Abstract
The purpose of this study was to compare the incidence of reinfection in patients who received oral antibiotic prophylaxis with those who did not following two-stage revision knee arthroplasty. Additional purposes included: (1) comparison of these findings to the infection rate in patients who underwent revision for aseptic reasons, and (2) characterisation of the organisms responsible for reinfection following revision procedures. Twenty-eight two-stage revision knee arthroplasty procedures were followed up by a mean of 33 days of oral antibiotics (range, 28–43 days), while the remaining 38 procedures received only 24–72 hours of in-patient antibiotics. The incidence of reinfection in each group within 12 months was compared. The reinfection rates were additionally compared to those of 237 patients who underwent revision for aseptic loosening over the same time period. Patients who were treated with postoperative antibiotic prophylaxis had a considerably lower reinfection rate, with one reinfection in the prophylaxis group (4%), compared to six reinfections in the no-prophylaxis group (16%). The reinfection rates remained higher compared to those found in patients who underwent revision knee arthroplasty for aseptic loosening (1 of 237 patients; 0.4%). Both high and low virulence organisms were identified in the patients who were subsequently reinfected. A minimum of 28 days of postoperative oral antibiotics appeared to decrease reinfection rates following two-stage revision knee arthroplasty. These results suggest that the use of oral antibiotic prophylaxis following re-implantation may be appropriate in all patients undergoing two-stage revision, even in the absence of any signs of active infection.
Introduction
Total knee arthroplasty remains one of the most successful procedures in providing marked pain reduction and functional improvement with survivorship consistently reported at greater than 90% at follow-up times of ten to 15 years [3, 17, 24]. However, there are several potential complications associated with the procedure with peri-prosthetic infections among the most devastating. In addition to placing a considerable emotional and economic burden on both patients and surgeons, infections can be difficult to eradicate and may frequently require multiple surgical procedures performed by an experienced orthopaedic surgeon over a period of several months [11, 25]. Knee arthroplasties cured of peri-prosthetic infections can have a lasting negative effect on patients, being associated with poorer postoperative function as compared to total knee arthroplasties with no history of infection [2, 29]. While advances in surgical care such as the use of laminar air flow [19] and adhesive antimicrobial incision drapes [1] have contributed to a reduction in infection rates, the incidence of peri-prosthetic infection following primary total knee arthroplasty remains around 1–2% in the largest reported series [15, 16], rising to over 5% in some cases following aseptic revision procedures [15, 26].
Several strategies have been proposed for the treatment of peri-prosthetic infection following total knee arthroplasty including serial aspirations in combination with parenteral antibiotics, arthroscopic lavage [14, 28], open irrigation and debridement of the joint with retention of components [20], and single-stage component removal followed by irrigation and re-implantation [27]. However, apart from certain cases of acute postoperative or haematogenous infections that can be treated with copious irrigation and liner exchange, a two-stage revision procedure remains the standard of care [8]. The first stage consists of component explantation, joint irrigation and debridement, and placement of a static or dynamic spacer that includes cement laden with a high dose of antibiotics. Some authors have suggested that the use of a dynamic spacer provides better ranges of motion and improves clinical outcomes following re-implantation as compared to non-articulating designs [5, 23]. Patients then undergo several weeks of parenteral antibiotic therapy, which is targeted to the susceptibility profile of the organism responsible or provides broad spectrum empirical coverage if joint cultures are inconclusive [21]. Following this therapy, patients eventually undergo reimplantation if the infection has been cleared based on intra-operative histological negative confirmation of infection. Nevertheless, despite an absence of clinical or histological signs of infection, it is possible that some latent microorganisms remain in the joint at the time of re-implantation, or that the joint can be seeded at the time of the second stage procedure. In addition, patients may be more susceptible to an early new infection in this joint which was previously operated upon multiple times. For this reason, there may be a theoretical benefit to treating patients following re-implantation with a prolonged course of oral antibiotics for prophylaxis against reinfection. However, there is little if any literature evaluating this issue.
The purpose of this study was to compare the reinfection rates following two-stage revision total knee arthroplasty in patients who underwent a minimum of four weeks of prophylactic oral antibiotic therapy to those who received in-hospital perioperative antibiotics only. In addition, the secondary purposes were to compare the reinfection rates in patients who underwent two-stage revision knee arthroplasty to the infection rates in those who received revision arthroplasty for aseptic reasons at the same centre during the same time period, and to describe the organisms responsible for reinfection following the two-stage revision procedures.
Methods
A review of a prospectively-collected database of all arthroplasty procedures performed at a single institution was performed to identify those patients who underwent two-stage revision of a total knee arthroplasty, as well as those who underwent single-stage revision for aseptic reasons and had a minimum of 12 months of follow-up. Any two-stage procedures that underwent a revision for aseptic reasons within 12 months of the reimplantation were excluded. One patient, who was not treated with oral prophylaxis, had a fall that directly caused a full wound dehiscence and was also excluded from the study. Thus, available for analysis were a total of 66 knees in 65 patients who underwent two-stage revision surgery between 2000 and 2008, and who had a mean age of 63 years (range, 40–89 years) at the time of component re-implantation. Of these, 28 knee reimplantations received a minimum of 28 days of postoperative oral antibiotic prophylaxis (mean treatment time of 33 days; range, 28–43 days), while the remaining 38 knee re-implantations received short-term inpatient parenteral antibiotics only (mean 1.3 days; range, one to three days). An additional 237 knees underwent revision of one or more components for aseptic reasons over the same time period at the same centre. Institutional review board approval was obtained for the study of these patients.
Patients suspected of having a periprosthetic infection were evaluated using the Leone and Hanssen criteria [18], with the presence of any one of the following four criteria considered diagnostic for infection: (1) growth of the same organism in two or more cultures obtained from either aspiration of the joint or intraoperative sampling; (2) a finding of acute inflammation on histological evaluation of intraoperative tissue samples (at our institution, defined as ten or more polymorphonuclear cells in a single high power field); (3) gross purulence of the joint observed at the time of surgery; or (4) an actively discharging sinus tracking into the joint. These criteria were used at the time of initial evaluation and operation of a suspected joint infection, as well as at the time of re-implantation and any subsequent evaluation for suspected re-infection.
Intraoperative wound sampling was performed at the time of component removal with specimens sent for culture in an attempt to identify the organism(s) responsible for the infection as well as their antibiotic sensitivities. A custom-made cement spacer was implanted in all patients at the time of component removal, with high-dose antibiotics mixed into the cement to provide sustained local elution between revision stages. Patients were then maintained on parenteral antibiotic therapy for a minimum of six weeks, with the specific therapy based on the advice of an in-hospital infectious diseases consultant. Antibiotic therapy was then withdrawn for a minimum of ten days (range, ten to 32 days), and patients were monitored for clinical signs of recurrent joint infection.
Following parenteral antibiotic therapy, patients returned to the operating room for removal of the cement spacer. A minimum of three tissue samples were taken from different locations at this time, which were examined by frozen section and evaluated for signs of acute inflammation. If present, a new antibiotic-eluting custom cement spacer was implanted, and the decision for further antibiotic therapy was made in consultation with the infectious diseases specialist. If no signs of acute inflammation were found, a new total knee arthroplasty prosthesis was implanted.
Prior to the initiation of this study, the senior surgeon had transferred from another hospital to our institution, where this study was undertaken. At the previous hospital, all patients were treated with six weeks of oral antibiotics following two-stage revision knee arthroplasty as a matter of protocol. At our institution, there were no pre-determined criteria for the use of prophylactic oral antibiotics, and there was no standard protocol in place. A retrospective review of the prospectively-collected database revealed that some patients had been prescribed oral antibiotic prophylaxis on discharge, while others had not.
Patients were monitored following discharge from the hospital for re-infection of the revised total knee arthroplasty, defined as a deep infection of the joint space and/or capsule necessitating a return to the operating room within 12 months of the re-implantation procedure. Superficial wound infections not reaching the capsule, seromas, and haematomas that remained superficial to the capsule were not considered reinfections, as they could be treated with local evacuation and/or debridement not requiring exposure or revision of the prosthesis.
The reinfection rates in the oral prophylaxis and no prophylaxis groups were then determined and compared. The infection rates for both of these groups were then compared to those found in the 237 aseptic knee arthroplasty revisions performed over the same time period. The results of microbiological analysis of wound samples taken at the time of component removal were evaluated in an attempt to determine the profile of the organisms responsible for the periprosthetic infections treated in this study as well as to determine the types of infectious agents present in patients who were subsequently re-infected, and to see if there were any predilections for any specific organisms.
Results
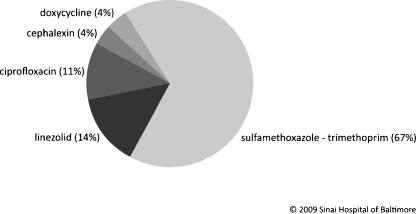
Patients who were treated with oral antibiotic prophylaxis following two-stage revision total knee arthroplasty were less likely to become re-infected as compared to those patients who were treated with short-term in-patient antibiotics only (relative risk = 0.23). Prophylactic oral antibiotics used following component reimplantation are shown in Fig. 1. There was one reinfection among the 28 knees that received oral prophylaxis (4%), as compared to six reinfections in the 38 knees in the no prophylaxis group (16%).
Fig. 1.
Prophylactic oral antibiotics used following component reimplantation
The overall reinfection rate was significantly higher in patients who underwent a two-stage revision procedure when compared to the infection rate in those who had undergone a single-stage revision procedure for aseptic reasons over the same time period (11% compared to 0.4%; relative risk 25.1). The difference in reinfection rates between patients who did not receive oral prophylaxis and those who underwent aseptic revision (16% compared to 0.4%; relative risk 37.4) was markedly higher than the difference between the oral prophylaxis and aseptic revision groups (4% compared to 0.4%; relative risk 7.4).
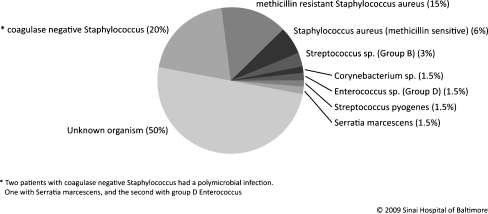
The most common organism responsible for infection was unknown, with no positively identified organism in 50% of cases. The most commonly-identified organisms were coagulase-negative Staphylococcus that was found in 20% of cases (13 of 66 knees), followed by methicillin-resistant Staphylococcus aureus in 15% of cases (10 of 66 knees). A full description of the responsible organisms can be found in Fig. 2.
Fig. 2.
Prevalence of infectious organisms cultured from wound swabs at the time of component removal
A variety of organisms responsible for the original infection was found in patients who were subsequently re-infected. The one patient in the oral prophylaxis group who was subsequently re-infected was found to be infected with methicillin-resistant Staphylococcus aureus at the time of original component removal. In contrast, in the no-prophylaxis group, a variety of organisms were identified in the patients who were subsequently re-infected, including some typically considered to be of low virulence. The specific organisms were: methicillin-resistant Staphylococcus aureus (n = 2), group B Streptococcus (n = 1), methicillin-sensitive Staphylococcus aureus (n = 1), group D Enterococcus (n = 1), and an unknown organism in one case.
Discussion
The senior author spent several years working at an institution where all patients who underwent two-stage revision knee arthroplasty for deep infection were treated with six weeks of oral prophylactic antibiotics following component re-implantation. Subsequently, this surgeon moved to a hospital where no protocol was in place for post-revision oral antibiotic use. On review of a database of all arthroplasty procedures performed at this institution, the authors noticed that some patients had been prescribed a prolonged course of oral antibiotics on discharge, whereas others had not. This observation prompted the authors to undertake this study, to evaluate whether a minimum of 28 days of oral antibiotic prophylaxis reduced re-infection rates following two-stage revision knee arthroplasty. Patients treated with oral prophylaxis may have a considerably lower re-infection rates when compared to those in the non-prophylaxis group. The re-infection rates in both groups were higher than in patients who were revised for aseptic reasons over the same time period. A variety of organisms were found in the re-infected patients.
The authors acknowledge several limitations to this study. First, although the prescription of prophylactic oral antibiotics was done without any pre-determined criteria or protocols, patients were not truly randomised to one of the two groups (oral prophylaxis and no-prophylaxis). Second, this study may be underpowered to detect differences in the incidence of reinfections with a high degree of certainty. Although there were large differences in relative risk of re-infection between the oral prophylaxis group and the no prophylaxis patients (0.23), as well as the aseptic revision group (7.42), a sample size estimation using the proportions of re-infections found in this study (0.04 for the oral prophylaxis group and 0.16 for the no-prophylaxis group) revealed that approximately 130 patients would be required in each group to detect this difference with a power of 0.9 and a p value of 0.05; this is a number of patients that would be difficult to recruit at any one centre. Despite these limitations, the authors believe that this study provides sufficient evidence to suggest that the use of prophylactic oral antibiotics following two stage revision knee arthroplasty reduces reinfection rates even in the absence of any clinical, histological, or microbiological signs of infection at the time of component re-implantation.
Most studies concerning the optimum antibiotic therapy during two-stage revision knee arthroplasty have focussed on the interval between component removal and prosthesis reimplantation. A six week course of parenteral antibiotics following component removal has often been considered the standard of care in North America. Goldman et al. reported a 91% success rate in eradicating infection in 64 infected total knee arthroplasties over a mean follow-up time of 7.5 years (range, two to 17 years) using this protocol [6]. A similar reinfection rate was reported by Windsor et al. following treatment of 38 infected total knees [30]. However, neither of these authors used any antibiotic therapy beyond the immediate postoperative period following re-implantation. Following the widespread adoption of the implantation of high dose antibiotic-eluting spacers at the time of component removal, a few authors have advocated a reduced course of parenteral antibiotics between stages [10], in some cases as short as one postoperative day [12]. In addition, a few authors have recommended the use of oral antibiotics between stages in selected patients, arguing that they are similarly effective while being more convenient and cost-effective for both patients and health care providers [4, 22]. Oussedik et al. reported on the use of an antibiotic-laden cement spacer and oral linezolid following component removal in 12 patients who underwent two stage revision knee arthroplasty. The authors reported resolution of infection in all patients at a mean final follow-up of 32 months (range, 19–47 months) [22]. However, to the best of our knowledge, no studies reported to date have evaluated the efficacy and benefits of postoperative oral antibiotic prophylaxis in reducing reinfection rates.
There are three theoretical benefits to the use of a prolonged course of oral antibiotic prophylaxis following two-stage revision knee arthroplasty. First, despite the absence of any clinical, histological, or microbiological evidence of infection at the time of component reimplantation, it is possible that latent infectious organisms may still be present in the region of a previously active infection. This is supported by several reports of a high incidence of reinfection with the same organism following two-stage revision [6, 7, 9, 13]. Prolonged therapy with oral antibiotics may assist in eradicating any remaining latent organisms and reducing the incidence of same-organism reinfection. Second, while some periprosthetic infections occur as a result of an acute seeding of the joint in either the early postoperative period or through haematogenous dissemination from a distant nidus, the majority of infections are chronic in nature [18]. It is possible that some of these patients have an increased susceptibility to infection or a depressed immune function that impairs their ability to successfully eradicate the invading organisms, which would also place them at a new increased risk of infection following surgical re-implantation of a new knee prosthesis. Finally, several authors have reported that the risk of periprosthetic infection is higher following a revision arthroplasty procedure, as compared to primary implantation [15, 26]. Because prosthesis re-implantation following staged treatment of a periprosthetic infection falls into this higher risk category, more aggressive postoperative antimicrobial therapy may be appropriate in an attempt to reduce the incidence of reinfection. For this reason, patients undergoing two-stage revision knee arthroplasty might benefit from a prolonged course of antibiotics following re-implantation compared to the 24–48 hours of postoperative antibiotic therapy recommended for healthy patients following joint arthroplasty.
In conclusion, the results of this study suggest that the use of a prolonged course of prophylactic oral antibiotic therapy following two-stage revision total knee arthroplasty may reduce the rate of subsequent re-infection. The authors recommend that the use of oral antibiotic prophylaxis should not be limited to patients originally infected with a highly virulent species, as several of the patients in this study were originally infected with a low-virulence organism. Further study should be undertaken to confirm these findings with a larger study group.
Conflict of interest
No external funding was provided in support of this study. The authors certify that they have full control of all primary data and agree to allow the journal to review the data if requested.
References
- 1.Alexander JW, Aerni S, Plettner JP. Development of a safe and effective one-minute preoperative skin preparation. Arch Surg. 1985;120:1357–1361. doi: 10.1001/archsurg.1985.01390360023006. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Engh G, Rorabeck C, Sawhney J, Woolfrey M. Patient satisfaction and outcome after septic versus aseptic revision total knee arthroplasty. J Arthroplasty. 2000;15:990–993. doi: 10.1054/arth.2000.16504. [DOI] [PubMed] [Google Scholar]
- 3.Buechel FF, Sr, Buechel FF, Jr, Pappas MJ, Dalessio J. Twenty-year evaluation of the New Jersey LCS rotating platform knee replacement. J Knee Surg. 2002;15:84–89. [PubMed] [Google Scholar]
- 4.Cordero-Ampuero J, Esteban J, Garcia-Cimbrelo E, Munuera L, Escobar R. Low relapse with oral antibiotics and two-stage exchange for late arthroplasty infections in 40 patients after 2–9 years. Acta Orthop. 2007;78:511–519. doi: 10.1080/17453670710014167. [DOI] [PubMed] [Google Scholar]
- 5.Fehring TK, Odum S, Calton TF, Mason JB (2000) Articulating versus static spacers in revision total knee arthroplasty for sepsis. The Ranawat Award. Clin Orthop Relat Res 380:9–16 [DOI] [PubMed]
- 6.Goldman RT, Scuderi GR, Insall JN (1996) 2-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res 331:118–124 [DOI] [PubMed]
- 7.Haleem AA, Berry DJ, Hanssen AD (2004) Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res 428:35–39 [DOI] [PubMed]
- 8.Hanssen AD, Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999;48:111–122. [PubMed] [Google Scholar]
- 9.Hanssen AD, Trousdale RT, Osmon DR (1995) Patient outcome with reinfection following reimplantation for the infected total knee arthroplasty. Clin Orthop Relat Res 321:55–67 [PubMed]
- 10.Hart WJ, Jones RS. Two-stage revision of infected total knee replacements using articulating cement spacers and short-term antibiotic therapy. J Bone Joint Surg Br. 2006;88:1011–1015. doi: 10.2106/JBJS.E.01077. [DOI] [PubMed] [Google Scholar]
- 11.Hebert CK, Williams RE, Levy RS, Barrack RL (1996) Cost of treating an infected total knee replacement. Clin Orthop Relat Res 331:140–145 [DOI] [PubMed]
- 12.Hoad-Reddick DA, Evans CR, Norman P, Stockley I. Is there a role for extended antibiotic therapy in a two-stage revision of the infected knee arthroplasty? J Bone Joint Surg Br. 2005;87:171–174. doi: 10.1302/0301-620X.87B2.15640. [DOI] [PubMed] [Google Scholar]
- 13.Hofmann AA, Goldberg T, Tanner AM, Kurtin SM (2005) Treatment of infected total knee arthroplasty using an articulating spacer: 2- to 12-year experience. Clin Orthop Relat Res:125–131 [DOI] [PubMed]
- 14.Ilahi OA, Al-Habbal GA, Bocell JR, Tullos HS, Huo MH. Arthroscopic debridement of acute periprosthetic septic arthritis of the knee. Arthroscopy. 2005;21:303–306. doi: 10.1016/j.arthro.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991. doi: 10.1016/j.arth.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J (2009) Prosthetic joint infection risk after TKA in the medicare population. Clin Orthop Relat Res. doi: 10.1007/s11999-009-1013-5 [DOI] [PMC free article] [PubMed]
- 17.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement. A concise follow-up of a previous report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 18.Leone JM, Hanssen AD. Management of infection at the site of a total knee arthroplasty. J Bone Joint Surg Am. 2005;87:2335–2348. doi: 10.2106/00004623-200510000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Lidwell OM, Lowbury EJ, Whyte W, Blowers R, Stanley SJ, Lowe D. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. Br Med J (Clin Res Ed) 1982;285:10–14. doi: 10.1136/bmj.285.6334.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997;12:426–433. doi: 10.1016/S0883-5403(97)90199-6. [DOI] [PubMed] [Google Scholar]
- 21.Nickinson RS, Board TN, Gambhir AK, Porter ML, Kay PR (2009) The microbiology of the infected knee arthroplasty. Int Orthop. doi: 10.1007/s00264-009-0797-y [DOI] [PMC free article] [PubMed]
- 22.Oussedik SI, Haddad FS. The use of linezolid in the treatment of infected total joint arthroplasty. J Arthroplasty. 2008;23:273–278. doi: 10.1016/j.arth.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 23.Park SJ, Song EK, Seon JK, Yoon TR, Park GH (2009) Comparison of static and mobile antibiotic-impregnated cement spacers for the treatment of infected total knee arthroplasty. Int Orthop. doi: 10.1007/s00264-009-0907-x [DOI] [PMC free article] [PubMed]
- 24.Ritter MA, Berend ME, Meding JB, Keating EM, Faris PM, Crites BM (2001) Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop Relat Res 388:51–57 [DOI] [PubMed]
- 25.Sculco TP. The economic impact of infected total joint arthroplasty. Instr Course Lect. 1993;42:349–351. [PubMed] [Google Scholar]
- 26.Sierra RJ, Cooney WPt, Pagnano MW, Trousdale RT, Rand JA (2004) Reoperations after 3200 revision TKAs: rates, etiology, and lessons learned. Clin Orthop Relat Res 425:200–206 [PubMed]
- 27.Silva M, Tharani R, Schmalzried TP (2002) Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res 404:125–131 [DOI] [PubMed]
- 28.Waldman BJ, Hostin E, Mont MA, Hungerford DS. Infected total knee arthroplasty treated by arthroscopic irrigation and debridement. J Arthroplasty. 2000;15:430–436. doi: 10.1054/arth.2000.4637. [DOI] [PubMed] [Google Scholar]
- 29.Wang CJ, Hsieh MC, Huang TW, Wang JW, Chen HS, Liu CY. Clinical outcome and patient satisfaction in aseptic and septic revision total knee arthroplasty. Knee. 2004;11:45–49. doi: 10.1016/S0968-0160(02)00094-7. [DOI] [PubMed] [Google Scholar]
- 30.Windsor RE, Insall JN, Urs WK, Miller DV, Brause BD. Two-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Further follow-up and refinement of indications. J Bone Joint Surg Am. 1990;72:272–278. [PubMed] [Google Scholar]