Abstract
Background:
Minimally invasive surgery has become increasingly utilized in the trauma setting. When properly applied, it offers several advantages, including reduced morbidity, lower rates of negative laparotomy, and shortened length of hospital stay. The purpose of this study was to evaluate the role of laparoscopy in the management of trauma patients with penetrating abdominal injuries.
Methods:
We conducted a 3-year retrospective chart review of 4541 trauma patients admitted to our urban Level II trauma center. Penetrating abdominal injuries accounted for 209 of these admissions. Patients were divided into 3 treatment groups based on the characteristics of their abdominal injuries. Management was either observation, immediate laparotomy, or screening laparoscopy.
Results:
Thirty-three patients were observed in the Emergency Department based on their initial physical examination and radiologic studies. After Emergency Department evaluation, 154 patients underwent immediate laparotomy. In this group, 119 therapeutic laparotomies, 11 nontherapeutic laparotomies, and 24 negative laparotomies were performed. A review of the negative laparotomies revealed that possibly 8 of 10 gun shot wounds and all 14 stab wounds could have been done laparoscopically. Twenty-two patients underwent laparoscopic evaluation, 9 of which were converted to open procedures.
Conclusion:
Minimally invasive surgical techniques are particularly helpful as a screening tool for anterior abdominal wall wounds and lower chest injuries to rule out peritoneal penetration. Increased use of laparoscopy in select patients with penetrating abdominal trauma will decrease the rate of negative and nontherapeutic laparotomies, thus lowering morbidity and decreasing length of hospitalization. As technology and expertise among surgeons continues to improve, more therapeutic intervention may be done laparoscopically in the future.
INTRODUCTION
Minimally invasive surgical techniques have become increasingly utilized in all areas of surgery. Current use of laparoscopy in the evaluation and management of trauma patients has been a natural extension of this trend. Several studies1–3 have analyzed various aspects of its application to the trauma patient. Although utilized for both blunt and penetrating injuries, laparoscopy has gained the most widespread acceptance as a useful tool in the management of patients with penetrating abdominal injuries. Its ability to accurately determine anterior peritoneal penetration from stab and gunshot wounds has been proven. Others2,3 have expanded its role beyond simply a screening tool for injury, to its current use in some centers as a diagnostic and therapeutic modality.
The purpose of this study was to evaluate the role of laparoscopy in the trauma setting at our urban Level II trauma center. More specifically, we examined its use in the management of hemodynamically stable trauma patients with penetrating anterior abdominal injuries. We also sought to determine how our results compared with those of other centers regarding the widely accepted laparoscopic advantages of reduced morbidity, decreased rates of negative laparotomy, and shortened length of hospital stay (LOS).
METHODS
We conducted a retrospective chart review of 4541 trauma patients who were admitted to our Level II trauma center between July 1, 1999 and July 31, 2002. Penetrating injuries accounted for 817 (18%) of these trauma admissions. There were 209 penetrating injuries isolated to the abdomen, of which 116 were gunshot wounds (GSW) and 93 were stab wounds (SW).
Patients were divided into 3 groups based on their management. The first group consisted of hemodynamically stable patients without evidence of abdominal peritoneal penetration based on physical examination, local wound exploration, or further confirmatory studies, including focused abdominal sonography for trauma (FAST), computed axial tomography (CT), or diagnostic peritoneal lavage (DPL), or all of these. The additional confirmatory studies were not applied in a standard fashion to all patients, but rather selected based on clinical indication and attending physician preference. These patients were admitted for observation without therapeutic intervention. In addition, stab wounds with peritoneal penetration, but no peritoneal signs, also underwent a course of observation.
The second group of patients was those with peritoneal signs or confirmed evidence of abdominal peritoneal penetration based on physical examination, local wound exploration, or further confirmatory studies. These patients underwent immediate laparotomy.
The third group of patients was taken to the operating room for laparoscopic evaluation due to questionable peritoneal penetration. Criteria for laparoscopy was a hemodynamically stable patient with an injury trajectory suggestive of peritoneal penetration that could not reliably be ruled out based on physical examination or further confirmatory studies. Laparoscopy is used as a screening tool for peritoneal penetration at our institution. Conversion to laparotomy was performed if peritoneal penetration was confirmed laparoscopically. No attempt was made to laparoscopically assess the extent of the intraabdominal injuries or make therapeutic interventions.
Intraoperative findings were described using standard terminology. Laparotomy was negative if it was discovered after the abdomen was opened that no peritoneal penetration had occurred. A nontherapeutic laparotomy was one that confirmed peritoneal penetration with either no intraabdominal injuries or injuries so minor that they did not require surgical repair. The patients in these 2 groups were closed without therapeutic intervention and admitted to the floor for postoperative recovery. A therapeutic laparotomy was one that necessitated surgical repair of internal injuries.
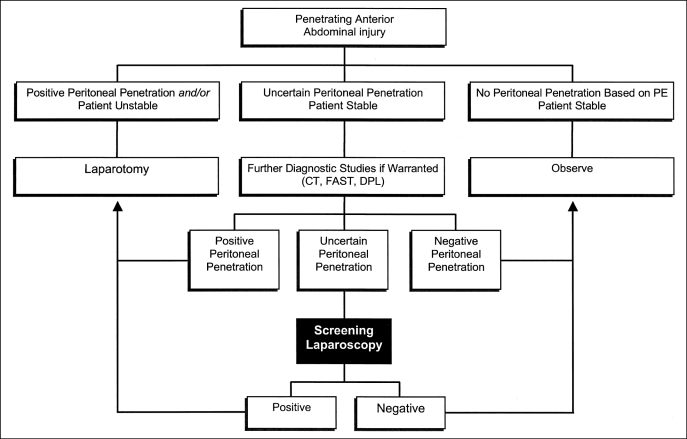
The laparoscopic findings were described as either positive or negative based on evidence of peritoneal penetration. Patients with positive findings at laparoscopic evaluation were converted to open procedures. These converted laparotomies were subsequently described as therapeutic or nontherapeutic. Figure 1 details the algorithm used for management of our patients with penetrating abdominal wounds.
Figure 1.
Algorithm for management of penetrating abdominal trauma.
Injury Severity Score (ISS) and length of hospital stay (LOS) were calculated for each patient in the study. Morbidity and mortality figures were also generated for each patient from our computer database by using standard methodology to define associated complications.
RESULTS
Penetrating abdominal injuries accounted for 209 of our trauma admissions, of which 116 were GSW and 93 were SW. Gender breakdown of these patients was male, 171 (82%) and female, 38 (18%). Mean age for all patients in the study was 32.8 years.
Thirty-three patients (GSW=9, SW=24) were observed in the Emergency Department based on their initial physical examination, radiologic studies, or additional confirmatory studies, or all of these. As expected, most of these patients had SW. The majority of the GSW patients received immediate laparotomies due to the higher ballistic forces associated with these injuries. In general, GSW to the anterior abdomen required laparotomy unless the wound was tangential. Mean ISS for the observation group was 3.8. To our knowledge, no injuries were missed.
After Emergency Department evaluation, 154 patients underwent immediate laparotomy. Table 1 provides the negative, nontherapeutic, and therapeutic outcomes in the formal laparotomy group with regards to the number and percentage of procedures and LOS for patients with GSW and SW. Laparotomy patients had a mean ISS of 13.6. A review of the negative laparotomies revealed that possibly 8 of 10 GSW and all 14 stab wounds could have been done laparoscopically, based on the location of the entrance wound in the anterior abdominal wall. However, 2 of the negative GSW laparotomies assessed tangential wounds that would not have been well visualized by laparoscopy alone.
Table 1.
Results of Formal Laparotomy Group
| GSW* (n = 100) |
SW† (n = 54) |
|||||
|---|---|---|---|---|---|---|
| # | % | LOS‡ | # | % | LOS | |
| Negative | 10 | 10 | 3.5 | 14 | 26 | 4.6 |
| Nontherapeutic | 4 | 4 | 3.5 | 7 | 13 | 5 |
| Therapeutic | 86 | 86 | 10.1 | 33 | 61 | 6.2 |
GSW = Gunshot wound.
SW = Stab wounds.
LOS = Length of hospital stay.
Twenty-two patients underwent laparoscopic evaluation (GSW=7, SW=15). All of these patients had anterior abdominal wounds, and 2 patients had flank wounds in addition to the anterior wounds. Of these 22 patients, 7 had an additional confirmatory test prior to going to the operating room (Table 2). One GSW was converted to an open procedure, and 6 had laparoscopy only. Eight SW were converted to an open procedure, and 7 had laparoscopy only (Table 3). Table 4 provides the results of laparotomies after conversion for GSW and SW patients. No procedure-related complications occurred with the laparoscopy group of patients. Mean ISS for the laparoscopic group was 6.4.
Table 2.
Additional Confirmatory Test in Patients Managed With Laparoscopy*
| GSW | CT scan—rule out rectal injury |
| GSW | FAST and CT scan-GSW to chest, bullet near diaphragm |
| SW | FAST—stab near diaphragm r/o pericardial effusion |
| SW | FAST—pregnant |
| SW | FAST and DPL—lower chest r/o pericardial effusion and hollow viscus injury |
| SW | CT scan—rule out foreign body |
| SW | FAST |
GSW = Gunshot wound; CT = Computed tomography; FAST = Focused abdominal sonography for trauma; SW = Stab wounds; LOS = Length of hospital stay.
Table 3.
Results of Laparoscopy Group
GSW = Gunshot wound.
SW = Stab wounds.
Table 4.
Results of Laparotomies After Conversion
GSW = Gunshot wound.
SW = Stab wounds.
Table 5 lists the number and percentage of GSW and SW patients who underwent laparotomy, laparoscopy, or were observed. Morbidity and mortality figures were also analyzed. Mortality was 13% (GSW=20, SW=0) for the laparotomy group, and 0% (GSW=0, SW=0) for the laparoscopy group. Morbidity was 27% (GSW=42, SW=7) in the laparotomy group and 14% (GSW=1, SW=2) in the laparoscopy group. These numbers reflect the increased severity of injury with the laparotomy group. However, we found no difference in morbidity or mortality when we compared data for the negative laparotomy group and the negative laparoscopy group. No deaths or procedure-related complications occurred in either group.
Table 5.
Management of Gunshot Wounds Versus Stab Wounds
| Laparotomy | Observed | Laparoscopy | |
|---|---|---|---|
| Gunshot wound | 100 (86.2%) | 9 (7.8%) | 7 (6.0%) |
| Stab wound | 54 (58.1%) | 24 (25.8) | 15 (16.1%) |
Mean LOS was 7.9 days for the laparotomy patients and 3.0 days for the laparoscopy patients. This difference can be attributed to the higher severity of injury associated with the laparotomy group. However, a more useful comparison of LOS is that between the negative laparotomy group and the negative laparoscopy group, which revealed an LOS of 4.1 and 1.9, respectively.
DISCUSSION
Laparoscopic evaluation of the peritoneal cavity is not a new concept, having first been described by Kelling4 over a century ago. The first reports demonstrating the utility of laparoscopic surgery in the evaluation of trauma patients were published soon thereafter in the 1920s.5,6 These early trauma studies investigated laparoscopy as a method to diagnose internal bleeding in patients with traumatic abdominal injuries. Reports describing similar experiments were published sporadically throughout most of the last century. However, mainly due to technological limitations, it would be many years before laparoscopic surgical techniques would prove their practical utility and gain widespread acceptance. It is now evident that despite the lack of early enthusiasm in the surgical community for these new techniques, the laparoscopic pioneers correctly recognized the potential benefits of minimally invasive surgery in the trauma patient.
Recent technologic advances in optics and laparoscopic instrumentation have greatly broadened the applications for minimally invasive surgery. We now have a better understanding of the physiologic changes and complications associated with these procedures. Laparoscopic equipment is currently a standard part of every modern operating room. With increased training and utilization of minimally invasive procedures in all areas of surgery has come an increase in expertise among trauma surgeons. These techniques have evolved from what was once a novelty into an important part of every surgeon's practice. For trauma patients, laparoscopy provides clear visualization of the peritoneal space and anterior abdominal wall, and unlike other diagnostic modalities, has the additional benefit of potential for therapeutic intervention.
However, despite its increased use in trauma, the optimum role of laparoscopy in this setting has not yet been clearly defined. There continues to be variation among trauma centers on how best to optimize its application, taking full advantage of its benefits while overcoming its limitations. Laparoscopy has been used as a screening, diagnostic, and therapeutic tool to evaluate both blunt and penetrating trauma at various centers. Villavicencio and Aucar1 authored an extensive review in 1997 in which they compared outcomes collected from 37 separate studies, involving over 1900 patients. A review of the data showed that it was most useful as a screening tool, missing only 1% of injuries and preventing 63% of patients from unnecessary laparotomies. The data were less encouraging when laparoscopy was used as a diagnostic tool, with missed injury rates reported between 41% and 77%. These numbers reflect a diagnostic accuracy that is unacceptable to most surgeons who have used the laparoscope less frequently in this manner.7 Laparoscopy is infrequently used as a therapeutic tool; however, several reports have demonstrated favorable results with laparoscopic repair of a variety of intraabdominal injuries, including the dia-phragm, liver, gallbladder, spleen and bowel.3 We currently use the laparoscope as a screening tool only.
Emergency department evaluation of the injured patient has evolved greatly over the years, based mainly on the technology of the time. Trauma surgeons have had available a variety of diagnostics tools to assist with the management of their patients, including DPL, FAST, and CT. The increased availability of laparoscopy now offers them even more flexibility during the workup of injured patients. Each of these modalities has advantages and disadvantages that must be considered.
Certainly the evaluation of every trauma patient starts with the advanced trauma life support (ATLS) primary survey followed by a thorough physical examination. It is important to carefully inspect the patient's wounds, because findings on the initial physical assessment usually determine the decision-making algorithm. Local wound exploration is limited in its ability to determine specific intraabdominal injuries, but it can often determine peritoneal penetration and thereby avoid the need for further studies. In patients who are obtunded due to central nervous system dysfunction or intoxication as well as in those with distracting injuries to multiple body systems, the physical examination may be less reliable. Wounds with tangential trajectories can also be difficult to accurately assess, necessitating additional diagnostic studies.
Diagnostic peritoneal lavage is simple, inexpensive, and can be quickly performed in the emergency department. However, DPL is limited by poor specificity, inability to accurately assess the retroperitoneum, and potential for missed hollow viscus or diaphragmatic injuries.8 It is also an invasive test that has some risk, albeit low, for procedural complications. Although DPL has been considered the standard modality to assess traumatic intraabdominal injury for many years, its use is now declining in favor of more accurate, less invasive modalities, such as ultrasound (FAST) and CT.8–10 We have significantly decreased the number of DPLs performed at our institution in recent years as well, relegating its use to screening for late presenting potential hollow viscus injuries or rapid evaluation of blunt injuries if FAST is unequivocal or unavailable.
Technological improvements have greatly enhanced the capabilities of CT and ultrasound, both of which now have an important role in trauma management. FAST is now widely used in most trauma centers; however, its major role is in blunt trauma. It has a low specificity for organ injury, but can effectively determine the presence of free fluid in the gravity dependent spaces of the peritoneal cavity. Some centers have used positive FAST examination findings as an indicator for laparotomy in penetrating trauma.11 Its main utility in penetrating injuries is rapid evaluation of the pericardium.
Improvements in CT speed and resolution have allowed for reliable evaluation of both the peritoneum and retroperitoneum. CT findings can often confirm or rule out peritoneal penetration based on a more clearly delineated wound trajectory or evidence of intraabdominal injury.12,13 Unlike blunt injuries that can often be managed by observation and monitoring, CT confirmation of penetrating intraabdominal injury warrants laparotomy at our institution.
The results of our study were consistent with those of other centers regarding the generally accepted laparoscopic advantages of decreased rates of negative laparotomy, shortened length of hospital stay, and quicker return to normal activity. We found overall that the laparotomy patients had both higher morbidity and mortality. The laparotomy patients had many more pulmonary complications including atelectasis, pneumonia, and respiratory failure. They also were found to have more wound complications including dehiscence, infection, and abscess formation. The decreased mobility of the laparotomy patients led to one deep vein thrombosis in this group. The results of our study did not show any difference in morbidity or mortality between the negative laparoscopy and the negative laparotomy groups. Other studies have shown these rates to be lower in the laparoscopy group.14 We found that a decrease occurred in LOS from 4.1 days in the negative laparotomy group to 1.9 days in the negative laparoscopy group.
Studies have reported decreased rates of negative trauma laparotomy with efficient use of laparoscopy. Brandt et al15 looked at 21 trauma patients who underwent laparoscopic evaluation of both penetrating and blunt injuries, and found that emergency laparoscopy was 100 percent accurate in determining the need for laparotomy. They determined that 9 patients avoided unnecessary laparotomy based on the laparoscopic screening. A more recent retrospective review16 demonstrated a direct correlation between increased use of laparoscopy and decreased rates of negative laparotomy. Our study revealed that laparoscopic evaluation spared many patients unnecessary laparotomies. After reviewing the operative reports of patients with negative laparotomies, it was determined that possibly 8 of 10 GSW and all 14 stab wounds could have been done laparoscopically. Two of the 10 GSW patients had lateral or posterior injuries that required a more detailed evaluation of the retroperitoneum than would have been possible by laparoscopy alone.
Although we currently use the laparoscope solely as a screening tool for peritoneal penetration, the next logical progression for us is to conduct a more effective laparoscopic evaluation of specific organ structures in the trauma setting. This could potentially decrease or eliminate the conversions from laparoscopy to laparotomy that were nontherapeutic. This would entail a systematic laparoscopic evaluation of the entire peritoneal cavity, including running the small bowel, visualizing the diaphragm and solid organs, and accurately assessing for evidence of pelvic or retroperitoneal injury. The threshold for conversion would vary among surgeons based on laparoscopic expertise and confidence in the laparoscopic examination. The next step is more therapeutic intervention as we gain more experience.
CONCLUSION
Current trends in all areas of surgery are towards less invasive techniques. Data show that laparoscopy is a useful modality for evaluating and managing trauma patients with penetrating injuries. We have found that it is particularly helpful as a screening tool for anterior abdominal wall wounds and lower chest injuries to rule out peritoneal penetration. Increased use of laparoscopy in select patients with penetrating abdominal trauma will decrease the rate of negative and nontherapeutic laparotomies, thus lowering morbidity, decreasing length of hospitalization, and provide for more efficient utilization of available resources. As technology and expertise among surgeons continues to improve, more standard therapeutic interventions may be done laparoscopically in the future.
Footnotes
Disclosure: The authors have no financial interest in any commercial device, equipment, instrument, or drug that is a subject of this article. No financial support was provided nor do conflicts of interest exist.
References:
- 1. Villavicencio RT, Aucar JA, Analysis of laparoscopy in trauma. J Am Coll Surg. 1999;189:11–20 [DOI] [PubMed] [Google Scholar]
- 2. Smith RS, Fry WR, Morabito DJ, et al. Therapeutic laparos-copy in trauma. Am J Surg. 1995;170:632–637 [DOI] [PubMed] [Google Scholar]
- 3. Zantut LF, Ivatury RR, Smith RS, et al. Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma: A multicenter experience. J Trauma. 1997;42:825–831 [DOI] [PubMed] [Google Scholar]
- 4. Litynski G. Laparoscopy- the early attempts: spotlighting Georg Kelling and Han Christian Jacobaeus. JSLS. 1997;1:83–85 [PMC free article] [PubMed] [Google Scholar]
- 5. Short AR. The uses of celioscopy. BMJ. 1925;2:254–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stone WE. Intra-abdominal examination by the aid of the peritoneoscope. J Kansas Med Soc. 1924;24:63–65 [Google Scholar]
- 7. Ivatury RR, Simon RJ, Stahl WM. Acritical evaluation of laparoscopy in penetrating abdominal trauma. J Trauma. 1993;34: 822–828 [DOI] [PubMed] [Google Scholar]
- 8. Catre MG. Diagnostic peritoneal lavage versus abdominal computed tomography in blunt abdominal trauma: a review of prospective studies. Can J Surg. 1995;38:117–122 [PubMed] [Google Scholar]
- 9. Fernandez L, McKenney MG, McKenney KL, et al. Ultra-sound in blunt abdominal trauma. J Trauma. 1998;45:941–948 [DOI] [PubMed] [Google Scholar]
- 10. Scalea TM, Rodriguez A, Chiu WC, et al. Focuses assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466–472 [DOI] [PubMed] [Google Scholar]
- 11. Udobi KF, Rodriguez A, Chiu WC, et al. Role of ultrasonography in penetrating abdominal trauma: a prospective clinical study. J Trauma. 2001;50:475–479 [DOI] [PubMed] [Google Scholar]
- 12. Chiu WC, Shanmuganathan K, Mirvis SE, et al. Determining the need for laparotomy in penetrating torso trauma: a prospective study using triple-contrast enhanced abdominopelvic computed tomography. J Trauma. 2001;51:860–869 [DOI] [PubMed] [Google Scholar]
- 13. Soto JA, Morales C, Munera F, et al. Penetrating stab wounds to the abdomen: use of serial US and contrast-enhanced CT in stable patients. Radiology. 2001;220:365–371 [DOI] [PubMed] [Google Scholar]
- 14. Sosa JL, Baker M, Puente I, et al. Negative laparotomy in abdominal gunshot wounds: Potential impact of laparoscopy. J Trauma. 1995;38:194–197 [DOI] [PubMed] [Google Scholar]
- 15. Brandt CP, Priebe PP, Jacobs DG. Potential of laparoscopy to reduce non-therapeutic trauma laparotomies. Am Surg. 1994;60:416–420 [PubMed] [Google Scholar]
- 16. Simon RJ, Rabin J, Kuhls D. Impact of increased use of laparoscopy on negative laparotomy rates after penetrating trauma. J Trauma. 2002;53:297–302 [DOI] [PubMed] [Google Scholar]