Abstract
Background
Offset in THA correlates to abductor muscle function, wear, and impingement. Femoral offset after THA is not independent of the cup center of rotation (COR) so hip offset, a combination of femoral offset and change in hip COR, becomes the important measurement.
Questions/purposes
We therefore asked whether hip offset in arthritic hips would correlate with cup COR; whether offset could always be balanced within 6 mm of contralateral normal hips; and whether hip length could also be kept within 6 mm.
Methods
We compared hip offset of arthritic and contralateral normal hips on radiographs in 82 patients (82 hips) who had THA. We used computer navigation in all patients with the aim of reconstructing the hip offset and to compare hip offset change to the quantitative change of the hip COR.
Results
The preoperative radiographic change to equalize the offset ranged from −12 to +21 mm (mean, 1.5); postoperatively the change was 1.4 ± 6.4 mm and was within ± 6 mm in 78 of 82 hips. As COR displaced superiorly from 3 to 6+ mm the offset had to be substantially increased. Only with COR 0–3 mm superior and 0–5 mm medial was offset always within 5 mm.
Conclusions
Hip offset reconstruction was directly related to the position of the hip COR, and navigation allowed quantitative control of offset and hip length.
Introduction
The principle of total hip arthroplasty (THA) is to recreate the correct articulation of the hip which has become destroyed by arthritis. The arthritic hip has loss of cartilage which causes the femoral head to slide and migrate away from the normal hip center of rotation (COR) [23]. One technical goal of the THA operation is to restore the femoral head COR into the acetabular COR as closely as possible to normal with the new articulation surface. When the centers are not restored near normal, there is decreased abductor function [1, 9, 17], increased wear [13, 24], and loosening of implants [6, 10, 18, 19, 26–28]. Femoral offset, the perpendicular distance from the COR of the femoral head to the axis of the femur, is an important reflection of the displacement of the femur from the pelvis. However, in THA the acetabular COR is changed by reaming and cup implantation. Therefore, femoral offset no longer represents the displacement of the femur from the pelvis—the displacement is influenced by both femoral offset and cup COR (two authors have named this change in cup COR as “cup offset” [12, 15]). The important measure of offset incorporates both the cup and femur, and we call this “hip offset” and define it as the perpendicular distance from the teardrop through the femoral head COR to the axis of the femur (Fig. 1). Perhaps the most common method used to intraoperatively measure offset has been the pin method, which measures the displacement of the femur from the pelvis before and after reconstruction so that it is a measure of hip offset [3]. The combination of femoral offset and cup COR (hip offset) has been measured in previous clinical [4, 15, 17, 25] and computer modeling studies [12].
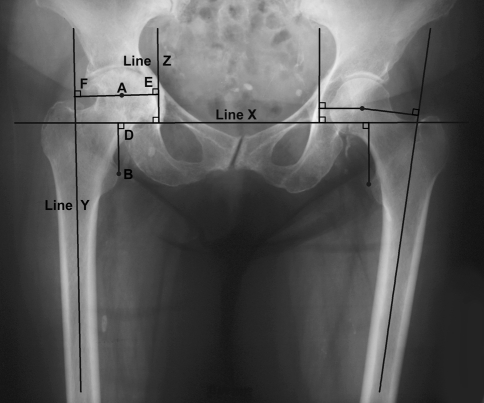
Fig. 1.
The method for measuring hip length and hip offset is shown. Point A is the center of the femoral head, point B is the apex of the lesser trochanter, and line Y is the anatomic axis of the femur. Hip offset is measured as follows: Line X is the transteardrop line with line Z drawn through the teardrop perpendicular to the transteardrop line. A perpendicular line between line Y and line Z through the femoral head hip center (point A) is the hip offset, ie, AE plus AF. Hip length is measured from the apex of the lesser trochanter, point B, perpendicular to the transteardrop line X, line BD.
Computer navigation provides a method to quantitatively measure the COR intraoperatively and correlate its restoration to that of hip offset. Offset is particularly important because it can be difficult to balance with leg length. Leg length can almost always be corrected by the use of different modular heads, but this also affects offset. When the COR of the hip is moved superiorly by 5 mm or more, achieving offset which does not cause impingement often requires a high offset stem [2, 4, 24]. However, when offset is increased by more than 5 mm there is an increase in wear [13]. One study measured as little as 2 mm radiographic change of COR as being the most important technical factor for loosening of the cup [10]. In patients with congenital disease of the hip (DDH), elevation of COR caused limping and loosening [6, 18, 26]. Because change in COR and offset have been correlated to THA failure [6, 10, 18, 19, 26, 27], we wondered whether the amount of change of COR correlated with amount of change in offset.
Therefore, (1) we investigated the influence of COR on restoration of hip offset; (2) we asked how often the offset could be controlled within 6 mm of a normal hip; and (3) because offset and length are interrelated, we asked whether the hip length could also be restored within 6 mm.
Patients and Methods
We performed primary THA in 121 patients with 129 hips between March 2007 and November 2007. Eighty-two of these patients had unilateral hip arthritis and these formed the study group. Each patient was operated with an imageless computer navigation system (Navitrack®; ORTHOsoft, Inc, Montreal, Canada). The diagnosis in 79 of 82 hips was osteoarthritis, two had developmental disease of the hip, and one had osteonecrosis. Thirty-seven were men with a mean (± SD) age of 60.7 ± 9.69 years, and 45 were women with a mean age of 65.2 ± 11.6 years. Mean weight was 85.1 ± 23.9 kg and mean height was 174 ± 20.5 cm (mean body mass index, 28.3 ± 4.6). All patients were followed up to 1 year postoperatively, with clinical data evaluated for impingement pain, muscle strength, and dislocation, which directly relate to hip offset. The data were studied retrospectively under Institutional Review Board approval for retrospective studies. All patients signed consent for use of the data obtained at their operations.
Clinical evaluations were performed on 76 patients (76 hips) because six hips had a revision of a Durom® cup (Zimmer, Inc, Warsaw, IN) caused by product failure [14]. Postoperatively patients followed the same clinical protocol. We used no dislocation precautions. Pain was evaluated with a Harris hip score [7]. Muscle strength was grossly evaluated by the necessity for an assistive device and limp. Clinical signs of impingement were determined by dislocation or impingement pain. Operations were performed through a mini-posterior incision by the same surgeon (LDD) [5]. Implants used were the noncemented anatomic porous replacement stem (APR®; Zimmer) in 65 hips; the Zweymüller™ Alloclassic® (Zimmer) in 14 hips; and a cemented Apollo® stem (Zimmer) in three hips. Acetabular components in 70 hips were the Converge® with a Durasul® highly crosslinked polyethylene liner (Zimmer); and 12 hips had a Durom® metal-on-metal cup (Zimmer).
Two of us (MD, ZW), who were not involved in patient care, made all radiographic measurements on AP pelvic radiographs preoperatively and 6 weeks postoperatively. Both legs were internally rotated 15° (preoperatively the arthritic leg rotated as much as possible up to 15°) [9]. Magnification was corrected on postoperative radiographs using the acetabular component size and femoral head diameter; on preoperative radiographs, it was corrected by comparing the preoperative and postoperative radiographic femoral shaft diameters at a fixed 10 cm distal to the proximal corner of the lesser trochanter.
Measurements of offset were made as hip offset and not as femoral offset. Because our patients had one hip that was normal, the hip offset of the normal and arthritic hips were measured preoperatively for the change of the arthritic hip necessary at THA surgery to create a correct hip offset (Fig. 1). Postoperatively, at the 6 week postoperative followup, the hip offset of the reconstructed hip was measured on radiographs by the same method for the change accomplished at surgery and for any discrepancy between reconstructed and the normal hip. Computer navigation is a precise quantitative measurement of the overall change of the femur in relationship to the pelvis [22]. We were aware that hip offset is not always symmetrical: one hip may have a greater offset than that of the contralateral hip in the same patient. The mean difference between normal hips in one study was 2.54 ± 2.31 mm [11]. In hips with asymmetrical offset the normal cannot be compared to the arthritic without accounting for the magnitude of the asymmetry (Fig. 2). Sometimes, both hips are arthritic (different than this study) and the change needed to restore the two CORs at surgery cannot be measured by comparing a normal to the arthritic hip. We developed a new radiographic method for measuring preoperative quantitative target change for hip length and offset when the contralateral hip was not normal, as well as with severe pelvic rotation (Fig. 3).
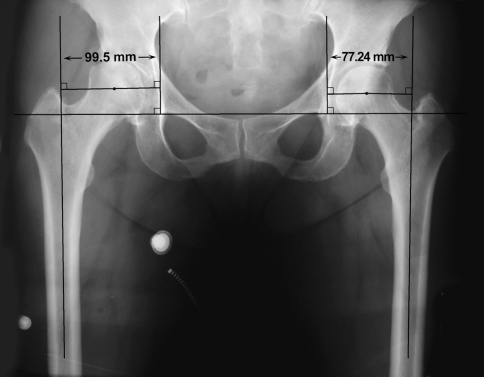
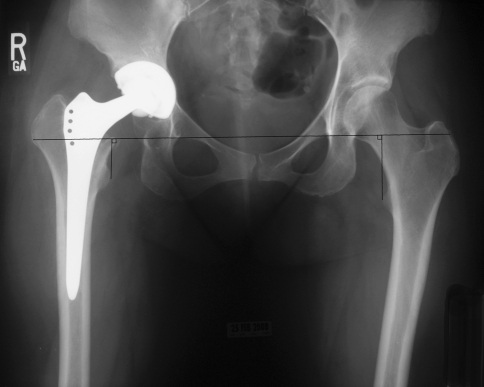
Fig. 2.
Preoperative AP pelvis radiograph shows hips with asymmetrical offset. The arthritic hip has femoral head migration of 5.56 mm in the horizontal direction which means the radiographic anatomic asymmetry is 16.7 mm.
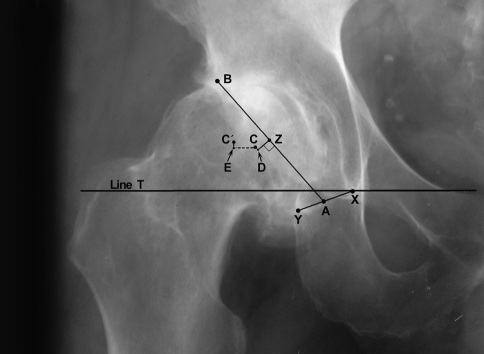
Fig. 3.
Line T designates the transteardrop line. Line XY designates the transverse acetabular ligament. The mouth of acetabulum is from the midpoint of Line XY (point A) to the superior-lateral cortical rim of the acetabulum excluding osteophytes (point B). Point Z marks the midpoint of Line AB. Line ZD is 7 mm lateral and perpendicular to point Z. The center of the acetabulum (point C) is 1 mm cranial to point D. The center of the femoral head (F) was determined by using a transparent template with concentric circles. Line CE is drawn parallel to the transteardrop line from point C to point F. The change necessary to make the centers of rotation C and F coincide in the lateral direction (offset) is Line CE and the vertical direction (hip length) is Line FE.
Biomechanical reconstruction of the hip requires that both the offset and length of the hip are restored. With an opposite normal hip, restoration of the radiographic hip length gives equal leg length. Radiographic measurements of length of the hip were obtained by measuring the perpendicular distance from the transteardrop line to the apex of the lesser trochanter [15, 20] (Fig. 1). We measured radiographic hip lengths [15] separate from clinical leg lengths. Clinical leg lengths were measured intraoperatively in all 82 hips in the supine position after the induction of anesthesia to provide muscle relaxation of any muscle contracture. Legs were compared in the axis of the body (a line referencing the center of the sternum and bisecting the pelvic anterior iliac spines) with both legs elevated 30° to eliminate the effect of flexion contracture in the arthritic hip. The difference in the level of the bony prominence of the medial malleoli was measured as the leg length difference. This measurement was repeated for clinical leg lengths at the completion of the operation.
Intraoperatively the bony anatomic acetabular COR was determined by the software of computer navigation from data generated by the surgeon touching the acetabular bone 16 times with a pointer with an attached array. The 16 points must not be taken on osteophytes. The software calculates a best fit COR from the points and since the points are not taken on osteophytes, the deformity of the acetabulum by arthritis causes little distortion of the correct COR. The change in COR with reaming and cup implantation is measured in the cephalocaudad direction (vertical) and the mediolateral direction (horizontal). In our operations the COR was always moved superior (cephalad) and medial. Intraoperatively there were two methods used for computer navigation measurement of the hip offset. For both methods, a pelvic tracker was attached to the pelvic brim with three threaded pins. The measurement before and after reconstruction of the hip required the leg be placed in exactly the same location. One method used a fixed array attached to the distal lateral femur by three pins (Fig. 4A). The software identified the leg position for the initial measurement and after reconstruction. The accuracy of the distal femoral fixed array for hip offset and length was validated by Renkawitz et al. [22] in 17 cadaver hips using CT scans and imageless navigation. The second method used a 3.5-mm screw into the greater trochanter as the locator for the navigation software before and after reconstruction (Fig. 4B). The technique required the leg to be in the same position, which was performed by overlaying the operated leg onto the contralateral leg aligning the patellae and soles of the heels. To give optimal reproduction of the leg position, the same assistant aligned the legs before and after reconstruction. A pointer guide with optical trackers touched the depression in the screw head for each measurement. The fixed array to the distal femur was used as the standard and the results with the screw into the greater trochanter were validated by comparing it to the distal fixed array. Manual measurement of hip offset was performed by the clearance by one fingerbreadth of the lesser trochanter from the ischium in full extension; the greater trochanter from the ilium in abduction and external rotation; and clearance of the trochanter from the ilium anteriorly in full flexion-internal rotation.
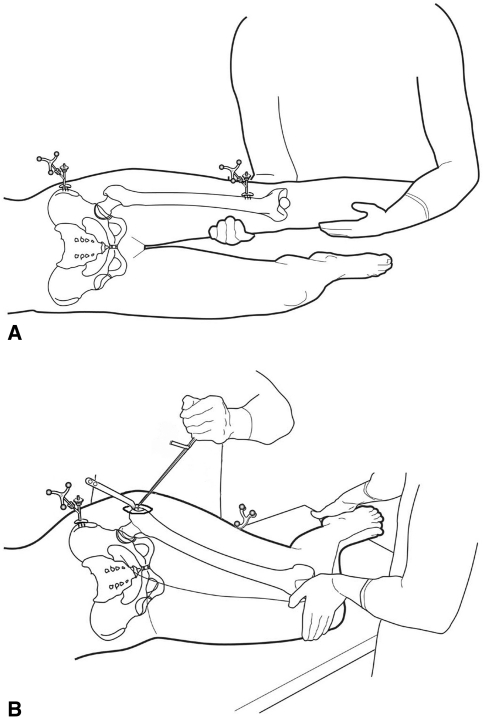
Fig. 4A–B.
(A) A diagram shows the use of the femoral tracker array for leg length and offset. Leg position is monitored by the software to be exactly duplicated after reconstruction. (B) A diagram shows femur registration using a screw in the greater trochanter. The pointer touches the depression of the screw head for the measurement before and after reconstruction. The same surgical assistant positions the legs by aligning the patellae and heels of the feet.
Hip length was measured with computer navigation using the same methods described for hip offset. Manually, hip length was confirmed by overlaying the two legs as described for the screw technique of computer navigation measurement (Fig. 4B).
The Kolmogorov-Smirnov test was used to determine whether the data were normally distributed. For each hip, the offset measurements were given as mean and SD and the discrepancy between the arthritic and normal hip was the mean of individual differences. The paired t test was used to compare offset (and hip length) measured by the two methods of femoral tracking to the reference value of radiographic change. Statistical analysis used SPSS® software (SPSS Inc, Chicago, IL).
Results
In 76 hips (76 patients) with clinical evaluation (6 hips had Durom® cup), the Harris hip pain score at 1 year was 42 ± 5.6 versus a preoperative score of 19.9 ± 5.6. Two patients used a cane and both were over 80 years of age with balance problems. One patient with a dysplastic hip had a radiographic hip length difference of 1.7 mm, but used a shoe lift because of a clinical leg length difference of 10 mm caused by pelvic obliquity from scoliosis. No patient had impingement pain or a dislocation.
The hip offset radiographic measurements showed greater change than was observed with intraoperative navigation (1.5 mm versus 0.1 mm) (Table 1) which represents radiographic rotational and magnification errors. The extremes of the range of change of hip offset are because of the wide variability of migration of the femoral head which can be superolateral (which requires a reduction of offset) to a medial protrusion position (which requires an increase in offset). Postoperatively the radiographic offset discrepancy from the normal hip was 1.7 ± 5 mm (range, −10.6 to 13.1 mm) which was nearly the same as the desired preoperative change of 1.5 mm. Seventy-eight of 82 hips (95%) had a postoperative radiographic offset discrepancy within 6 mm.
Table 1.
Hip offset radiographic measurements
| Measurement (mm) | Preoperative discrepancy | Postoperative change |
|---|---|---|
| Hip rad | 1.5 ± 5.6* (range, −11.7 to 21.4) | 1.4 ± 6.4 (range, −12.7 to 15.3) |
| Hip nav troch | 0.1 ± 5.1 (range, −11 to 13) | |
| Hip nav femur+ | −0.7 + 7.9 (range, −24 to 17) |
mm = millimeters; hip rad = hip radiographs; hip nav troch = hip navigation by trochanteric screw; hip nav femur = hip navigation by distal femoral pins with array;
* = target change in offset to be obtained at surgery; + = no statistical difference between the two measurements by navigation.
The preoperative discrepancy in hip lengths (radiographic) and leg lengths (clinical) were corrected (Table 2). Eighty-one of 82 hips (99%) had a radiographic discrepancy of 6 mm or less. The intraoperative measure of leg length difference was the most reliable number to use for change of length at surgery in these patients with a normal contralateral hip. Radiographic measurements are distorted by rotation and magnification.
Table 2.
Hip length discrepancy
| Measurement (mm) | Preoperative discrepancy | Postoperative discrepancy |
|---|---|---|
| Hip length | 4.0 ± 5.1 | 0.6 ± 3.6 |
| Leg length | 2.9 ± 3.0 | 0.3 ± 2.1 |
mm = millimeters.
When the cup COR is changed from the anatomic by 6 mm or more, the mean and range of offset is increased statistically (Table 3). A superior COR requires greater offset for clearance of the femur from the pelvis by the manual measurements we performed. When superior and medial changes were combined, the influence of COR was greater. The acceptable COR was defined as 3 mm or less superiorly and 5 mm or less medially (23 hips) and these hips had a discrepancy in hip offset from the normal hip of 0.4 ± 3.8 mm (Fig. 5); a change of COR of 6 mm or more superiorly and 6 mm or more medially (7 hips) had a discrepancy of 3.9 ± 6.3 mm (Fig. 6) The two dysplastic hips in this study required superior displacement of the COR more than 6 mm to permit coverage of the cup. Four of 17 valgus hips (femoral neck shaft angle greater than 135o) had an increased postoperative hip offset discrepancy of 6 mm or more which was clinically necessary to prevent manual impingement during intraoperative examination (Fig. 7). These hips were the four outliers in offset from the desired maximum discrepancy of 6 mm. Seven hips had a preoperative offset discrepancy between the arthritic and normal hip of more than 6 mm (range, −14.8 to 11.7 mm), which was considered anatomically asymmetric offset, (Fig. 2).
Table 3.
Cup center of rotation (COR) and offset
| COR superior (mm) | n hips | Offset discrepancy |
|---|---|---|
| 0–3 | 46 | 1.1 ± 3.6 |
| 4–5 | 23 | 1.7 ± 6.3 |
| 6+ | 14 | 2.9 ± 6.3* |
COR superior = number of millimeters the COR is displaced superiorly; n hips = number of hips; offset discrepancy = the discrepancy in offset between the normal hip and the reconstructed hip; * = p = 0.02 versus contralateral normal hip.
Fig. 5.
Postoperative radiographic with hip COR within 3 mm superior and 5 mm medial so hip offset and length are within 3 mm of the normal hip.
Fig. 6.
Postoperative AP pelvis radiograph of dysplastic hip with acetabular cup placement using the medial protrusio technique which elevated and medialized the COR more than 6 mm so the reconstruction required a high offset stem. This was the only hip which did not keep hip length discrepancy within 6 mm.
Fig. 7.
Postoperative radiograph with offset increased more than 6 mm to prevent bony impingement because of a valgus hip. The iliopsoas tendon should be recessed to avoid tendinitis.
Discussion
Precise reconstruction of hip biomechanics is one goal of THA surgery. Several studies have documented the importance of the hip COR to both longevity of the hip replacement [10, 18, 19, 26–28] and muscle function [1, 9, 17]. In studies on function, the relationship of COR to the hip offset was documented. In clinical series, superomedial or superolateral displacement of the hip COR contributed to loosening of the socket and femur. Superior displacement of COR by 5 mm or more distorts the femoral offset so a high offset stem is required to restore femoral bone position [4]. The use of a high offset stem is consistent with our finding of the necessity of increased offset with superior COR. With our use of computer navigation the data correlated the quantitative change in COR to the quantitative change in hip offset necessary to avoid impingement by intraoperative manual testing. We also investigated whether the quantitative knowledge provided by computer navigation allowed us to obtain offset of the THA within 6 mm of a contralateral normal hip as measured radiographically. This is important because one study correlates offset more than this with increased wear [13]. We were able to keep offset within 6 mm in 78 of 82 hips (95%), and only in hips with a neck shaft angle greater than 135° were we not able to maintain offset within 6 mm (Fig. 7). Finally, we asked whether we could keep radiographic hip length within 6 mm, which has been the standard for avoidance of clinical leg length difference [16, 20]. We were able to do so in 81 of 82 patients (99%), and in these patients the clinical leg lengths were within ± 2.5 mm. In our experience, patients do not tolerate clinical leg length difference more than 3 mm so this number is clinically more important than the radiographic discrepancy of 6 mm. With this biomechanical reconstruction, there was no patient with functional leg length difference [21], dislocation, or impingement pain [16].
The most important limitation was the inability to control rotation of the hip for accurate hip offset measurement on radiographs. This potential error was minimized by using the contralateral hip as the control. The second limitation was that validation of the computer navigation software was not performed with CT scans. However, the accuracy of imageless computer navigation for offset and hip length was validated by Renkawitz et al. [22] in a study of 17 cadavers using CT scans. The true offset was known by measurement of the cadaver and there was close agreement of CT scan and imageless computer navigation. Therefore, imageless computer navigation can be considered accurate in measurement of offset.
We contend reconstruction of offset by THA can only be accurately measured by including the acetabular reconstruction, which usually changes the center of rotation of the hip. This was validated by our correlation of change in the cup COR to offset reconstruction. It clinically confirms the computer model of Kurtz et al. that showed change in acetabular COR had a greater effect on bony impingement than femoral offset [12]. Their computer modeling study showed the greater the variance of the cup center of rotation (more superior, more medial, or both) the more the hip offset (combination of femoral offset and cup offset in their study) had to be increased to avoid impingement. This is the same finding as in our clinical study and consistent with the necessity for high offset stems in one study where 42 of 109 (39%) hips had a hip center superior by a mean 5 ± 6 mm and medially displaced by a mean 3.7 ± 6 mm [4]. The influence of center of rotation was also studied in both surface and conventional THAs [25]. In this study the cup was medialized a mean 6 mm with both types of arthroplasty. With the surface replacement, the difference could not be compensated by increasing femoral offset so medialization caused a reduced hip offset compared to the normal side in 20 of 22 hips. The conventional THAs had an increased offset of mean 5.2 mm in 17 of 19 hips because the femoral component could be adjusted.
Superior displacement of the hip COR decreases the perpendicular distance to the vector of the gluteus medius with consequent reduction of abductor strength [1, 19]. Therefore, the offset must be increased to adjust this perpendicular distance for function. However, increasing the offset more than 5 mm from the normal hip increases polyethylene wear [13]. Therefore, if the hip center is moved by 5 mm or more superiorly, the hip offset must be increased, yet this may reduce the longevity of the hip if offset is increased by more than 5 mm. Our data show that only by limiting superior displacement of the hip COR to 3 mm, and medialization to 5 mm or less, can an increase in offset always be kept within 5 mm (0.4 ± 3.8 mm). These data are compelling evidence that to maximize muscle function and minimize wear the superior COR must be kept within 3 mm of normal. This quantitative correlation confirms the clinical data that correlated failure of THA to radiographic COR displacement of 2 mm or more superiorly [10, 18, 19, 26, 27].
Computer navigation provided intraoperative knowledge of quantitative change of hip offset. Radiographic measurement of hip offset showed more change than measured intraoperatively with navigation because of rotation and magnification of radiographs (Table 1). Using computer navigation, the greater trochanter method of measurement was more likely precise for both hip offset and hip length because it measures change closer to the center of the hip [20]. Distal femoral pin sites cause discomfort for some patients as long as 6 weeks postoperatively, although we experienced no fractures and no sequelae at 1 year. As a consequence of this study, and the published relationship of center of rotation to wear and longevity, we strive to keep the center at no more than 3 mm superior and 5 mm medially. However, the COR of the cup cannot be restored to the COR of the anatomic acetabulum with some hip deformities, such as severe dysplasia or severe migration of the femoral head. Technically, the center of rotation of the cup is determined by the depth of reaming. Without guidance from computer navigation, the best anatomic landmarks are to not ream medially beyond the cortical bone of the cotyloid notch and inferomedially maintain the edge of the cup at the level of the transverse acetabular ligament. At the superoanterior rim of the bony acetabulum the metal shell should be flush with bone. There may be up to 3 mm of metal uncovered by the superior posterior rim of acetabulum because the anatomic acetabulum has average inclination of 55° and cup inclination must not exceed 45° [5].
Our data educate the orthopaedic surgeon to the importance of the strong correlation of hip offset to COR of the cup; thinking about hip offset rather than femoral offset; and the benefit of computer navigation in maintaining hip offset and length within 6 mm of normal, as measured radiographically. It is important to remember that asymmetric hip offset does occur and restoration to normal may not equal the opposite hip. Additionally, dysplastic hips often require superior displacement of the COR to allow coverage of the cup, which we experienced in both the dysplastic hips in this study. If it is necessary to increase the offset, as we observed in valgus hips, we release that portion of attachment of the iliopsoas muscle to the proximal side of the lesser trochanter, which recesses this muscle and prevents tendinitis [8].
Acknowledgments
We thank Patricia J. Paul for preparation of this manuscript.
Footnotes
One or more of the authors (LDD) received royalties from Zimmer, Inc.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20:414–420. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Bourne RB, Rorabeck CH. Soft tissue balancing: The hip. J Arthroplasty. 2002;17(Suppl 1):17–22. doi: 10.1054/arth.2002.33263. [DOI] [PubMed] [Google Scholar]
- 3.Charles MN, Bourne RB, Davey JR, Greenwald AS, Morrey BF, Rorabeck CH. Soft-tissue balancing of the hip: the role of femoral offset restoration. J Bone Joint Surg Am. 2004;86:1078–1088. [PubMed] [Google Scholar]
- 4.Dolhain P, Tsigaras H, Bourne RB, Rorabeck CH, Mac Donald S, Mc Calden R. The effectiveness of dual offset stems in restoring offset during total hip replacement. Acta Orthop Belg. 2002;68:490–499. [PubMed] [Google Scholar]
- 5.Dorr LD. Hip Arthroplasty: Minimally Invasive Techniques and Computer Navigation. 1. Philadelphia, PA: WB Saunders; 2005. [Google Scholar]
- 6.Flecher X, Parratte S, Brassart N, Aubaniac JM, Argenson JN. Evaluation of the hip center in total hip arthroplasty for old development dysplasia. J Arthroplasty. 2008;23:1189–1196. doi: 10.1016/j.arth.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 8.Heaton K, Dorr LD. Surgical release of iliopsoas tendon for groin pain after total hip arthroplasty. J Arthroplasty. 2002;17:779–781. doi: 10.1054/arth.2002.33570. [DOI] [PubMed] [Google Scholar]
- 9.Johnston RC, Brand RA, Crownenshield RD. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979;61:639–652. [PubMed] [Google Scholar]
- 10.Karachalios T, Hartofilakidis G, Zacharakis N, Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res. 1993;296:140–147. [PubMed] [Google Scholar]
- 11.Krishnan SP, Carrington RW, Mohiyaddin S, Garlick N. Common misconceptions of normal hip joint relations on pelvic radiographs. J Arthroplasty. 2006;21:409–412. doi: 10.1016/j.arth.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 12.Kurtz WB, Ecker TM, Reichmann WM, Murphy SB. Factors affecting bony impingement in hip arthroplasty. J Arthroplasty. 2010;25:624–634. doi: 10.1016/j.arth.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467:2895–2900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long WT, Dastane M, Harris MJ, Wan Z, Dorr LD. Failure of the Durom Metasul acetabular component. Clin Orthop Relat Res. 2010;468:400–405. doi: 10.1007/s11999-009-1071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loughead JM, Chesney D, Holland JP, McCaskie AW. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg Br. 2005;87:163–166. doi: 10.1302/0301-620X.87B2.15151. [DOI] [PubMed] [Google Scholar]
- 16.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 17.McGrory BJ, Morrey BJ, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:865–869. [PubMed] [Google Scholar]
- 18.Pagnano MW, Hanssen AD, Lewallen DG, Shaughnessy WJ. Effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am. 1996;78:1004–1014. doi: 10.2106/00004623-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ranawat CS, Dorr LD, Inglis AE. Total hip arthroplasty in protusio acetabuli of rheumatoid arthritis. J Bone Joint Surg Am. 1980;62:1059–1065. [PubMed] [Google Scholar]
- 20.Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16:715–720. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 21.Ranawat CS, Rodriguez JA. Functional leg-length inequality following total hip arthroplasty. J Arthroplasty. 1997;12:359–364. doi: 10.1016/S0883-5403(97)90190-X. [DOI] [PubMed] [Google Scholar]
- 22.Renkawitz T, Schuster T, Herold T, Goessmann H, Sendtner E, Grifka J, Kalteis T. Measuring leg length and offset with an imageless navigation system during total hip arthroplasty: is it really accurate? Int J Med Robot. 2009;5:192–197. doi: 10.1002/rcs.250. [DOI] [PubMed] [Google Scholar]
- 23.Resnick D. Bone and Joint Imaging. 3. Philadelphia, PA: Elsevier Saunders; 2005. [Google Scholar]
- 24.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–134. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Silva, M, Lee KH, Heisel C, Dela Rosa MS, Schmalzried TP. The biomechanical results of total hip resurfacing arthroplasty. J Bone Joint Surg Am. 2004;86-A:40–60. [DOI] [PubMed]
- 26.Stans AA, Pagnano MW, Shaughnessy WJ, Hanssen AD. Results of total hip arthroplasty for Crowe type III developmental hip dysplasia. Clin Orthop Relat Res. 1998;348:149–157. doi: 10.1097/00003086-199803000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Sugano N, Noble PC, Kamaric E. Predicting the position of the femoral head center. J Arthroplasty. 1999;14:102–107. doi: 10.1016/S0883-5403(99)90210-3. [DOI] [PubMed] [Google Scholar]
- 28.Yoder SA, Brand RA, Pedersen DR, O’Gorman TW. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;228:79–87. [PubMed] [Google Scholar]