Abstract
Contrast agents are increasingly being used to characterize the vasculature in an organ of interest, to better delineate benign from malignant pathology and to aid in staging and directing therapeutic procedures. We review the mechanisms of action of first, second and third generation contrast agents and their use in various endoscopic procedures in the gastrointestinal tract. Various applications of contrast-enhanced endoscopic ultrasonography include differentiating benign from malignant mediastinal lymphadenopathy, assessment of depth of invasion of esophageal, gastric and gall bladder cancers and visualization of the portal venous system and esophageal varices. In addition, contrast agents can be used to differentiate pancreatic lesions. The use of color Doppler further increases the ability to diagnose and differentiate various pancreatic malignancies. The sensitivity of power Doppler sonography to depict tumor neovascularization can be increased by contrast agents. Contrast-enhanced harmonic imaging is a useful aid in identifying the tumor vasculature and studying pancreatic microperfusion. In the future, these techniques could potentially be used to quantify tumor perfusion, to assess and monitor the efficacy of antiangiogenic agents, to assist targeted drug delivery and allow molecular imaging.
Keywords: Contrast media, Endoscopic ultrasonography, Gastrointestinal neoplasms, Doppler ultrasonography, Pancreatic cancer
CONTRAST-ENHANCED ENDOSCOPIC ULTRASONOGRAPHY
The use of intravenous contrast agents in ultrasonography was first utilized in echocardiography to enhance imaging of cardiac chambers and great vessels[1]. Since then, they have been used in transabdominal ultrasonography and more recently in endoscopic ultrasonography (EUS). Use of contrast agents in EUS has been shown to improve the characterization of the vasculature inside the organ of interest, to better delineate benign from malignant pathology[2-8], to aid in staging and directing therapeutic procedures and thereby to determine prognosis.
CONTRAST AGENTS
Contrast agents are made of gas-filled microbubbles encapsulated by a phospholipid or albumin shell. They are categorized into first, second and third generation based on their capability for transpulmonary passage and their half-life in the human body. Commonly used first generation agents include Albunex, Levovist and Echovist. Second generation agents include SonoVue, Sonazoid, and Optison among others[9,10]. The only third generation agent currently available is Echogen, capable of phase-shift from liquid to gas form once it attains body temperature[11]. Contrast agents in use today are relatively safe and have demonstrated no severe, long-lasting adverse effects in humans (Table 1)[12,13].
Table 1.
| Contrast agent | Composition | Manufacturer |
| First generation | ||
| Albunex | 5% human albumin with stabilized microbubbles | Mallinckrodt |
| Echovist (SHU 454) | Standardized microbubbles with galactose shell | Schering |
| Levovist (SHU 508) | Stabilized, standardized microbubbles with galactose, 0.1% palmitic acid shell | Schering |
| Myomap | Albumin shell | Quadrant |
| Quantison | Albumin shell | Quadrant |
| Sonavist | Cyanoacrylate shell | Schering |
| Sonazoid | C4F10 with lipid stabilizer shell | GE healthcare |
| Second generation | ||
| Definity/luminity | C3F8 with lipid stabilizer shell | Bristol–myers squibb medical imaging |
| Imagent-imavist | C6H14 with lipid stabilizer shell | Alliance |
| Optison | C3F8 with denatured human albumin shell | GE healthcare |
| Bisphere/cardiosphere | Polylactide-coglycolide shell with albumin overcoat | - |
| SonoVue (BR1, Bracco, Italy) | SF6 gas with lipid stabilizer shell | Bracco |
| AI700/imagify | C4F10 gas core stabilized with polymer shell | Acusphere |
| Third generation | ||
| Echogen | Dodecafluoropentane (DDFP) liquid in phase shift colloid emulsion | Sonus pharmaceuticals |
MECHANISMS OF ACTION
Contrast agents were specifically developed to image vascularity and vessel patterns, especially for small volume and slow velocity blood flow. This is highly important in tumors, where angiogenesis completely alters the vascular structure. The principle of ultrasound contrast agents is that they create multiple small interfaces with high echogenicity, a process best achieved by gaseous microbubbles, surrounded by a shell used to increase stability[14]. Microbubbles are very good backscatters, effectively reflecting the ultrasound waves. However, the microbubbles respond and oscillate to sound pressure in a non-linear fashion, with an asymmetrical diameter induced by ultrasound pressure. The diameter is variable between 2 and 10 μm, about the size of red blood cells. Consequently, they do not leave the vascular system (blood pool contrast agents). The ultrasound contrast agents are administered through intravenous bolus injection, in a large arm vein. Second-generation contrast agents are those passing through the lungs, allowing contrast enhancement of the entire vascular system.
Contrast agents were used initially as Doppler signal enhancers, including in contrast-enhanced EUS examinations (CE-EUS). Both color Doppler and power Doppler can be used, especially for regions with very low flow volumes, where the unenhanced signal is too weak or the signal-noise ratio is too poor (Figures 1 and 2). Although the contrast agent selectively enhances the useful signal to the detriment of the noise, the main disadvantage of these techniques is the presence of artifacts. Both tissue motion (flash) artifacts and blooming artifacts appear and impede the examinations. Flash artifacts are specific to the Doppler mode, appearing as color signals caused by tissue motion, being most commonly seen in hypoechoic areas, induced by cardiac or respiratory motion[15]. Blooming artifacts appear as a consequence of the high amplification of the backscattered signal, which saturates the receiver and causes smearing of the color signal. They appear immediately after the wash-in phase and disappear when the concentration of contrast is lower[16]. The introduction of second generation contrast agents made it possible to enhance B-mode and contrast-harmonic imaging for improved visualization (Figure 3)[17,18].
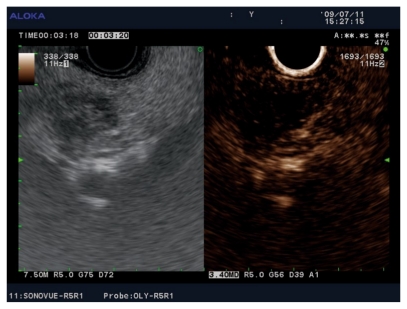
Figure 1.
Contrast enhanced endoscopic ultrasonography exam of lung adenocarcinoma. A: Non-enhanced power Doppler image of a lung adenocarcinoma visualized in the aorto-pulmonary window from the mid-esophagus, with discrete Doppler signals in the periphery of the mass and embedding of a large branch of the left pulmonary artery; B: Same tumor visualized after contrast-enhancement with SonoVue, with a better depiction of the vascular peripheral signals and the possibility of quantification of the vascular index. The relationship to the aorta and pulmonary artery is clearly depicted.
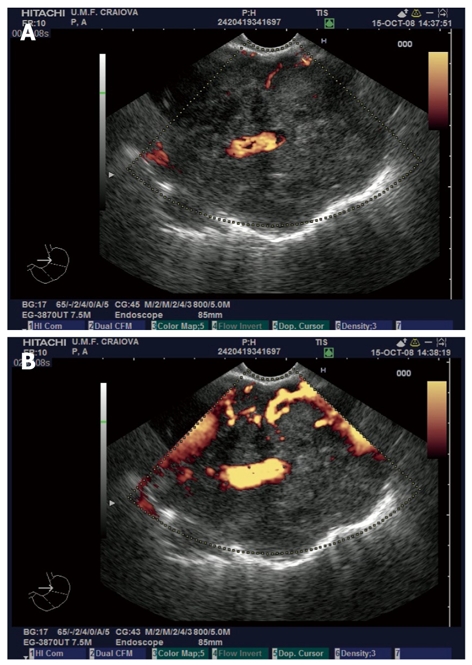
Figure 2.
Contrast enhanced endoscopic ultrasonography of pancreatic cancer. A: Pancreatic head adenocarcinoma visualized in bidirectional non-enhanced power Doppler mode; B: Contrast-enhancement with SonoVue indicates a hypovascular mass with increased collateral circulation.
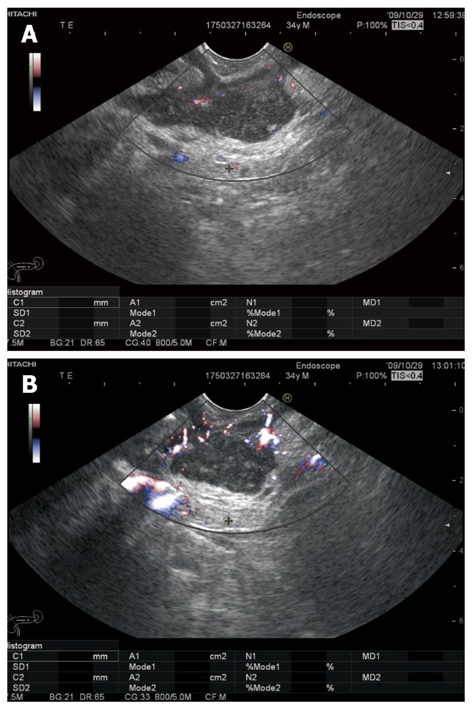
Figure 3.
Contrast-enhanced (SonoVue) harmonic endoscopic ultrasound imaging showing a small (12 mm) hypovascular adenocarcinoma in the head of the pancreas. The tumor tissue did not enhance in the early arterial phase, nor in the late venous phase, as compared to the surrounding pancreatic parenchyma.
CLINICAL USES OF CE-EUS
Differentiating benign from malignant mediastinal lymphadenopathy
EUS-guided fine-needle aspiration (FNA) represents the current “gold-standard” for the diagnosis of malignant mediastinal lymphadenopathy[19,20], and is further improved by localized cytopathologic assessment of the specimens[21]. Nonetheless, EUS-FNA carries the risk of mediastinitis if inflammatory nodes are aspirated, contamination and tumor seeding. However, studies have not been consistent in their findings[6,22]. CE-EUS may offer a non-invasive method to increase the specificity of diagnosis of benign lymph nodes, and aid in targeting aspiration of only high-yield lymph nodes.
Differentiating benign from malignant lymph nodes using appearance and type (arterial, venous) of vascularity may not be reliable since non-lymphomatous cancer cells invade lymph nodes heterogeneously[23]. Currently, CE-EUS cannot replace EUS-guided FNA in confirming malignant mediastinal lymph nodes. The combination of CE-EUS and EUS-FNA will possibly improve diagnostic accuracy.
Esophageal and gastric cancer
EUS can provide cross-sectional imaging of the wall of the gastrointestinal tract, and determine the depth of invasion of cancers. The normal esophageal and gastric walls consist of five layers on EUS images with enhancement of the third and fifth layers (submucosa and subserosa, respectively). Esophageal cancers are not enhanced with CE-EUS because of their relative avascularity[8]. In gastric cancer, assessment of the depth of invasion can be improved with CE-EUS, especially for depressed, endophytic cancers. Use of CE-EUS improves the overall accuracy of assessment of depth of invasion of gastric carcinoma from 70% to 90%. Active ulcers and scars in both malignant and non-malignant lesions are not enhanced post-contrast. This has been attributed to the nature of vascularity (linear convergence) and foci of fibrosis. Gastric myogenic tumors appear as hypoechoic masses linked to the fourth layer on EUS[8]. Hirooka et al[24] demonstrated that poorly differentiated gastric carcinomas were enhanced by infusion of Albunex whereas well differentiated ones were not. However, prediction of histologic type of gastric carcinoma by the nature of the enhancement has been inconsistent.
Gallbladder diseases
CE-EUS has the potential to differentiate gallbladder lesions and assess the depth of tumor infiltration in gallbladder carcinomas[5]. It can differentiate chronic cholecystitis and cholesterol polyps from infiltrating and exophytic gallbladder cancer, respectively, since the three-layer structure remains intact in the benign conditions. Majority of gallbladder adenocarcinomas enhance with EUS on administration of Albunex[5], unlike other gallbladder diseases including adenosquamous carcinoma cholesterol polyps and chronic cholecystitis[5,24]. CE-EUS is also able to clearly differentiate the depth of invasion in the gallbladder wall from T1b from T1a, improving accuracy over standard EUS[5].
Pancreatic diseases
First generation: CE-EUS has been used in pancreatic cancer to demarcate vascular landmarks, detect vascular obliteration by a thrombus or tumor, and examine microvascular blood flow to organs and lesions.
Albunex was the earliest contrast agent used to enhance EUS images. Hirooka et al[24] demonstrated that peripheral injection of Albunex can enhance B-mode images of pancreatic pathology during high-frequency EUS. Enhancement was marked in cases of pancreatic islet cell tumors. Pancreatic ductal cell carcinomas remained unenhanced compared to the surrounding normal parenchyma and fibrosis thereby making boundaries clearer[24]. Administration of contrast also improved the capability for differential diagnosis of lesions identified by B-mode EUS[25].
A study by the same authors in 1998 demonstrated similar findings with 100% image enhancement (at 12 Hz) using Albunex in islet cell carcinomas and serous cystadenomas, 80% enhancement in mucin-producing tumors, and 75% in chronic pancreatitis. Also, no enhancement was noted with ductal cell carcinomas and pancreatic pseudocysts, consistent with hypovascularity. Differences in vascularity as demonstrated on angiography paralleled the enhancement patterns during CE-EUS, except in 20% and 25% of cases with mucin-producing tumors and chronic pancreatitis, respectively. In addition, they demonstrated that areas of normal parenchyma and fibrosis around a lesion can be enhanced, demarcating the boundaries. This could lead to accurate pre-operative staging and planning of surgical resection lines, in the case of mucinous tumors involving the main pancreatic duct[4].
The authors propose that enhancement after Albunex may be related, at least in part, to the nature of microcirculation and vascular permeability of the lesion, which determine the concentration of contrast agent within the lesion. This could account for the less predictive pattern of angiography with sonographic enhancement[4]. Concentric bile duct wall thickening on intraductal ultrasonography with strong enhancement after administration of Levovist was seen in patients with autoimmune pancreatitis with a reduction in enhancement after steroid therapy likely indicating resolution of inflammation[26].
Second generation: Using an experimental second generation microbubble contrast agent, Wong et al[27] demonstrated hypoechogenicity in normal pancreatic tissue after a bolus but not with continuous infusion. This could be related to a greater intravascular density of contrast material with bolus injection compared to a continuous infusion. A decreased echo signal from the pancreatic parenchyma after contrast injection may be due to an increased signal from the pancreatic interface with adjacent structures[27]. Whether this will have a clinically useful application remains to be determined. Certainly, lesions that are enhanced with contrast will be more easily distinguished from the surrounding normal pancreas.
CE-EUS reveals the characteristic vascularity and can diagnose and follow up intraductal papillary mucinous neoplasms (IPMN) of the pancreas. Enlargement or enhancement of a mural nodule accurately indicated the presence of atypical malignant epithelium and determined the need for surgical resection[28]. Mural nodules were classified into four types based on morphology during EUS, before and after contrast: Type 1 (low papillary type), Type 2 (polypoid type), Type 3 (villous type) and Type 4 (invasive type with a blurred hypoechoic area between lesion and parenchyma). When IPMNs with Type 3/4 were diagnosed as malignant, accuracy was higher[29].
The use of CE-EUS has also been used to differentiate between mass-forming chronic pancreatitis and pancreatic cancer. Focal lesions can be seen in alcohol and autoimmune pancreatitis, with presentation similar to that of pancreatic cancer. CE-EUS produces a “parenchymographic” enhancement (i.e. isovascular to pancreatic parenchyma) in inflammatory benign masses and shows an inverse correlation with the degree of fibrosis within the mass, the duration of the inflammatory process and the enhancement with contrast infusion. Ductal carcinomas exhibit complete absence or a low level of enhancement due to greater fibrosis within the tumor[30,31].
Color Doppler
Combining B-mode EUS with CE-Doppler ultrasound improves the visualization of the vascularity of a pancreatic lesion, with malignant ductal adenocarcinoma demonstrating low flow and a relatively avascular pattern. Bhutani et al[32] described enhancement of color Doppler signals from the celiac artery, superior mesenteric artery, and portal vein during EUS in a swine model after administration of Levovist. This effect was easily appreciated without the need for complex quantitative measurements. No visually obvious enhancement was evident in vessels such as the aorta that already had a pronounced unenhanced color Doppler signal[32]. Using Optison (FS069), Becker et al[33] demonstrated that the sensitivity and specificity of echo-enhanced color-Doppler EUS are comparable with the cytopathology results. Ueno et al[34] differentiated islet cell tumors and ductal cell cancer with color-Doppler EUS. Islet cell tumors had marked hypervascularization whereas patients with adenocarcinoma had vascularity only around the tumor. These results have been confirmed by several other investigators. Hypovascularity as a sign of malignancy in CE-EUS can provide 92% sensitivity and 100% specificity (89%-100%)[2]. Using CE-Doppler EUS, hypovascularized malignant ductal adenocarcinoma and hypervascularized benign tumor entities, mostly neuroendocrine tumors, and serous microcystic adenomas of the pancreas can be easily differentiated. This is of pivotal importance since serous microcystic adenomas can be observed due to low growth potential, and neuroendocrine tumors may be enucleated or otherwise and less radically resected compared to ductal adenocarcinoma.
Power Doppler
Unenhanced power Doppler ultrasonography is unable to provide tumor differentiation, as a previous study showed a very low specificity (77%) of unenhanced power Doppler EUS[35]. Although other factors like the presence of peripancreatic collaterals, might improve the specificity, this was not confirmed in larger studies. It is possible to misdiagnose necrotic pancreatitis as ductal adenocarcinoma and also to find inflammation surrounding ductal adenocarcinomas. Indeed, the presence of power Doppler inside the inflammatory masses is variable as a function of inflammation and necrosis, thus complicating the differential diagnosis[35].
The sensitivity of power Doppler sonography to depict tumor neovascularization can be increased by contrast agents. In an animal model of pancreatic vascular disruption using 50% ethanol plus purified carbon particle solution, standard EUS demonstrated hypoechogenicity in the ethanol treated area. With injection of Definity, power Doppler EUS revealed marked contrast enhancement of normal pancreatic parenchyma from the ethanol-treated area[36]. Several studies using CE-EUS with power Doppler scanning also demonstrated an improvement in discrimination of pancreatic cancer from chronic pancreatitis[33,37,38] and may also help to localize small benign tumors such as insulinomas[7].
Hocke et al[38], using pulsed Doppler analysis with CE-Doppler EUS, demonstrated an improvement in the differentiation between chronic pancreatitis and malignancy. They used specific criteria to define malignancy: lack of vascularization before injection of SonoVue, irregular appearance of arterial vessels over a short distance post-injection, and absence of detection of venous vessels in the lesion[38]. In contrast to the technique described by Becker et al[33], Hocke et al[38] combined the analysis of the detected vessels with pulsed wave Doppler analysis. They concluded that the use of second generation contrast agents with low mechanical index techniques will possibly allow real-time imaging with or without three-dimensional reconstructions in EUS imaging.
With CE power Doppler sonography, the signal intensity from flowing blood is lower compared to that of moving solid tissue structures. Harmonic imaging was specifically developed to overcome these obstacles, since tissue particles have fewer harmonic waves than intravascular microbubbles, thus avoiding flash and blooming artifacts[35].
Harmonic imaging
CE harmonic imaging techniques are currently available for EUS, as a result of the improvement in transducer technology. Thus, the use of adequate broadband transducers that can detect harmonic signals was recently been reported[17,25]. A pilot study previously described an experimental technique with low mechanical index, which allowed differentiation between chronic pancreatitis and pancreatic cancer, based on tissue microperfusion characteristics[17]. Another feasibility study demonstrated both parenchymal perfusion and microvasculature in the pancreas[25]. Both intermittent homogeneous parenchymal perfusion images and real-time continuous images of finely branching vessels of the pancreas were obtained with a mechanical index of 0.4. Although the initial study included a small number of patients with pancreatic lesions, it seemed that tumor characterization was possible based on the vascular or perfusion pattern. Thus, pancreatic carcinomas had absent or heterogeneous perfusion images in the intermittent mode, while the vessels were visualized as irregular “network like” structures in real-time mode. Both neuroendocrine tumors and chronic pseudotumoral pancreatitis were homogenous and iso- or hyper-vascular. Several other research groups are testing the feasibility of CE-EUS[39-41]. CE-EUS with low mechanical index (0.4) was tested in 25 patients, after peripheral injection of SonoVue[39]. The method seemed feasible for differentiating adenocarcinoma from other focal mass lesions, being proposed as the method of choice to establish the management of patients when EUS-FNA is non-contributive. Harmonic imaging has also been used with CE-EUS after peripheral injection of Sonazoid in two settings, WPI (wide-band pulse inversion harmonic) and EXPHD (extended pure harmonic detection)[40]. The change in echo-intensity was evaluated. Ductal carcinomas, IPMTs, chronic pancreatitis and endocrine tumors demonstrate varied echo-intensities after infusion of contrast agent. CE harmonic EUS can be a useful aid in identifying tumor vasculature, especially that of pancreatic masses[41].
Esophageal varices and portal hypertension
B-mode EUS can detect grade II varices or larger. After administration of Levovist, flow signals can become evident beneath the third echogenic layer of the esophageal wall and help visualize perforating veins and periesophageal vessels[42]. EUS-guided portal vein angiography by using CO2 as a contrast agent, has been evaluated in a porcine model. This is less viscous, making it easier to inject through small-caliber needles, minimizing damage to the vascular wall compared with iodinated contrast (Table 2)[43].
Table 2.
Indications for the use of contrast agents during endoscopic ultrasonography
| Study | Indication | Agent used |
| Hocke et al[6] | Differentiating benign from malignant lymph nodes | SonoVue |
| Kanamori et al[22] | Levovist | |
| Nomura et al[8] | Assessment of depth of invasion of esophageal cancer | Air-filled Albumin |
| Nomura et al[8] | Assessment of depth of invasion of gastric cancer | Air-filled Albumin |
| Itoh et al[28] | Differentiating benign from malignant intraductal papillary mucinous tumors of the pancreas | Levovist |
| Hirooka et al[5] | Gallbladder diseases | Albunex |
| Ueno et al[34] | Diagnosing Islet cell tumors | Levovist |
| Sakamoto et al[40] | Determining origin of solid pancreatic masses | Levovist with suspension of monosaccharide microparticles |
| Hirooka et al[24] | Albunex | |
| Dietrich et al[2] | Levovist | |
| Sofuni et al[41] | Levovist | |
| Becker et al[33] | Discriminating between mass forming pancreatitis and pancreatic cancer | Optison |
| Hocke et al[6] | SonoVue | |
| D’Onofrio et al[31] | SonoVue | |
| Hyodo et al[26] | Diagnosing cause of chronic pancreatitis/mass forming pancreatitis (autoimmune pancreatitis) | Levovist |
| D’Onofrio et al[31] | SonoVue | |
| Zhu et al[30] | SonoVue | |
| Kasono et al[7] | Localizing small insulinomas | Levovist |
FUTURE PERSPECTIVES
Tumor blood flow was previously linked in several studies with both metastasis potential and poor prognosis. A clear correlation was also proven between microvessel density, different angiogenic factors [e.g. vascular endothelial growth factor (VEGF)] and the tumors with definite vascular signals demonstrated by CE ultrasound[44]. Quantification of tumor perfusion has been proven feasible for the early assessment and monitoring of the efficacy of antiangiogenic agents in quantitative terms based on changes in vascularity, before morphological changes become apparent[45].
The feasibility of new technologies using CE ultrasound with microbubbles targeted to VEGF receptor type 2 are currently being tested[46-48]. Several applications of molecular imaging and targeted ultrasound therapy can also be envisioned in the near future, including determination of the detailed physical processes behind sonoporation (increased uptake of drugs inside the cell through transient porosities in the cell membrane in the presence of contrast agents).
In this context, the development of CE-EUS will be clearly beneficial for targeted ultrasound imaging and ultrasound-assisted drug-delivery applications in gastrointestinal tract tumors, as well as other tumors accessible by EUS (pancreatic and lung tumors, etc.).
Footnotes
Peer reviewer: Richard Hu, MD, MSc, Division of Gastroenterology, Department of Medicine, Olive view-UCLA Medical Center, 14445 Olive View Drive, Los Angeles, CA 91342, United States
S- Editor Sun H L- Editor Cant MR E- Editor Ma WH
References
- 1.Keller MW, Feinstein SB, Watson DD. Successful left ventricular opacification following peripheral venous injection of sonicated contrast agent: an experimental evaluation. Am Heart J. 1987;114:570–575. doi: 10.1016/0002-8703(87)90754-x. [DOI] [PubMed] [Google Scholar]
- 2.Dietrich CF, Ignee A, Braden B, Barreiros AP, Ott M, Hocke M. Improved differentiation of pancreatic tumors using contrast-enhanced endoscopic ultrasound. Clin Gastroenterol Hepatol. 2008;6:590–597.e1. doi: 10.1016/j.cgh.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg BB, Hilpert PL, Burns PN, Liu JB, Newman LM, Merton DA, Witlin LA. Hepatic tumors: signal enhancement at Doppler US after intravenous injection of a contrast agent. Radiology. 1990;177:713–717. doi: 10.1148/radiology.177.3.2173841. [DOI] [PubMed] [Google Scholar]
- 4.Hirooka Y, Goto H, Ito A, Hayakawa S, Watanabe Y, Ishiguro Y, Kojima S, Hayakawa T, Naitoh Y. Contrast-enhanced endoscopic ultrasonography in pancreatic diseases: a preliminary study. Am J Gastroenterol. 1998;93:632–635. doi: 10.1111/j.1572-0241.1998.179_b.x. [DOI] [PubMed] [Google Scholar]
- 5.Hirooka Y, Naitoh Y, Goto H, Ito A, Hayakawa S, Watanabe Y, Ishiguro Y, Kojima S, Hashimoto S, Hayakawa T. Contrast-enhanced endoscopic ultrasonography in gallbladder diseases. Gastrointest Endosc. 1998;48:406–410. doi: 10.1016/s0016-5107(98)70012-4. [DOI] [PubMed] [Google Scholar]
- 6.Hocke M, Menges M, Topalidis T, Dietrich CF, Stallmach A. Contrast-enhanced endoscopic ultrasound in discrimination between benign and malignant mediastinal and abdominal lymph nodes. J Cancer Res Clin Oncol. 2008;134:473–480. doi: 10.1007/s00432-007-0309-7. [DOI] [PubMed] [Google Scholar]
- 7.Kasono K, Hyodo T, Suminaga Y, Sugiura Y, Namai K, Ikoma A, Tamemoto H, Imawari M, Kawakami M, Ishikawa SE. Contrast-enhanced endoscopic ultrasonography improves the preoperative localization of insulinomas. Endocr J. 2002;49:517–522. doi: 10.1507/endocrj.49.517. [DOI] [PubMed] [Google Scholar]
- 8.Nomura N, Goto H, Niwa Y, Arisawa T, Hirooka Y, Hayakawa T. Usefulness of contrast-enhanced EUS in the diagnosis of upper GI tract diseases. Gastrointest Endosc. 1999;50:555–560. doi: 10.1016/s0016-5107(99)70083-0. [DOI] [PubMed] [Google Scholar]
- 9.Straub JA, Chickering DE, Church CC, Shah B, Hanlon T, Bernstein H. Porous PLGA microparticles: AI-700, an intravenously administered ultrasound contrast agent for use in echocardiography. J Control Release. 2005;108:21–32. doi: 10.1016/j.jconrel.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Klibanov AL. Ultrasound molecular imaging with targeted microbubble contrast agents. J Nucl Cardiol. 2007;14:876–884. doi: 10.1016/j.nuclcard.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Maresca G, Summaria V, Colagrande C, Manfredi R, Calliada F. New prospects for ultrasound contrast agents. Eur J Radiol. 1998;27 Suppl 2:S171–S178. doi: 10.1016/s0720-048x(98)00059-x. [DOI] [PubMed] [Google Scholar]
- 12.Karl-Jurgen Wolf FF. Color Duplex Sonography Principles and Clinical Applications. New York: Thieme Publishing Group; 1995. [Google Scholar]
- 13.Quaia E. Microbubble ultrasound contrast agents: an update. Eur Radiol. 2007;17:1995–2008. doi: 10.1007/s00330-007-0623-0. [DOI] [PubMed] [Google Scholar]
- 14.Greis C, Dietrich C. Ultrasound contrast agents and contrast-enhanced ultrasonography. In: Dietrich CF, editor. Endoscopic Ultrasound. An introductory manual and atlas. New York: Thieme Publishing Group; 2006. pp. 44–57. [Google Scholar]
- 15.Campbell SC, Cullinan JA, Rubens DJ. Slow flow or no flow? Color and power Doppler US pitfalls in the abdomen and pelvis. Radiographics. 2004;24:497–506. doi: 10.1148/rg.242035130. [DOI] [PubMed] [Google Scholar]
- 16.Forsberg F, Liu JB, Burns PN, Merton DA, Goldberg BB. Artifacts in ultrasonic contrast agent studies. J Ultrasound Med. 1994;13:357–365. doi: 10.7863/jum.1994.13.5.357. [DOI] [PubMed] [Google Scholar]
- 17.Dietrich CF, Ignee A, Frey H. Contrast-enhanced endoscopic ultrasound with low mechanical index: a new technique. Z Gastroenterol. 2005;43:1219–1223. doi: 10.1055/s-2005-858662. [DOI] [PubMed] [Google Scholar]
- 18.Sanchez MV, Varadarajulu S, Napoleon B. EUS contrast agents: what is available, how do they work, and are they effective? Gastrointest Endosc. 2009;69:S71–S77. doi: 10.1016/j.gie.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Micames CG, McCrory DC, Pavey DA, Jowell PS, Gress FG. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest. 2007;131:539–548. doi: 10.1378/chest.06-1437. [DOI] [PubMed] [Google Scholar]
- 20.Yasuda I, Tsurumi H, Omar S, Iwashita T, Kojima Y, Yamada T, Sawada M, Takami T, Moriwaki H, Soehendra N. Endoscopic ultrasound-guided fine-needle aspiration biopsy for lymphadenopathy of unknown origin. Endoscopy. 2006;38:919–924. doi: 10.1055/s-2006-944665. [DOI] [PubMed] [Google Scholar]
- 21.Tournoy KG, Praet MM, Van Maele G, Van Meerbeeck JP. Esophageal endoscopic ultrasound with fine-needle aspiration with an on-site cytopathologist: high accuracy for the diagnosis of mediastinal lymphadenopathy. Chest. 2005;128:3004–3009. doi: 10.1378/chest.128.4.3004. [DOI] [PubMed] [Google Scholar]
- 22.Kanamori A, Hirooka Y, Itoh A, Hashimoto S, Kawashima H, Hara K, Uchida H, Goto J, Ohmiya N, Niwa Y, et al. Usefulness of contrast-enhanced endoscopic ultrasonography in the differentiation between malignant and benign lymphadenopathy. Am J Gastroenterol. 2006;101:45–51. doi: 10.1111/j.1572-0241.2006.00394.x. [DOI] [PubMed] [Google Scholar]
- 23.Nakase K, Yamamoto K, Hiasa A, Tawara I, Yamaguchi M, Shiku H. Contrast-enhanced ultrasound examination of lymph nodes in different types of lymphoma. Cancer Detect Prev. 2006;30:188–191. doi: 10.1016/j.cdp.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Hirooka Y, Naitoh Y, Goto H, Ito A, Taki T, Hayakawa T. Usefulness of contrast-enhanced endoscopic ultrasonography with intravenous injection of sonicated serum albumin. Gastrointest Endosc. 1997;46:166–169. doi: 10.1016/s0016-5107(97)70067-1. [DOI] [PubMed] [Google Scholar]
- 25.Kitano M, Takagi T, Sakamoto H, Das K, Komaki T, Noda K, Yamao K, Kudo M. Dynamic imaging of pancreatic tumors by contrast-enhanced harmonic EUS with long-lasting contrast. Gastrointestinal Endoscopy. 2009;69:S228. [Google Scholar]
- 26.Hyodo N, Hyodo T. Ultrasonographic evaluation in patients with autoimmune-related pancreatitis. J Gastroenterol. 2003;38:1155–1161. doi: 10.1007/s00535-003-1223-7. [DOI] [PubMed] [Google Scholar]
- 27.Wong RF, Tarcin O, Reddy N, Ahmed I, Brining D, Matsunaga TO, Bhutani MS. Contrast-enhanced EUS (CE-EUS) using a new microbubble contrast agent (MRX-815) - a feasibility study in a porcine model. Gastrointestinal Endoscopy. 2006;63:AB274. [Google Scholar]
- 28.Itoh T, Hirooka Y, Itoh A, Hashimoto S, Kawashima H, Hara K, Kanamori A, Ohmiya N, Niwa Y, Goto H. Usefulness of contrast-enhanced transabdominal ultrasonography in the diagnosis of intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol. 2005;100:144–152. doi: 10.1111/j.1572-0241.2005.40726.x. [DOI] [PubMed] [Google Scholar]
- 29.Ohno E, Hirooka Y, Itoh A, Kawashima H, Hara K, Nonogaki K, Kasugai T, Ishikawa T, Ohmiya N, Niwa Y, et al. Usefulness of contrast-enhanced endoscopic ultrasonography (CE-EUS) in the diagnosis of mural nodule of intraductal papillary mucinous neoplasms of the pancreas. the comparison of the ce-eus findings with the pathological findings. Gastrointestinal Endoscopy. 2008;67:AB209. [Google Scholar]
- 30.Zhu Q. Study on contrast enhanced EUS in differential diagnosis of pancreatic tumor. Gastrointestinal Endoscopy. 2009;69:S265. doi: 10.1016/j.gie.2012.02.051. [DOI] [PubMed] [Google Scholar]
- 31.D'Onofrio M, Zamboni G, Tognolini A, Malago R, Faccioli N, Frulloni L, Pozzi Mucelli R. Mass-forming pancreatitis: value of contrast-enhanced ultrasonography. World J Gastroenterol. 2006;12:4181–4184. doi: 10.3748/wjg.v12.i26.4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhutani MS, Hoffman BJ, van Velse A, Hawes RH. Contrast-enhanced endoscopic ultrasonography with galactose microparticles: SHU508 A (Levovist) Endoscopy. 1997;29:635–639. doi: 10.1055/s-2007-1004270. [DOI] [PubMed] [Google Scholar]
- 33.Becker D, Strobel D, Bernatik T, Hahn EG. Echo-enhanced color- and power-Doppler EUS for the discrimination between focal pancreatitis and pancreatic carcinoma. Gastrointest Endosc. 2001;53:784–789. doi: 10.1067/mge.2001.115007. [DOI] [PubMed] [Google Scholar]
- 34.Ueno N, Tomiyama T, Tano S, Wada S, Aizawa T, Kimura K. Utility of endoscopic ultrasonography with color Doppler function for the diagnosis of islet cell tumor. Am J Gastroenterol. 1996;91:772–776. [PubMed] [Google Scholar]
- 35.Rickes S, Unkrodt K, Neye H, Ocran KW, Wermke W. Differentiation of pancreatic tumours by conventional ultrasound, unenhanced and echo-enhanced power Doppler sonography. Scand J Gastroenterol. 2002;37:1313–1320. doi: 10.1080/003655202761020605. [DOI] [PubMed] [Google Scholar]
- 36.Giday SA, Canto MI, Magno P, Buscaglia J, Clarke J, Ko CW, Wroblewski L, Kalloo AN, Kantsevoy SV, Jagannath S. Contrast-enhanced endoscopic ultrasonography (CE-EUS) improves visualization of pancreatic vasculature. Gastrointestinal Endoscopy. 2006;63:AB266. [Google Scholar]
- 37.Okamoto Y, Kawamoto H, Takaki A, Ishida E, Ogawa T, Kuwaki K, Kobayashi Y, Sakaguchi K, Shiratori Y. Contrast-enhanced ultrasonography depicts small tumor vessels for the evaluation of pancreatic tumors. Eur J Radiol. 2007;61:163–169. doi: 10.1016/j.ejrad.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 38.Hocke M, Schulze E, Gottschalk P, Topalidis T, Dietrich CF. Contrast-enhanced endoscopic ultrasound in discrimination between focal pancreatitis and pancreatic cancer. World J Gastroenterol. 2006;12:246–250. doi: 10.3748/wjg.v12.i2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hirooka Y, Itoh A, Kawashima H, Hara K, Nonogaki K, Kasugai T, Ohno E, Ishikawa T, Ohmiya N, Niwa Y, et al. Utility of contrast-enhanced endoscopic ultrasonography (CE-EUS) in the diagnosis of pancreatic diseases using perflubutane microbubbles. Gastrointestinal Endoscopy. 2008;67:AB214. [Google Scholar]
- 40.Sakamoto H, Kitano M, Suetomi Y, Maekawa K, Takeyama Y, Kudo M. Utility of contrast-enhanced endoscopic ultrasonography for diagnosis of small pancreatic carcinomas. Ultrasound Med Biol. 2008;34:525–532. doi: 10.1016/j.ultrasmedbio.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 41.Sofuni A, Iijima H, Moriyasu F, Nakayama D, Shimizu M, Nakamura K, Itokawa F, Itoi T. Differential diagnosis of pancreatic tumors using ultrasound contrast imaging. J Gastroenterol. 2005;40:518–525. doi: 10.1007/s00535-005-1578-z. [DOI] [PubMed] [Google Scholar]
- 42.Ernst H, Nusko G, Hahn EG, Heyder N. Color Doppler endosonography of esophageal varices: signal enhancement after intravenous injection of the ultrasound contrast agent Levovist. Endoscopy. 1997;29:S42–S43. doi: 10.1055/s-2007-1004290. [DOI] [PubMed] [Google Scholar]
- 43.Giday SA, Ko CW, Clarke JO, Shin EJ, Magno P, Jagannath SB, Buscaglia JM, Kantsevoy SV. EUS-guided portal vein carbon dioxide angiography: a pilot study in a porcine model. Gastrointest Endosc. 2007;66:814–819. doi: 10.1016/j.gie.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 44.Ohshima T, Yamaguchi T, Ishihara T, Yoshikawa M, Kobayashi A, Sakaue N, Baba T, Yamada S, Saisho H. Evaluation of blood flow in pancreatic ductal carcinoma using contrast-enhanced, wide-band Doppler ultrasonography: correlation with tumor characteristics and vascular endothelial growth factor. Pancreas. 2004;28:335–343. doi: 10.1097/00006676-200404000-00024. [DOI] [PubMed] [Google Scholar]
- 45.Lassau N, Brule A, Chami L, Benatsou B, Péronneau P, Roche A. [Evaluation of early response to antiangiogenic treatment with dynamic contrast enhanced ultrasound] J Radiol. 2008;89:549–555. doi: 10.1016/s0221-0363(08)71480-x. [DOI] [PubMed] [Google Scholar]
- 46.Lyshchik A, Fleischer AC, Huamani J, Hallahan DE, Brissova M, Gore JC. Molecular imaging of vascular endothelial growth factor receptor 2 expression using targeted contrast-enhanced high-frequency ultrasonography. J Ultrasound Med. 2007;26:1575–1586. doi: 10.7863/jum.2007.26.11.1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Palmowski M, Huppert J, Ladewig G, Hauff P, Reinhardt M, Mueller MM, Woenne EC, Jenne JW, Maurer M, Kauffmann GW, et al. Molecular profiling of angiogenesis with targeted ultrasound imaging: early assessment of antiangiogenic therapy effects. Mol Cancer Ther. 2008;7:101–109. doi: 10.1158/1535-7163.MCT-07-0409. [DOI] [PubMed] [Google Scholar]
- 48.Willmann JK, Lutz AM, Paulmurugan R, Patel MR, Chu P, Rosenberg J, Gambhir SS. Dual-targeted contrast agent for US assessment of tumor angiogenesis in vivo. Radiology. 2008;248:936–944. doi: 10.1148/radiol.2483072231. [DOI] [PMC free article] [PubMed] [Google Scholar]