Abstract
BACKGROUND:
The N-terminal fragment of pro-brain type natriuretic peptide (NT-proBNP) is an established biomarker for cardiac failure.
OBJECTIVE:
To determine the influence of preoperative serum NT-proBNP on postoperative outcome and mid-term survival in patients undergoing coronary artery bypass grafting (CABG).
METHODS:
In 819 patients undergoing isolated CABG surgery preoperative serum NT-proBNP levels were measured. NT-proBNP was correlated with various postoperative outcome parameters and survival rate after a median follow-up time of 18 (0.5–44) months. Risk factors of mortality were identified using χ2, Mann–Whitney test, and Cox regression.
RESULTS:
NT-proBNP levels >430 ng/ml and >502 ng/ml predicted hospital and overall mortality (p<0.05), with an incidence of 1.6% and 4%, respectively. Kaplan–Meier analysis revealed decreased survival rates in patients with NT-proBNP >502 ng/ml (p = 0.001). Age, preoperative serum creatinine, diabetes, chronic obstructive pulmonary disease, low left ventricular ejection fraction and BNP levels >502 ng/ml were isolated as risk factors for overall mortality. Multivariate Cox regression analysis, including the known factors influencing NT-proBNP levels, identified NT-proBNP as an independent risk factor for mortality (OR = 3.079 (CI = 1.149-8.247), p = 0.025). Preoperative NT-proBNP levels >502 ng/ml were associated with increased ventilation time (p = 0.005), longer intensive care unit stay (p = 0.001), higher incidence of postoperative hemofiltration (p = 0.001), use of intra-aortic balloon pump (p<0.001), and postoperative atrial fibrillation (p = 0.031)
CONCLUSION:
Preoperative NT-proBNP levels >502 ng/ml predict mid-term mortality after isolated CABG and are associated with significantly higher hospital mortality and perioperative complications.
Keywords: Brain type natriuretic peptide, BNP, NT-proBNP, CABG, Coronary artery disease
INTRODUCTION
Brain type natriuretic peptide (BNP) is primarily produced by cardiac myocytes. Physiological effects of BNP are a peripheral vasodilatation and inhibition of renin–angiotensin production.1-3 The precursor peptide proBNP is split into the active hormone BNP and the N-terminal fragment of proBNP (NT-proBNP). Both BNP and NT-proBNP are established markers for cardiac failure. However, other pathologies such as exacerbated chronic obstructive pulmonary disease, acute coronary syndromes, atrial fibrillation, and myocarditis can cause elevated BNP levels. Additionally, higher NT-proBNP levels are associated with: female gender, impaired renal function, and older age. Obesity has been shown to decrease NT-proBNP levels.2 Increased BNP levels are a prognostic marker associated with higher mortality in patients with myocardial infarction, cardiogenic shock, and pulmonary embolism.4-6 In patients with coronary artery disease increased BNP levels are associated with an increased rate of myocardial infarction and cardiovascular death during mid-term follow-up.7
We aimed to investigate if preoperative serum NT-proBNP levels are associated with hospital and mid-term mortality and with postoperative outcome variables in patients undergoing isolated coronary artery bypass grafting (CABG)
PATIENTS AND METHODS
Data used in the analysis were collected from the institutional database at the Department of Cardiac Surgery, Innsbruck Medical University, which contained data collected using the data collection form of the Society of Thoracic Surgeons (Adult Cardiac Surgery Database Data Collection form Version 2.25.1). Preoperative NT-proBNP was measured routinely in all patients on the day of admission before surgery. The data of 819 patients undergoing isolated CABG were analysed. Patients included in the study were consecutive cases with CABG seen at our department between 2001 and 2007. Patients with concomitant procedures (valve surgery, aortic surgery, etc) were excluded. Patients with missing preoperative NT-proBNP values were also excluded. Patients were followed up by request of the national death registry (Statistik Austria).
Definitions
Primary end points of the study included:
Hospital mortality, defined as the incidence of death occurring during admission to hospital for surgery or up to 30 days after CABG
Overall mortality, defined as hospital deaths and all deaths during the follow-up time.
Secondary end points of the study were:
Carotid artery disease, defined as the presence of carotid artery stenosis of ≥50%, or carotid artery occlusion, or post-carotid endarterectomy.
The EuroSCORE, used for perioperative risk stratification as described by Nashef and coworkers.8
Hypertension, diagnosed if current blood pressure was >140 mmHg systolic or >90 mmHg diastolic, or if the patient was currently receiving antihypertensive drugs, or if the patient had a history of hypertension.
Stroke, defined as any neurologic impairment of motor, sensory or cognitive function that persisted for >24 h, or was associated with death, and that could not be explained by other neurologic etiologies (ie, postoperative delirium, dementia, head trauma).
History of neurologic events, defined as a preoperative history of transient ischemic attack or stroke.
Chronic obstructive pulmonary disease (COPD), defined by long-term use of bronchodilators or steroids for lung disease and forced expiratory volume in one second (FEV1) <80% of the predicted value in preoperative spirometry, which was performed routinely at our clinic.
Peripheral vascular disease, defined as the presence of intermittent claudication, or previous or planned intervention on the abdominal aorta or limb arteries.
Ventilation time, defined as the duration of ventilation needed postoperatively, including potential need for additional ventilation after re-intubation.
Intensive care unit (ICU) stay, defined as the duration of ICU stay needed after the operation, including potential need for additional ICU stay after readmission.
Perioperative myocardial infarction, defined as the development of new persistent ST-segment, T- or Q-wave changes in electrocardiogram (ECG), new left bundle branch block, and/or troponin T elevation above the 5×99th centile of the upper reference limit and/or creatine kinase (CK)-MB/CK ratio of >10%.
Need for intra-aortic balloon pump (IABP), defined as any use of an IABP after establishing cardiopulmonary bypass or in the postoperative period.
Postoperative atrial fibrillation, defined as any new episode of atrial fibrillation documented by online monitoring or on ECG during the postoperative period.
Reoperation for bleeding, defined as any incidence of reoperation needed for bleeding complications.
Statistical Analysis
Continuous variables are shown as median and range, categorical variables as number and percentage. The 1-, 2-, and 3-year survival rates were calculated using a life table. We calculated the best cut-off values of NT-proBNP to predict hospital mortality or overall mortality by using receiver operating characteristic (ROC) curves. The comparison between categorical variables and hospital mortality, overall death, or NT-proBNP >502 ng/l was performed using χ2 analysis. The comparison between continuous variables and hospital mortality, overall death, or NT-proBNP >502 ng/l was performed using a Mann–Whitney test. Survival curves were generated using Kaplan–Meier estimates. Differences in the survival rate were calculated using the log rank test. For multivariate analysis we used a Cox regression model. As covariates the factors commonly known to influence NT-proBNP levels were entered: gender, age (we chose an age >67 years, which was the median of our cohort), body mass index (calculated as body weight [kg]/height2 [m2]; we chose a BMI >27 kg/m2, which was the median of our cohort), serum creatinine levels above the upper reference limit of 1.2 mg/dl. A p value <0.05 was regarded as statistically significant. SPSS™ 15.0 for Windows (SPSS Inc, Chicago, USA) statistical software was used.
RESULTS
After a median follow up time of 18 (0.5–44) months 33/819 (4%) patients died, including 13/819 (1.6%) hospital deaths. The 1, 2-, and 3-year survival rates (including hospital mortality) were 97%, 93%, and 90%, respectively.
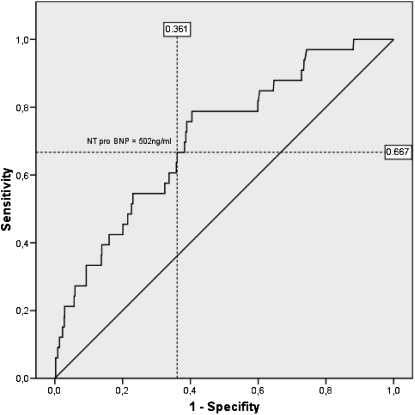
Analysis of the ROC curves showed that a serum NT-proBNP cut-off level of 430 ng/l best predicted hospital mortality and a cut-off level of 502 ng/l best predicted overall mortality (Figure 1). Univariate analysis showed that age, preoperative serum creatinine, peripheral vascular disease, and NT-proBNP levels >430 ng/l were significantly associated with hospital mortality. Age, preoperative serum creatinine, diabetes mellitus, history of cerebrovascular accident, chronic obstructive pulmonary disease, left ventricular ejection fraction, and NT-proBNP levels >502 ng/l were significantly associated with overall mortality (Tables 1 and 2).
Figure 1.
Receiver operating characteristic curve of N-terminal pro-brain type natriuretic peptide (NT-proBNP) level predicting overall death.
Table 1.
Univariate correlations between demographical data of 819 coronary artery bypass patients and hospital mortality and mid-term mortality.
| Hospital mortality (p values) | Hospital mortality (RR) | Overall death (p values) | Overall death (RR) | |
| Male gender | 0.176 | 2.11 (0.7–6.39) | 0.059 | 1.93 (0.97–3.85) |
| Chronic renal failure requiring dialysis | 0.736 | 0.166 | 0.28 (0.04–1.75) | |
| History of smoking | 0.924 | 1.06 (0.33–3.4) | 0.582 | 0.82 (0.41–1.65) |
| Current smoker | 0.480 | 0.912 | ||
| Diabetes mellitus | 0.910 | 1.08 (0.3–3.76) | 0.014 | 0.44 (0.22–0.86) |
| Insulin-dependent diabetes mellitus | 0.349 | 0.030 | 0.37 (0.15–0.92) | |
| Family history of coronary artery disease | 0.152 | 0.44 (0.14–1.4) | 0.203 | 0.606 (0.28–1.31) |
| Arterial hypertension | 0.960 | 1.039 (0.23–4.63) | 0.966 | 1.020 (0.40–2.59) |
| Dyslipidemia | 0.444 | 0.463 (0.06–3.53) | 0.332 | 1.495 (0.66–3.37) |
| History of cerebrovascular accident | 0.471 | na | <0.001 | 0.220 (0.09–0.53) |
| Chronic obstructive pulmonary disease | 0.073 | 0.377 (0.124–1.141) | 0.04 | 0.50 (0.26–0.98) |
| Peripheral vascular disease | 0.046 | 0.324 (0.10–1.03) | 0.127 | 0.534 (0.24–1.2) |
| Carotid artery disease | 0.339 | na | 0.412 | 2.21 (0.31–15.89) |
| History of myocardial infarction | 0.204 | 0.5 (0.16–1.5) | 0.053 | 0.52 (0.26–1.02) |
| Previous percutaneous coronary intervention | 0.515 | 0.61 (0.14–2.17) | 0.680 | 0.80 (0.29–2.24) |
| Urgent operation | 0.430 | 0.6 (0.17–2.15) | 0.634 | 0.81 (0.34–1.42) |
| Reoperation for bleeding | <0.001 | 0.05 (0.02–0.17) | <0.001 | 0.14 (0.05–0.38) |
| Perioperative myocardial infarction | <0.001 | 0.04 (0.01–0.23) | <0.001 | 0.06 (0.02–0.28) |
| Perioperative stroke | <0.001 | 0.44 (0.01–0.46) | 0.033 | 0.12 (0.01–1.21) |
| Postoperative transient ischemic attack | 0.857 | 1.01 (1.00–1.03) | 0.772 | 1.04 (1.03–1.06) |
| Postoperative renal failure | <0.001 | 0.022 (0.01–0.07) | <0.001 | 0.04 (0.02–0.1) |
| Postoperative atrial fibrillation | 0.525 | 1.63 (0.36–7.40) | 0.831 | 0.92 (0.41–2.06) |
| Sternal wound infections | 0.620 | 1.02 (1.01–1.03) | 0.423 | 1.04 (1.03–1.06) |
| Intraoperative blood products | 0.029 | 0.30 (0.1–0.94) | 0.251 | 0.66 (0.33–1.35) |
| NT-proBNP serum level >430 ng/l | 0.036 | 0.31 (0.1–0.99) | <0.001 | 0.22 (0.10–0.49) |
| NT-proBNP serum level >502 ng/l | 0.216 | 0.51 (0.17–1.51) | <0.001 | 0.3 (0.15–0.60) |
NT-proBNP; N-terminal pro-brain type natriuretic peptide; RR, relative risk.
Table 2.
Statistical differences between patients who are alive or dead at discharge and at time of follow-up.
| Discharge alive | Discharge dead | p Value | Alive at follow-up | Dead at follow-up | p Value | |
| Age (years) | 67 (27–89) | 76 (55–80) | 0.022 | 67 (27–89) | 76 (55–80) | 0.011 |
| Body mass index (kg/m2) | 27 (18–55) | 26 (20–36) | 0.573 | 27 (18–55) | 26 (19–40) | 0.886 |
| Preoperative serum creatinine (mg/dl) | 1.0 (0.5–6.2) | 1.2 (0.7–2.0) | 0.024 | 1 (0.5–6.2) | 1.1 (0.7–5.0) | 0.018 |
| Left ventricular ejection fraction (%) | 51 (10–91) | 54 (25–70) | 0.716 | 53 (10–91) | 50 (20–70) | 0.008 |
| Logarithmic EuroSCORE | 3 (0–63) | 5 (2–63) | 0.092 | 3 (0–52) | 5 (1–63) | 0.003 |
| Linear EuroSCORE | 4 (0–17) | 5 (1–11) | 0.092 | 4 (0–15) | 6 (0–17) | 0.008 |
| Total number of distal coronary anastomoses | 3 (1–6) | 3 (1–5) | 0.773 | 3 (1–6) | 3 (1–5) | 0.580 |
| Cardiopulmonary bypass time (min) | 103 (0–428) | 113 (0–355) | 0.597 | 103 (0–428) | 104 (0–355) | 0.749 |
| Aortic cross-clamping time (min) | 57 (0–345) | 64 (0–127) | 0.986 | 57 (0–345) | 58 (0–127) | 0.809 |
| Total mechanical ventilation time (h) | 8 (0–1,900) | 19 (7–482) | <0.001 | 8 (0–776) | 18 (4–1,900) | <0.001 |
| Total time on ICU (h) | 21 (1–1,919) | 58 (7–1,012) | <0.001 | 21 (1–1,268) | 45 (7–1,919) | <0.001 |
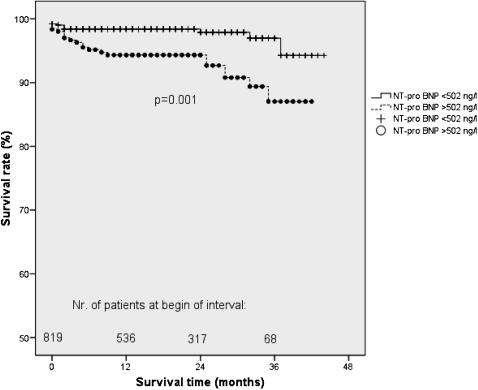
The Kaplan–Meier analysis confirmed a significantly decreased survival rate of patients with NT-proBNP levels >502 ng/l (n = 306) compared with NT-proBNP levels ≤502 ng/l (n = 513) (p = 0.001, Figure 2) The 1, 2-, and 3-year survival rates (including hospital mortality) were 98%, 96%, and 92%, respectively, if NT-proBNP levels were ≤502 ng/l vs. 94%, 87%, and 87%, respectively, if NT-proBNP levels were >502 ng/l.
Figure 2.
Survival rate of coronary artery bypass patients with preoperative serum N-terminal pro-brain type natriuretic peptide (NT-proBNP) levels > 502 ng/l compared with NT-proBNP levels < 502 ng/l.
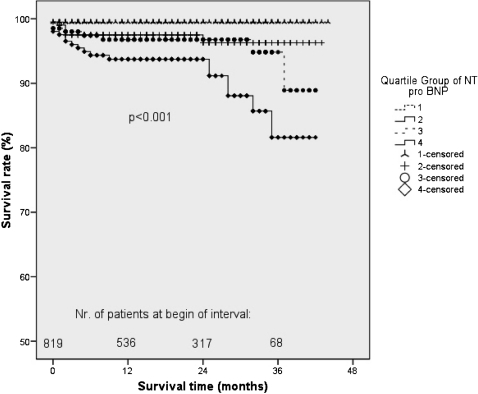
Mortality According to Quartiles of Serum NT-proBNP levels
Incidence of death during follow-up was significantly higher in the highest (18/205) in comparison with the lowest NT-proBNP quartile (1/203), (p<0.001, Table 3). Cox regression analysis of the different quartiles of NT-proBNP also showed significant differences. (p<0.001, Figure 3)
Table 3.
Overall death rate (n = 33) of 819 coronary artery bypass patients grouped according to quartiles of serum N-terminal pro-brain type natriuretic peptide (NT-proBNP) levels.
| Quartile | NT-pro-BNP (ng/l) | n | deaths |
| 1 | 66 (6–122) | 203 | 1 |
| 2 | 194 (123–291) | 207 | 6 |
| 3 | 502 (296–808) | 204 | 8 |
| 4 | 1704 (810–65,998) | 205 | 18 |
The difference between the groups was statistically significant (p<0.001).
Figure 3.
Mid- term survival of coronary artery bypass patients stratified by quartiles of preoperative N-terminal pro-brain type natriuretic peptide (NT-proBNP) levels.
Multivariate Cox regression analysis (covariates: gender, age >67 years, BMI >27 kg/m2, serum creatinine >1.2 mg/dl) revealed NT-proBNP as an independent risk factor for mid-term survival (p = 0.025, OR = 3.079, CI = 1.149–8.247).
Association Between NT-proBNP Levels and Perioperative Outcome
Patients with NT-proBNP levels >502 ng/l had more comorbidities and consecutively a higher EuroSCORE than those with NT-proBNP levels ≤502 ng/l. Postoperatively those patients had a significantly longer ventilation time (p = 0.005), longer ICU stay (p = 0.001), a higher rate of renal failure requiring hemofiltration (p = 0.001), a higher rate of IABPs (p<0.001), and a higher rate of postoperative atrial fibrillation (p = 0.031) than patients with NT-proBNP levels ≤502 ng/l (Table 4).
Table 4.
Demography of 819 isolated coronary artery bypass patients with preoperative evaluation of serum N-terminal pro-brain type natriuretic peptide (NT-proBNP) levels.
| All patients | NT-proBNP>502 (n = 306) | NT-proBNP≤502 (n = 513) | p Value | |
| Age (years) | 67 (27–89) | 71 (42–89) | 65 (27–84) | <0.001 |
| Male gender | 632 (77%) | 70% | 82% | <0.001 |
| Body mass index (kg/m2) | 27 (18–55) | 26 (18–55) | 27 (18–47) | 0.034 |
| Preoperative serum creatinine (mg/dl) | 1.0 (0.5–6.2) | 1.0 (0.5–6.2) | 1.0 (0.5–3.0) | <0.001 |
| Chronic renal failure requiring dialysis | 7 (1%) | 2% | 0% | <0.001 |
| History of smoking | 262 (32%) | 33% | 31% | 0.524 |
| Current smoker | 79 (10%) | 11% | 9% | 0.273 |
| Diabetes mellitus | 200 (24%) | 32% | 20% | <0.001 |
| Insulin-dependent diabetes mellitus | 51 (6%) | 11% | 3% | <0.001 |
| Family history of coronary artery disease | 133 (16%) | 16% | 16% | 0.952 |
| Arterial hypertension | 697 (85%) | 88% | 84% | 0.124 |
| Dyslipidemia | 680 (83%) | 82% | 86% | 0.143 |
| History of cerebrovascular accident | 31 (4%) | 5% | 3% | 0.196 |
| Chronic obstructive pulmonary disease | 308 (38%) | 45% | 32% | <0.001 |
| Peripheral vascular disease | 103 (13%) | 19% | 9% | <0.001 |
| Carotid artery disease | 53 (7%) | 8% | 6% | 0.218 |
| History of myocardial infarction | 362 (44%) | 61% | 34% | <0.001 |
| Previous percutaneous coronary intervention | 82 (10%) | 9% | 11% | 0.264 |
| Left ventricular ejection fraction (%) | 51 (10–84) | 49 (10–83) | 58 (21–91) | <0.001 |
| Urgent operation | 139 (17%) | 20% | 13% | 0.004 |
| Logarithmic EuroSCORE | 2.51 (1–63) | 4 (1–63) | 2 (1–29) | <0.001 |
| Linear EuroSCORE | 4 (0–17) | 5 (0–17) | 3 (0–12) | <0.001 |
| Total number of distal coronary anastomoses | 3 (1–6) | 3 (1–6) | 3 (1–6) | 0.094 |
| Cardiopulmonary bypass time (min) | 103 (0–428) | 103 (0–355) | 103 (0–428) | 0.803 |
| Aortic cross-clamping time (min) | 57 (0–345) | 57 (0–153) | 58 (0–230) | 0.492 |
| Intraoperative use of blood products | 272 (33%) | 41% | 29% | 0.001 |
| Total mechanical ventilation time (h) | 8 (0–1900) | 8 (0–1900) | 8 (0–767) | 0.005 |
| Total time on ICU (h) | 22 (7–1,919) | 22 (12–1919) | 21 (7–1,268) | 0.001 |
| Reoperation owing to bleeding | 30 (4%) | 4% | 4% | 0.761 |
| Perioperative myocardial infarction | 8 (1%) | 1% | 1% | 0.458 |
| Perioperative stroke | 4 (0.5%) | 1% | 0.2% | 0.119 |
| Postoperative transient ischemic attack | 2 (0.24%) | 0.3% | 0.2% | 0.711 |
| Postoperative renal failure requiring hemofiltration | 28 (3%) | 6% | 2% | 0.001 |
| Intra-aortic balloon pump | 33 (4%) | 6% | 1% | <0.001 |
| Postoperative atrial fibrillation | 186 (23%) | 27% | 20% | 0.031 |
| Sternal wound infections | 15 (2%) | 2% | 2% | 0.745 |
DISCUSSION
NT-proBNP and Hospital Mortality
In our series ROC curve analysis revealed an NT-proBNP cut-off level of 430 ng/l to best predict hospital mortality and a cut-off level of 502 ng/l for prediction of overall mortality. These levels are comparable to cut-off levels for predicting postoperative cardiac events in patients undergoing vascular surgery, which were reported to be between 280 and 533 pg/ml.1 Nozohoor et al. found that an increased BNP level on admission to the ICU was a risk factor for heart failure following aortic valve replacement.9 Nevertheless, one has to keep in mind that cut-off points vary between different study cohorts. Thus we focused on patients undergoing isolated CABG surgery in our study.
We found that age, preoperative serum creatinine, peripheral vascular disease, and NT-proBNP levels >430 ng/l were significantly associated with hospital mortality. Although the first three risk factors are also found to be predictive for hospital mortality in the EuroSCORE, NT-proBNP is not part of this preoperative risk score for cardiac surgery patients.8 In an interesting study, Grabowski et al. found a higher early mortality and a decreased PCI success rate (especially an increased number of no-reflow phenomenon) in patients with acute ST elevation myocardial infarction and with high levels of serum BNP.4
NT-proBNP and Mid-term Survival Rates
In a series of 98 male patients undergoing different types of heart surgery Hutfless et al. found increased BNP levels in patients who died within 1 year after surgery.10 Kragelund et al. found a decreased long-term survival in 1039 patients with stable coronary artery disease and increased BNP levels.11 Other authors found that BNP and NT-proBNP levels were predictive for survival rates in patients with acute coronary syndromes and acute myocardial infarction.12,13 In our study, mid-term survival rates were significantly decreased in patients with elevated NT-proBNP levels. Furthermore, NT-proBNP remained as a significant risk factor of survival when the commonly known factors influencing BNP levels (ie, gender, age BMI, serum creatinine) were included in the multivariate analysis.
NT-proBNP and Postoperative Complications
We found an increased mechanical ventilation time and length of ICU stay in patients with elevated preoperative NT-proBNP levels. In general, those patients exhibited a higher rate of comorbidities, resulting in an increased risk score (EuroSCORE). In detail, a higher rate of postoperative renal failure requiring hemofiltration was found, which may be explained by the higher preoperative serum creatinine levels in patients with NT-proBNP levels >502 ng/ml. We also found a higher rate of IABPs associated with higher NT-proBNP levels. This is in good agreement with Hutfless et al., who reported higher BNP levels in patients requiring an IABP postoperatively compared with those who did not.10 In exacerbated COPD elevated BNP levels were associated with a prolonged stay in the ICU.14
Atrial fibrillation is a common complication after cardiac surgery. Although it is easily manageable, it causes a (transient) circulatory disturbance that may be critical for the intensive care patient. In our study we found a higher rate of postoperative atrial fibrillation in patients with elevated NT-proBNP levels. Wazni and coworkers found that patients with atrial fibrillation following cardiac surgery exhibited higher BNP levels than patients who remained in sinus rhythm throughout the postoperative course.15
Clinical impact of the study
Preoperative measurement of NT-proBNP levels can be used, in addition to established risk scores, to determine CABG patients with an increased risk. Since the mid-term survival following coronary bypass surgery is significantly decreased, patients with increased NT-proBNP should be followed up closely. In accordance with this, Mayer et al. recently published results showing a decreased long-term survival rate of coronary patients without clinical manifestation of heart failure and NT-proBNP levels >862 pmol/l.16
We conclude that elevated preoperative serum NT-proBNP levels are associated with a higher postoperative early and mid-term mortality, as well as morbidity, in patients undergoing isolated CABG.
REFERENCES
- 1.Rodseth RN. B type natriuretic peptide – a diagnostic breakthrough in peri-operative cardiac risk assessment? Anaesthesia. 2009;64:165–78. doi: 10.1111/j.1365-2044.2008.05689.x. 10.1111/j.1365-2044.2008.05689.x [DOI] [PubMed] [Google Scholar]
- 2.Steiner J, Guglin M. BNP or NT-proBNP? A clinician's perspective. Int J Cardiol. 2008;129:5–14. doi: 10.1016/j.ijcard.2007.12.093. 10.1016/j.ijcard.2007.12.093 [DOI] [PubMed] [Google Scholar]
- 3.Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–68. doi: 10.1016/j.jacc.2007.09.021. 10.1016/j.jacc.2007.09.021 [DOI] [PubMed] [Google Scholar]
- 4.Grabowski M, Filipiak KJ, Karpinski G, Wretowski D, Rdzanek A, Huczek Z, et al. Serum B-type natriuretic peptide levels on admission predict not only short-term death but also angiographic success of procedure in patients with acute ST-elevation myocardial infarction treated with primary angioplasty. Am Heart J. 2004;148:655–62. doi: 10.1016/j.ahj.2004.04.023. 10.1016/j.ahj.2004.04.023 [DOI] [PubMed] [Google Scholar]
- 5.Jarai R, Fellner B, Haoula D, Jordanova N, Heinz G, Karth GD, et al. Early assessment of outcome in cardiogenic shock: relevance of plasma N-terminal pro-B-type natriuretic peptide and interleukin-6 levels. Crit Care Med. 2009;37:1837–44. doi: 10.1097/CCM.0b013e31819fe896. 10.1097/CCM.0b013e31819fe896 [DOI] [PubMed] [Google Scholar]
- 6.Coutance G, Le Page O, Lo T, Hamon M. Prognostic value of brain natriuretic peptide in acute pulmonary embolism. Crit Care. 2008;12:R109. doi: 10.1186/cc6996. 10.1186/cc6996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schnabel R, Lubos E, Rupprecht HJ, Espinola-Klein C, Bickel C, Lackner KJ, et al. B-type natriuretic peptide and the risk of cardiovascular events and death in patients with stable angina: results from the AtheroGene study. J Am Coll Cardiol. 2006;47:552–8. doi: 10.1016/j.jacc.2005.09.039. 10.1016/j.jacc.2005.09.039 [DOI] [PubMed] [Google Scholar]
- 8.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/s1010-7940(99)00134-7. 10.1016/S1010-7940(99)00134-7 [DOI] [PubMed] [Google Scholar]
- 9.Nozohoor S, Nilsson J, Lührs C, Roijer A, Algotsson L, Sjögren J. B-type natriuretic peptide as a predictor of postoperative heart failure after aortic valve replacement. J Cardiothorac Vasc Anesth. 2009;23:161–5. doi: 10.1053/j.jvca.2008.11.006. 10.1053/j.jvca.2008.11.006 [DOI] [PubMed] [Google Scholar]
- 10.Hutfless R, Kazanegra R, Madani M, Bhalla MA, Tulua-Tata A, Chen A, et al. Utility of B-type natriuretic peptide in predicting postoperative complications and outcomes in patients undergoing heart surgery. J Am Coll Cardiol. 2004;43:1873–9. doi: 10.1016/j.jacc.2003.12.048. 10.1016/j.jacc.2003.12.048 [DOI] [PubMed] [Google Scholar]
- 11.Kragelund C, Grønning B, Køber L, Hildebrandt P, Steffensen R. N-Terminal pro–B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005;352:666–75. doi: 10.1056/NEJMoa042330. 10.1056/NEJMoa042330 [DOI] [PubMed] [Google Scholar]
- 12.Suzuki S, Yoshimura M, Nakayama M, Mizuno Y, Harada E, Ito T, et al. Plasma level of B-type natriuretic peptide as a prognostic marker after acute myocardial infarction. A long-term follow-up analysis. Circulation. 2004;110:1387–91. doi: 10.1161/01.CIR.0000141295.60857.30. 10.1161/01.CIR.0000141295.60857.30 [DOI] [PubMed] [Google Scholar]
- 13.Omland T, Persson A, Ng L, O'Brien R, Karlsson T, Herlitz J, et al. N-Terminal pro-B–type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002;106:2913–8. doi: 10.1161/01.cir.0000041661.63285.ae. 10.1161/01.CIR.0000041661.63285.AE [DOI] [PubMed] [Google Scholar]
- 14.Stolz D, Breidthardt T, Christ-Crain M, Bingisser R, Miedinger D, Leuppi J, et al. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest. 2008;133:1088–94. doi: 10.1378/chest.07-1959. 10.1378/chest.07-1959 [DOI] [PubMed] [Google Scholar]
- 15.Wazni OM, Martin DO, Marrouche NF, Latif AA, Ziada K, Shaaraoui M, et al. Plasma B-type natriuretic peptide levels predict postoperative atrial fibrillation in patients undergoing cardiac surgery. Circulation. 2004;110:124–7. doi: 10.1161/01.CIR.0000134481.24511.BC. 10.1161/01.CIR.0000134481.24511.BC [DOI] [PubMed] [Google Scholar]
- 16.Mayer O, Simon J, Plášková M, Cífková R, Trefil L. N-terminal proB-type natriuretic peptide as prognostic marker for mortality in coronary patients without clinically manifest heart failure. Eur J Epidemiol. 2009;24:363–8. doi: 10.1007/s10654-009-9339-6. 10.1007/s10654-009-9339-6 [DOI] [PubMed] [Google Scholar]