Abstract
We report on a 23-year-old woman with a right adrenal tumor 13 cm in diameter who was treated by laparoscopy. The patient was asymptomatic, and the tumor was incidentally diagnosed on abdominal ultrasonography. A subsequent computed tomography (CT) of the abdomen confirmed a 12×7×8-cm homogenous mass of the right adrenal. Magnetic resonance imaging (MRI) showed a solid mass measuring 13×7×7.5 cm arising from the right adrenal. Laparoscopic complete excision of the mass was accomplished through a transabdominal lateral approach. The postoperative period was uneventful, and the patient was discharged on the second postoperative day. Histology was consistent with an adrenal ganglioneuroma. Two years later, there is no evidence of recurrence on abdominal CT scan.
Keywords: Ganglioneuroma, Laparoscopic adrenalectomy, Adrenal tumor
INTRODUCTION
Ganglioneuroma (GN) is a rare (0% to 6% of incidentalomas), differentiated, benign, slow-growing tumor that commonly arises from sympathetic ganglion cells and is composed of mature Schwann cells, ganglion cells, and nerve fibres.1,2 The family of tumors originating from ganglion cells includes GN which is a benign lesion, ganglioneuroblastoma which is of intermediate differentiation, and neuroblastoma which is a highly malignant lesion. Neuroblastoma and ganglioneuroblastoma most often occur in infants and children, whereas GN tends to occur in adolescents and young adults.1–3
GNs may arise anywhere along the paravertebral sympathetic plexus and occasionally from the adrenal medulla. Their localization is the retroperitoneal (32% to 52%), mediastinal (39% to 43%), or cervical region (8% to 9%).4–6 Definitive diagnosis is made on histological examination. When such tumors arise from the adrenal medulla, their assessment and management are similar to that of other adrenal tumors. GNs are often asymptomatic even if they are large. Abdominal pain or the palpation of an abdominal mass, or both of these, are among the most common presenting features. Occasionally, symptoms like hypertension, diarrhea, and virilization may develop as a result of mixed hormonally active tumors secreting catecholamines, vasointestinal peptide (VIP), androgens, or all of these.2,7–10 The prognosis is usually excellent, and recurrence is rare after surgical resection.11
The standard treatment suggested for benign adrenal tumors is laparoscopic surgery. At present, relative contraindications to laparoscopic adrenalectomy are a definitive or presumed diagnosis of invasive adrenal cortical carcinoma or circumstances that make a minimally invasive approach technically difficult, such as large tumors.12
We present herein a case of a large, incidentally diagnosed adrenal ganglioneuroma that was removed completely by the laparoscopic approach.
CASE REPORT
A 23-year-old woman was admitted to the endocrine ward of our hospital, for investigation and management of a 13-cm mass arising from the right adrenal. This mass was found incidentally following ultrasonography (US) of the abdomen while the patient was being investigated for oligomenorrhea.
On admission, she was in good health and asymptomatic. She had no past medical history of importance. Blood pressure was within the normal range. On physical examination, a mild discomfort at deep palpation of the right quadrant was found. Radiography of the thorax and an electrocardiogram were normal. Routine blood and urine tests as well as tumor markers showed no abnormality. Endocrinological investigations were within the normal range (Tables 1–3).
Table 1.
General Endocrinology Data
| Normal Range | Case | |
|---|---|---|
| Triiodothyronine (T3) (ng/mL) | 0.58-1.59 | 1.00 |
| Free thyroxine (FT4) (pmol/L) | 9.01-19.05 | 15.3 |
| Thyroid-stimulating hormone (TSH) (μIU/mL) | 0.35-4.94 | 1.006 |
| Anti-thyroid peroxidase autoantibody (Anti-TPO) | <12 | 2.1 |
| Luteinizing Hormone (LH) (mUI/mL) | luteal phase 0.67-23.75 | 7 |
| Follicle Stimulating Hormone (FSH) (mUI/mL) | luteal phase 1.11-13.99 | 7.23 |
| Prolactin (PRL) | 1.2-29.93 | 9.88 |
| Adrenocorticotropic Hormone (ACTH) (pg/mL) | 9-52 | 32.2 |
| 17OPG (ng/mL) | 0.66-4.95 | 1.4 |
| Dehydroepiandrosterone Sulfate (DHEA-S) (ng/mL) | 1950-5070 | 2614 |
| D4-androsterone (ng/mL) | 0.1-3.0 | 2.9 |
| Testosterone (ng/mL) | 0.1-0.8 | 1.1 |
| Aldosterone (pmol/L) | decubitus 22.2-477 standing 83-985 | 456 |
| Renin (μU/mL) | decubitus 5-47 standing 7-76 | 63.6 |
| Parathyroid Hormone (PTH) | 11-62 | 41.3 |
| Urine* (mL/24h) | - | 2310* |
| 4800† | ||
| VMA* (mg/24h) | 1.8-6.7 | 1.8 |
| Metanephrine* (mg/24h) | <1 | 0.36 |
| Adrenaline* (μg/24h) | 1.7-22.4 | 6.4 |
| Noradrenaline* (μg/24h) | 12.1-85.5 | 38.6 |
| Creatinine† (g/24h) | 1-2 | 0.6 |
| Ca/P† (g/24h) | 0.11-0.32/0.41-1 | 0.11/0.4 |
| K/Na* (mEq/24h) | 25-125/40-220 | 120.48/264 |
August 12, 2004.
August 19, 2004.
Table 2.
Synacthen Test (August 12, 2004)
| Normal Range | 0 min | 30 min | 60 min | |
|---|---|---|---|---|
| Cortisol (nmol/L) | morning 138-690 | 486.2 | 1391 | 1636 |
| Aldosterone (pmol/L) | decubitus 22.2-477 | 456 | 537 | 772 |
| standing 83-985 | ||||
| Active Renin (μU/mL) | decubitus 5-47 | 63.6 | - | - |
| standing 7-76 | ||||
| 17OH-PG (ng/mL) | 0.16-3.33 | 1.4 | 4.6 | 5.0 |
| ACTH (pg/mL) | 9-52 | 32.2 | - | - |
Table 3.
Overnight 1 mg Dexamethasone (DEX) Test (August 14, 2004)
| Normal Range | Case | |
|---|---|---|
| Cortisol (nmol/L) | morning 138-690 | <20 |
| Aldosterone (pmol/L) | decubitus 22.2-477 | 79.1 |
| standing 83-985 | ||
| Active Renin (μU/mL) | decubitus 5-47 | 31.2 |
| standing 7-76 | ||
| ACTH (pg/mL) | 9-52 | <5 |
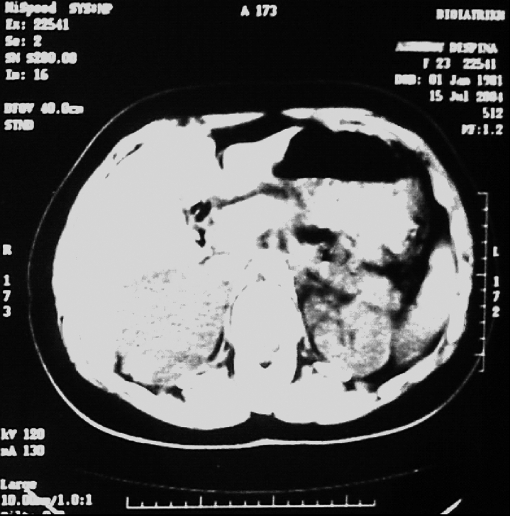
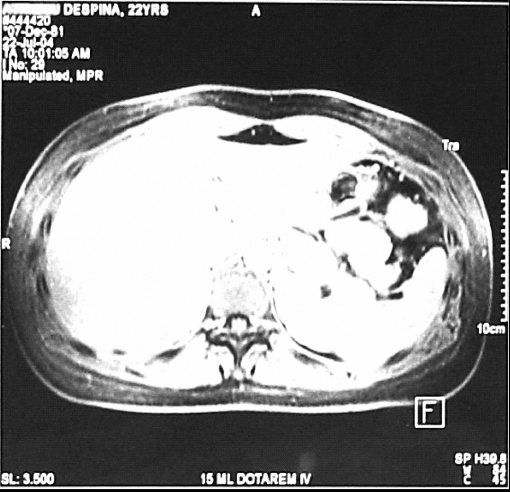
Computed tomography (CT) of the abdomen showed a 12×7×8-cm homogenous mass of the right adrenal (Figure 1). Magnetic resonance imaging (MRI) showed a solid mass measuring 13×7×7.5 cm arising from the right adrenal. On T2-weighted MR images, the tumor was shown as a heterogeneous mass. After intravenous injection of gadolinium, the mass showed a progressive, heterogeneous, and delayed enhancement (Figure 2). Preoperative radiological differential diagnoses were those of a GN and myelolipoma. No evidence was present of calcification or invasion of adjacent tissues or organs.
Figure 1.
Abdominal computed tomographic scan indicating the large benign tumor.
Figure 2.
Magnetic resonance imaging. After intravenous injection of gadolinium, the mass showed a progressive, heterogeneous, and delayed enhancement.
A laparoscopic approach was decided on, despite the large size of the tumor, because of the low risk of malignancy based on radiology findings.
Technical Aspects of the Procedure
We prefer the transperitoneal lateral decubitus approach, as the best for maximal exposure of the gland and major vessels. Using the Hasson technique, we introduced a 12-mm trocar, two 10-mm trocars, and one 5-mm trocar. Laparoscopic exploration of the abdominal cavity was normal, and the tumor was easily identified. The right triangular ligament and the retroperitoneal liver attachments were cauterized and divided to allow liver retraction. After dividing the retroperitoneum, the inferior vena cava (IVC) was identified. The inferior periadrenal fat was carefully dissected from the upper pole of the right kidney and the renal vein identified. The adrenal vein was subsequently identified, dissected, double-clipped, and divided. The inferior and superior adrenal vessels were cauterized or clipped. Ultrasonic scissors were not used. The specimen was extracted through an extension of the incision done for the Hasson technique. Minimal blood loss occurred, and the patient was not transfused.
The procedure lasted 90 minutes. The surgical specimen was oval and elastic in consistency, measuring 13×9.5×6 cm and weighing 390 g. The patient was discharged on the second postoperative day with bowel function returned to normal and able to resume normal physical activity.
Histology Report
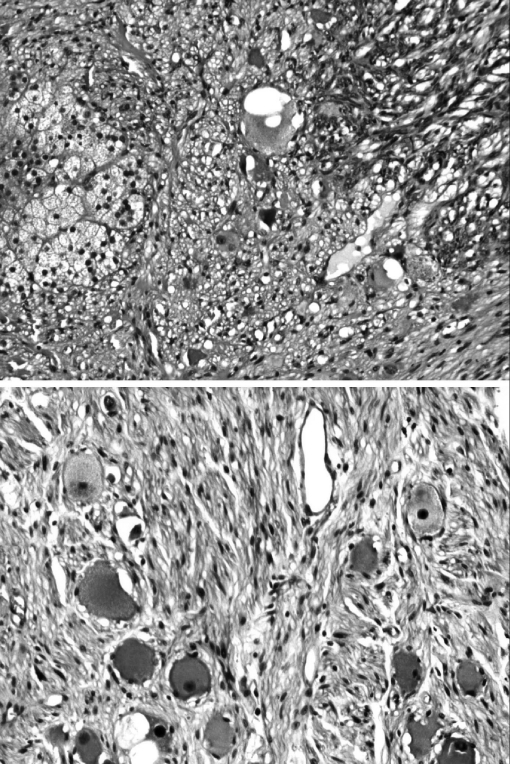
By gross inspection, a large encapsulated tumor mass of 13×9.5×6 cm, weighed 390 g. On the surface of the tumor, small foci of flattened adrenal tissue were recognized. By sectioning, the tumor had a solid homogenous appearance and was grayish-white to yellowish on the cut surface. Microscopically, it was composed mostly of spindle cells arranged in fascicles. Mature ganglion cells scattered or arranged in small clusters were also noted (Figure 3). The described features were diagnostic of ganglioneuroma. No additional treatment was administered for this benign tumor. Two years after the procedure, there is no evidence of recurrence on abdominal CT scan, and the cosmetic result is satisfactory.
Figure 3.
Top: Low magnification shows ganglioneuroma (right) with adjacent normal adrenal cortex (left) (H&E ×10). Bottom: High magnification demonstrates spindle and mature ganglion cells (H&E ×20).
DISCUSSION
Ganglioneuromas are rare tumors, and there is a relative paucity of information in the literature concerning their exact incidence.4,9,10,12–14 This is clinically relevant as the incidence of all adrenal tumors is increasing due to the availability of sophisticated imaging techniques and expertise; approximately, 1% to 10% of abdominal CT scans report incidentally an adrenal tumor.3 Based on several series, GN accounts from 0% to 6% of incidentalomas. It is encountered rather more frequently in the literature when comparing its incidence among other large tumors of greater than 6 cm in maximum diameter.3,11,13,14 Approximately 100 cases of adrenal GN and 112 cases of extra adrenal GN have been reported in the Japanese literature.15
The imaging based differential diagnosis of an asymptomatic, nonfunctioning giant adrenal mass without evidence of systematic disease is broad and includes besides GN, neuroblastoma, ganglioneuroblastoma, myelolipoma and angiomyolipoma.8 In the present case, the differential diagnoses suggested on MRI findings were benign tumor of the CNS (GN) and myelolipoma. Both CT scan and MRI are superior to US in detecting and characterizing an adrenal mass. Following the availability of studies comparing radiologically found and histologically proven dimensions of adrenal lesions, it was shown that CT scanning might underestimate the tumor size by 16% to 47%, whereas MRI does so by 20%. However, MRI appearances may correlate better with a histological diagnosis.11,16–20
Retroperitoneal GNs appear as well-defined masses that are oval, crescentic, or lobulated. They tend to surround major blood vessels; the result is absent or mild compromise of the lumen.2,21,22 Intratumoral calcifications are present in 2.4% to 40% of cases; however, no calcifications were observed in our case. Areas of low attenuation that do not enhance are common, although such an enhancement is usually of low intensity. An interesting pattern consists of delayed heterogeneous uptake of contrast media, which was observed on the MRI of the present case.7
Adrenal myelolipoma is a rare benign tumor composed of mature fat tissue associated with proliferating hematopoietic cells. CT features are characteristic if lipid content is demonstrated, which was not observed in our case.23,24
Hemorrhagic adrenal adenoma, adrenocortical carcinoma, metastatic tumors to the adrenal gland, and angiomyolipoma of the upper renal pole may also simulate GN or myelolipoma.25–29 The other tumors of the CNS (neuroblastoma and ganglioneuroblastoma) develop at the same sites as the GN, but they occur in much younger patients and particularly in children. Such tumors are usually quite aggressive, having developed metastases in bone, liver, and lung in approximately 50% of cases. Intratumoral calcifications are higher in proportion and number.30,31
It has recently been demonstrated that scintigraphy and positron emission tomography (PET) can complement CT and MRI in diagnosing GNs.32,33
Laparoscopic adrenalectomy has become the gold standard in most patients with adrenal tumors.34 Laparoscopic procedures are associated with less postoperative discomfort, shorter hospital stay, less postoperative disability, and a lower rate of complications. There are few absolute contraindications for laparoscopic adrenalectomy, and most of them are not specific to adrenal surgery. Large but well encapsulated adrenal masses without evidence of local invasion can be removed laparoscopically.3 The lateral transabdominal approach offers the best visualization of major vessels adjacent to the adrenals.35 The possibility of malignancy should be appreciated preoperatively (using CT, MRI, or both) as well as intraoperatively. Invasion of periadrenal tissues or organs is not well suited to laparoscopic techniques and needs conversion to an open procedure.
Several authors limit the laparoscopic adrenalectomy to lesions less than 6 cm in size,12 whereas others have performed laparoscopic adrenalectomy on tumors up to 13cm in diameter without any significant morbidity.5,13 Extensive experience in advanced laparoscopic techniques and open adrenal surgery are mandatory to manipulate and laparoscopically excise large tumors.
CONCLUSION
In summary, adrenal ganglioneuroma is a rare benign adrenal tumor that needs careful evaluation and surgical treatment. Laparoscopic resection of large tumors is feasible but necessitates experience in advanced laparoscopic surgery.
Contributor Information
G. N. Zografos, Third Department of Surgery, Athens General Hospital, “G. Gennimatas,” Greece..
K. Kothonidis, Third Department of Surgery, Athens General Hospital, “G. Gennimatas,” Greece..
C. Ageli, Third Department of Surgery, Athens General Hospital, “G. Gennimatas,” Greece..
N. Kopanakis, Third Department of Surgery, Athens General Hospital, “G. Gennimatas,” Greece..
K. Dimitriou, Department of Endocrinology, Athens General Hospital, “G. Gennimatas,” Greece..
E. Papaliodi, Department of Pathology, Athens General Hospital, “G. Gennimatas,” Greece..
G. Kaltsas, Department of Endocrinology, Athens General Hospital, “G. Gennimatas,” Greece..
M. Pagoni, Department of Internal Medicine, Athens General Hospital, “G. Gennimatas,” Greece..
G. Papastratis, Third Department of Surgery, Athens General Hospital, “G. Gennimatas,” Greece..
References:
- 1. Chang CY, Hsieh YL, Hung GY, Pan CC, Hwang B. Ganglioneuroma presenting as an asymptomatic huge posterior mediastinal and retroperitoneal tumor. J Chin Med Assoc. 2003;66(6):370–374 [PubMed] [Google Scholar]
- 2. Radin R, David CL, Goldfarb H, Francis IR. Adrenal and extra-adrenal retroperitoneal ganglioneuroma: imaging findings in 13 adults. Radiology. 1997;202:703–707 [DOI] [PubMed] [Google Scholar]
- 3. Brunt ML, Moley JF. Adrenal incidentaloma. World J Surg. 2001;25:905–913 [DOI] [PubMed] [Google Scholar]
- 4. Enzinger FM, Weiss SW. Soft tissue tumors. 2nd ed St Louis, MO: Mosby-Year Book, 1988;719–860 [Google Scholar]
- 5. Ichikawa T, Koyama A, Fujimoto H, et al. Retroperitoneal ganglioneuroma extending across the midline: MR features. Clin Imaging. 1993;17:19–21 [DOI] [PubMed] [Google Scholar]
- 6. Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM. Neurogenic tumours in the abdomen: tumour types and imaging characteristics. Radiographics. 2003;23(1):29–43 [DOI] [PubMed] [Google Scholar]
- 7. Moriwaki Y, Miyake M, Yamamoto T, et al. Retroperitoneal ganglioneuroma: a case report and review of the Japanese literature. Int Med. 1992;31:82–85 [DOI] [PubMed] [Google Scholar]
- 8. Tischler AS. Divergent differentiation in neuroendocrine tumors of the adrenal gland. Semin Diagn Pathol. 2000;17(2):120–126 [PubMed] [Google Scholar]
- 9. Juarez D, Brown RW, Ostrowski M, Reardon MJ, Lechago J, Truong LD. Pheochromocytoma associated with neuroendocrine carcinoma. A new type of composite pheochromocytoma. Arch Pathol Lab Med. 1999;123(12):1274–1279 [DOI] [PubMed] [Google Scholar]
- 10. Watanabe T, Noshiro T, Kusakari T, et al. Two cases of pheochromocytoma diagnosed histopathologically as mixed neuroendocrine-neural tumour. Intern Med. 1995;34(7):683–687 [DOI] [PubMed] [Google Scholar]
- 11. Kouriefs C, Leris AC, Mokbel K, Grossman AB, Reznek R, Carpenter R. Abdominal ganglioneuromas in adults. Urol Int. 2003;71(1):110–113 [DOI] [PubMed] [Google Scholar]
- 12. NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens State Sci Statements. 2002;19(2):1–23 [PubMed] [Google Scholar]
- 13. Henry JF, Sebag F, Iacobone M, Mirallie E. Results of laparoscopic adrenalectomy for large and potentially malignant tumors. World J Surg. 2002;26(8):1043–1047 [DOI] [PubMed] [Google Scholar]
- 14. Pillinger SH, Bambach CP, Sidhu S. Laparoscopic adrenalectomy: a 6-year experience of 59 cases. Aust N Z J Surg. 2002;72(7):467–470 [DOI] [PubMed] [Google Scholar]
- 15. Yamaguchi K, Hara I, Takeda M, et al. Two cases of ganglioneuroma. Urology. 2006;67(3):622. [DOI] [PubMed] [Google Scholar]
- 16. Kouriefs C, Mokbel K, Choy C. Is MRI scan more accurate than CT in estimating the real size of adrenal tumors? Eur J Surg Oncol. 2001;27:487–490 [DOI] [PubMed] [Google Scholar]
- 17. Lau H, Lo CY, Lam KY. Surgical implications of underestimation of adrenal tumour size by CT. Br J Surg. 1999;86:385–387 [DOI] [PubMed] [Google Scholar]
- 18. Linos DA, Stylopoulos N. How accurate is the computed tomography in predicting the real size of adrenal tumours? Arch Surg. 1997;132:740–743 [DOI] [PubMed] [Google Scholar]
- 19. Cerfolio RJ, Vaughan ED, Jr., Brennan TG, Jr., Hirvela ER. Accuracy of computed tomography in predicting adrenal tumour size. Surg Gynecol Obstet. 1993;176:307–309 [PubMed] [Google Scholar]
- 20. Zhang Y, Nishimura H, Kato S, et al. MRI of ganglioneuroma: Histologic correlation study. J Comput Assist Tomog. 2001;25:617–623 [DOI] [PubMed] [Google Scholar]
- 21. Ichikawa T, Koyama A, Fujimoto H, et al. Retroperitoneal ganglioneuroma extending across the midline: MR features. Clin Imaging. 1993;17:19–21 [DOI] [PubMed] [Google Scholar]
- 22. Ichikawa T, Ohtomo K, Araki T, et al. Ganglioneuroma: CT and MR features. Br J Radiol. 1996;69:114–121 [DOI] [PubMed] [Google Scholar]
- 23. Rao P, Kenney PJ, Wagner BJ, Davidson AJ. Imaging and pathologic features of myelolipoma. Radiographics. 1997;17:1373–1385 [DOI] [PubMed] [Google Scholar]
- 24. Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87–95 [DOI] [PubMed] [Google Scholar]
- 25. Otal P, Escourrou G, Mazerolles C, et al. Imaging features of uncommon adrenal masses with histopathologic correlation. Radiographics. 1999;19(3):569–581 [DOI] [PubMed] [Google Scholar]
- 26. Zografos GN, Korkolis D, Georgoutsos P, et al. Giant myelolipoma of the right adrenal gland. Review. Int J Clin Pract. 2002;56(4):319–320 [PubMed] [Google Scholar]
- 27. Dunphy CH. Computed tomography-guided fine needle aspiration biopsy of adrenal myelolipoma. Case report and review of the literature. Acta Cytol. 1991;35:353. [PubMed] [Google Scholar]
- 28. Miyake H, Maeda H, Tashiro M, et al. CT of adrenal tumors: frequency and clinical significance of low-attenuation lesions. AJR. 1989;152:1005–1007 [DOI] [PubMed] [Google Scholar]
- 29. Gould JD, Mitty HA, Pertsemlidis D, Szporn AH. Adrenal myelolipoma: diagnosis by fine needle aspiration. AJR. 1987;148:921–922 [DOI] [PubMed] [Google Scholar]
- 30. Dubois C, Jankowski A, Gay-Jeune C, Chabre O, Pasquier D, Ferretti G. Imaging of adrenal ganglioneuroma: a case report [in French]. J Radiol. 86(6 pt 1):659–662, 2005 [DOI] [PubMed] [Google Scholar]
- 31. Lonergan GJ, Schab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma and ganglioneuroma: radiologicpathologic correlation. Radiographics. 2002;22(4):911–934 [DOI] [PubMed] [Google Scholar]
- 32. Birgit G, Barbara H, Dieter H, et al. Metabolic activity and clinical features of primary ganglioneuroma. Cancer. 2001;91:1905–1913 [DOI] [PubMed] [Google Scholar]
- 33. Ilias I, Shulkin B, Pacak K. New functional imaging modalities for chromaffin tumors, neuroblastomas and ganglioneuromas. Trends Endocrinol Metab. 2005;16(2):66–72 [DOI] [PubMed] [Google Scholar]
- 34. Stanley DG. Laparoscopic adrenalectomy. Int Surg. 1994;79(3):253–258 [PubMed] [Google Scholar]
- 35. Zografos GN, Markou A, Ageli C, et al. Laparoscopic surgery for adrenal tumors. A retrospective analysis. Hormones. 2006;5(1):52–56 [DOI] [PubMed] [Google Scholar]