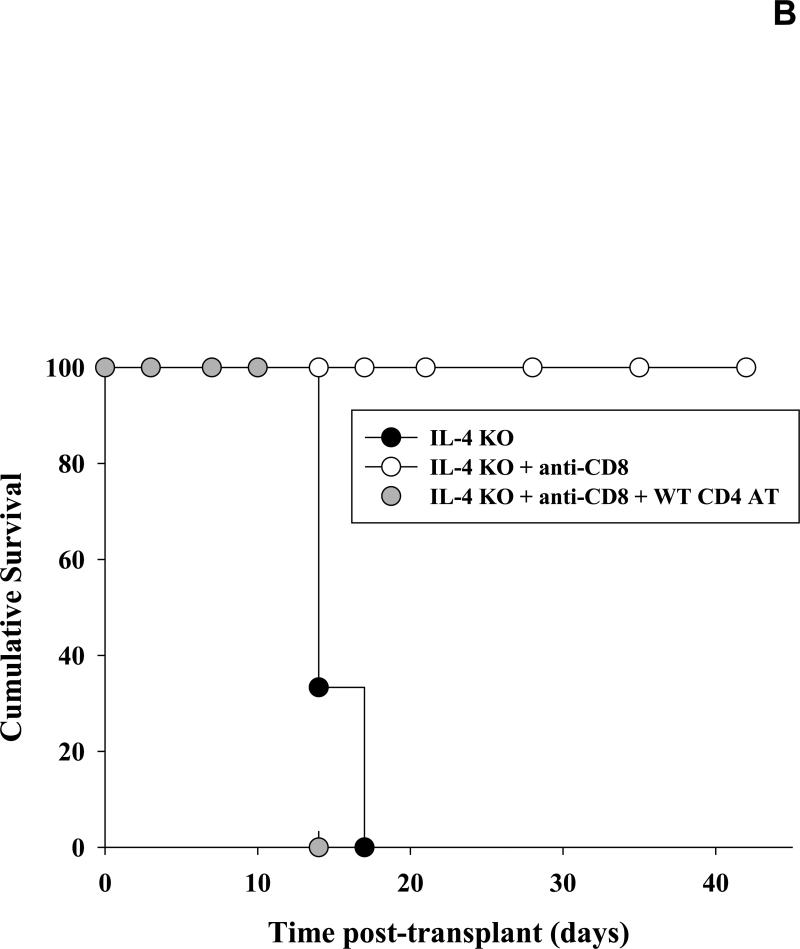
Figure 4. IL-4 producing CD4+ T cells critically regulate production of allospecific antibody post-transplant.
A) Serum from IL-4 KO recipients was collected 14 days following transplantation and analyzed for allospecific IgG alloantibody isotypes IgG1, IgG2a, and IgG3 using flow cytometry. Alloantibody production in IL-4 KO recipients was abrogated (1.7±1.5%, n=6) as compared to wild-type recipient mice (9.7±6.2%; p=0.0025; Figure 1). CD8+ T cell depletion enhanced alloantibody production in IL-4 KO recipients (5.0±3.0%, n=6; p=0.013) but not to the extent that it did in CD8-depleted wild-type recipients (76.2±14.3%; Figure 1). Adoptive transfer of wild type CD4+ T cells (n=5) resulted in significant upregulation of alloantibody production in CD8-depleted IL-4 KO recipient mice (50.4±16.7% vs. 5.0±3.0; p<0.0001, as denoted by “*”). B) To analyze hepatocyte survival, cohorts of IL-4 KO recipient mice were untreated (n=6), CD8-depleted (n=6), or both CD8-depleted and adoptively transferred with 10×106 wild-type CD4+ T cells (n=5). Hepatocyte grafts were monitored for survival by serum hA1AT levels. IL-4 KO recipients that were untreated or were adoptively transferred with wild-type CD4+ T cells (and CD8-depleted) rejected their transplants with median survival time of 14 days. However, IL-4 KO recipients that were only CD8-depleted exhibited significantly enhanced graft survival, with 100% cumulative survival 42 days post-transplant (p<0.0001).