Abstract
AIM: To evaluate the efficacy of simple and extended cholecystectomy for mucosa (T1a) or muscularis (T1b) gallbladder (GB) cancer.
METHODS: Original studies on simple and extended cholecystectomy for T1a or T1b GB cancer were searched from MEDLINE (PubMed), Cochrane Library, EMBase, and CancerLit using the search terms of GB, cancer/carcinoma/tumor/neoplasm.
RESULTS: Twenty-nine out of the 2312 potentially relevant publications met the eligibility criteria. Of the 1266 patients with GB cancer included in the publications, 706 (55.8%) and 560 (44.2%) had T1a and T1b GB cancer, respectively. Simple cholecystectomy for T1a and T1b GB cancer was performed in 590 (83.6%) and 375 (67.0%) patients, respectively (P < 0.01). In most series, the treatment of choice was simple cholecystectomy for T1a GB cancer patients with a 5-year survival rate of 100%. Lymph node metastasis was detected in 10.9% of the T1b GB cancer patients and in 1.8% of the T1a GB cancer patients, respectively (P < 0.01). Eight patients (1.1%) with T1a GB cancer and 52 patients (9.3%) with T1b GB cancer died of recurrent GB cancer (P < 0.01).
CONCLUSION: Simple cholecystectomy represents the adequate treatment of T1a GB cancer. There is no definite evidence that extended cholecystectomy is advantageous over simple cholecystectomy for T1b GB cancer.
Keywords: Gallbladder, Cancer, Cholecystectomy, Simple, Extended
INTRODUCTION
Gallbladder (GB) cancer confined to mucosa (T1a) or muscularis (T1b) is classified as an early cancer. Because of the high prevalence of advanced stage GB cancer at presentation, early GB cancer has been less studied among all GB cancers. However, on the basis of studies performed on GB cancer, less than 10% are early GB cancers and the proportion is growing because they tend to be diagnosed after laparoscopic cholecystectomy.
Most authors would agree that T1a GB cancer is a local disease and simple cholecystectomy represents its adequate treatment, provided that the resection margin is not involved. It was reported that the incidence of lymph node metastasis of GB cancer is less than 5%[1-9]. Recurrent GB cancer has been reported only in the form of case reports[2-4,10-12] and the 5-year survival rate of most GB cancer patients is approaching 100%[1,3,13-21]. Particularly, laparoscopic cholecystectomy is believed to be the adequate treatment of T1a GB cancer[4,12,14,16-20,22,23]. Although port site recurrence[24] and possible tumor seeding caused by pneumoperitoneum[25] are concerned, few cases have been reported[10,24].
It has been argued that T1b GB cancer may have spread regionally or systematically at presentation. Therefore, whether T1b GB cancer should be treated with simple cholecystectomy or extended cholecystectomy still remains debatable. Some authors believe that T1b GB cancer should be considered simply as a local disease with the following reasons. First, lymphovascular and perineural invasion and lymph node metastasis are rarely found in patients with pT1b GB cancer[26]. Second, the outcome of patients with pT1b GB cancer in terms of survival after simple cholecystectomy is excellent and similar to that of patients with pT1a GB cancer when the resection margins are not invaded[10,17]. Third, extended cholecystectomy does not increase the long-term survival rate of patients with pT1b GB cancer[15,17]. Fourth, no difference has been observed in survival rates between patients who underwent subsequent laparotomy with additional resection and those who did not[7,15,17]. On the other hand, others believe that lymphovascular and perineural invasion and lymph node metastasis are more frequently found in patients with pT1b GB cancer[11,13,14], and pT1b GB cancer recurs more frequently than pT1a GB cancer[7,11,18]. Extended cholecystectomy increases the long-term survival rate of patients with pT1b GB cancer[5,11,27].
Few early GB cancer cases are available and randomized trials are difficult to conduct for the assessment of appropriate surgical procedures. Therefore, a pooled systematic analysis of the efficacy of each surgical procedure for early GB cancer is essential to establish the appropriate management of T1a and T1b GB cancer. This study was to evaluate the efficacy of simple and extended cholecystectomy for T1a or T1b GB cancer.
MATERIALS AND METHODS
Search strategy
Original studies on surgery for T1 GB cancer were searched from MEDLINE (PubMed, 1966-2008), Cochrane Library (1996-2008), EMBase (1970-2008), and CancerLit (1970-2008) using the search terms of GB, cancer/carcinoma/tumor/neoplasm.
Selection criteria
Of the identified studies, only publications in the English language were included. Selection was confined to peer-reviewed articles. Unpublished data, abstracts, case reports and case series containing less than 5 patients were excluded. Studies in which the T stage was inadequately assessed and diagnosis was other than adenocarcinoma were excluded. All surgical studies on histologically proven T1a and T1b GB cancer were included. T1a and T1b GB cancer was defined as a cancer confined to the mucosa to muscularis, respectively. Only studies describing surgical intervention (simple cholecystectomy or extended cholecystectomy, etc.) for T1a and T1b GB cancer were included. Only the most recent publications were included when the selected articles included the same or overlapping data in multiple publications.
Data extraction
Two authors (Lee SE and Kang MJ) reviewed each article and performed data extraction independently according to the predefined inclusion criteria. General information pertaining to the study design, patient number and follow-up length were recorded. Types of intervention were classified into simple cholecystectomy and extended cholecystectomy, respectively. Because the extent of extended cholecystectomy varied in each article, we defined it as cholecystectomy, regional lymph node dissection, liver resection beyond wedge resection and/or resection of other organs, respectively. The overall 5-year survival rate of patients with GB cancer was defined as the primary outcome. Secondary outcomes included mortality, morbidity, and recurrence of GB cancer. The extracted data were then cross-checked by the two authors to eliminate the discrepancy.
Statistical analysis
Data are presented as median (range) unless otherwise stated. Interpretative analyses were performed based on pooled as opposed to individuals. Since patient data could not account for censored, missing or incomplete follow-up, survival analyses could not be conducted based on these data.
RESULTS
Search results
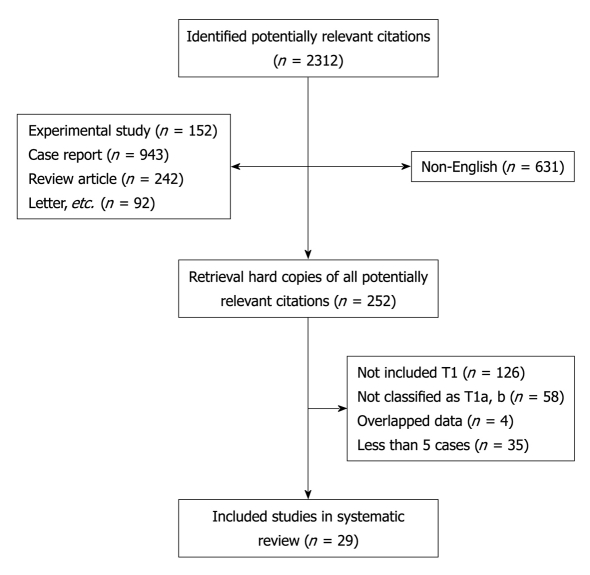
Overall, the search identified 2312 potentially relevant publications. After the titles and abstracts were reviewed, 252 publications were potentially eligible and full text reviews were conducted. Finally, 29 studies[1,3-22,24,26-32] that specifically assessed the surgical outcomes of patients with T1a and T1b GB cancer met the eligible criteria (Figure 1). There were no randomized studies and all studies were retrospective in nature. Furthermore, the majority of studies involved a small number of patients (median 15, range 5-89) except for nation-wide surveys[1,5,7,16] (Table 1).
Figure 1.
Flowchart of included articles.
Table 1.
Characteristics of included studies on surgical treatment of patients with T1 gallbladder cancer
| Authors | Yr | No. of patients |
Primary outcome |
Secondary outcome |
|||
| 3 YSR | 5 YSR | Morbidity | Mortality | Recurrence | |||
| Ogura et al[13] | 1991 | 3661 | NS | ||||
| Shirai et al[26] | 1992 | 89 | NS | NS | NS | ||
| Ouchi et al[11] | 1994 | 15 | NS | NS | |||
| Chijiiwa et al[28] | 1994 | 5 | NS | NS | |||
| de Aretxabala et al[14] | 1997 | 24 | NS | NS | NS | ||
| Mori et al[22] | 1997 | 9 | NS | NS | NS | ||
| Benoist et al[1] | 1998 | 362 | |||||
| Z'graggen et al[29] | 1998 | 9 | NS | NS | |||
| Shimada et al[9] | 2000 | 17 | NS | ||||
| Suzuki et al[30] | 2000 | 25 | NS | NS | |||
| Wakai et al[6] | 2001 | 25 | NS | NS | |||
| Puhalla et al[24] | 2002 | 9 | NS | ||||
| Wagholikar et al[7] | 2002 | 14 | NS | NS | |||
| Kim et al[17] | 2002 | 19 | NS | NS | |||
| Ouchi et al[18] | 2002 | 2343 | NS | NS | |||
| Wakai et al[10] | 2002 | 15 | NS | NS | |||
| Cucinotta et al[4] | 2005 | 12 | NS | NS | NS | ||
| Yildirim et al[15] | 2005 | 13 | |||||
| Eguchi et al[31] | 2005 | 12 | NS | NS | NS | ||
| Sun et al[19] | 2005 | 15 | NS | NS | |||
| Otero et al[32] | 2006 | 51 | NS | NS | |||
| Yagi et al[8] | 2006 | 13 | NS | NS | |||
| Chan et al[12] | 2006 | 33 | NS | NS | NS | ||
| Cangemi et al[27] | 2006 | 15 | NS | ||||
| Kang et al[16] | 2007 | 11 | NS | ||||
| You et al[3] | 2008 | 52 | NS | ||||
| Kwon et al[20] | 2008 | 20 | NS | NS | |||
| Kohya et al[21] | 2008 | 15 | NS | NS | NS | ||
| Goetze et al[5] | 2008 | 934 | NS | NS | |||
Japan survey from 172 major hospitals;
French cooperative group AURC (Association Universitaire de Recherche en Chirurgie);
Japan nationwide survey on laparoscopic cholecystectomy from 253 hospitals;
German Registry of Incidental Gallbladder Carcinoma of the German Society of Surgery. NS: Not stated.
Characteristics of the study population
Twenty-nine publications included 1266 patients with T1 GB cancer. Of these 1266 patients, 706 (55.8%) and 560 patients (44.2%) had T1a and T1b GB cancer, respectively.
Types of surgical intervention
The operative procedures performed in the 1266 patients are summarized in Table 2. Simple cholecystectomy for T1a and T1b GB cancer was performed in 590 (83.6%) and 375 (67.0%) patients, respectively (P < 0.01). Extended cholecystectomy for T1a and T1b GB cancer was performed in 110 (15.6%) and 168 (30.0%) patients, respectively (P < 0.01).
Table 2.
Surgical procedures for mucosa and T1b gallbladder cancer n (%)
| T1a (n = 706) | T1b (n = 560) | P value | Total (n = 1266) | |
| Simple cholecystectomy | 590 (83.6) | 375 (67.0) | < 0.01 | 965 (76.2) |
| Open cholecystectomy | 321 (54.4) | 286 (76.3) | < 0.01 | 607 (62.9) |
| Laparoscopic cholecystectomy | 269 (45.6) | 89 (23.7) | 358 (37.1) | |
| Extended cholecystectomy | 110 (15.6) | 168 (30.0) | < 0.01 | 278 (22.0) |
| 2nd operation | 16 (14.5) | 43 (25.6) | 59 (21.2) | |
| Major hepatectomy | 6 (0.8) | 16 (2.9) | NS | 22 (1.7) |
| Pancreatoduodenctomy | 0 | 1 (0.2) | NS | 1 |
NS: Not stated.
Postoperative morbidity and mortality
Five articles (17.2%)[1,3,15,16,24] discussed the postoperative morbidity related to the operative procedure. Complications occurred in 11 patients (11/52, 21.2%) following simple cholecystectomy, and in 21 patents (21/75, 28%) after extended cholecystectomy. Five postoperative deaths (1.0%)[1,24] occurred after simple cholecystectomy and the causes of death included acute myocardial infarction and pulmonary embolism. Seven postoperative deaths (1.5%)[1,10,11,24] occurred after extended cholecystectomy. Three patients died of co-morbidities of the disease, two patients died of hemorrhage, one patient died of peritonitis and one died of liver failure.
Lymph node metastasis
Of the 29 reviewed articles, information on lymph node metastasis was available from 17 publications (58.6%)[3,5-7,10,11,13-18,24,26-28,31] (Table 3). Lymph node metastasis was found in 1.8% and 10.9% of T1a and T1b GB cancer patients, respectively (P < 0.01). Of the 17 publications, only 5 included lymph node metastasis cases[3,5,13,15,17] (Table 4).
Table 3.
Lymph node metastasis of T1 gallbladder cancer n (%)
| T1a (n = 280) | T1b (n = 276) | P value | Total (n = 556) | |
| Lymphovascular invasion | 7 (2.5) | 33 (12.0) | < 0.01 | 40 (7.2) |
| Perineural invasion | 1 (0.4) | 7 (2.5) | NS | 8 (1.4) |
| Lymph node metastasis | 5 (1.8) | 30 (10.9) | < 0.01 | 35 (6.3) |
NS: Not stated.
Table 4.
Studies reporting lymph node metastasis of T1 gallbladder cancer n (%)
Recurrence
Information pertaining GB cancer recurrence was available from 26 out of 29 articles (89.76%)[1,3,5-8,10-13,15-22,24,26-30,32]. Eight patients (1.1%) with T1a GB cancer[3,4,10-12,18,26] and 52 patients (9.3%) with T1b GB cancer[4-7,11,12,17-19,27,32] died of recurrent GB cancer (P < 0.01). The studies reporting recurrent GB cancer are listed in Table 5. Cases of T1a GB cancer recurrence and the recurrence pattern of T1b GB cancer are summarized in Tables 6 and 7, respectively.
Table 5.
Studies reporting recurrence cases of T1 gallbladder cancer n (%)
| T1a | T1b | Odds ratio | 95% CI | |
| You et al[3] | 1/27 (3.7) | 0/25 | 0.510 | 0.39-0.67 |
| Shirai et al[26] | 2/78 (2.6) | 0/11 | 0.874 | 0.81-0.95 |
| Wakai et al[10] | 1/13 (7.7) | 0/2 | 0.923 | 0.79-1.08 |
| Z'graggen et al[29] | 0/3 | 1/6 (16.7) | 1.200 | 0.84-1.72 |
| Wagholikar et al[7] | 0/2 | 5/12 (41.7) | 1.286 | 0.91-1.82 |
| Goetze et al[5] | 0/21 | 14/72 (19.4) | 1.362 | 1.19-1.56 |
| Cangemi et al[27] | 0/4 | 5/11 (45.4) | 1.667 | 1.01-2.77 |
| Kim et al[17] | 0/10 | 1/9 (11.1) | 2.250 | 1.34-3.77 |
| Chan et al[12] | 1/14 (7.1) | 3/19 (15.8) | 2.438 | 0.23-26.29 |
| Otero et al[32] | 0/25 | 9/26 (34.6) | 2.471 | 1.71-3.57 |
| Ouchi et al[11] | 1/8 (12.5) | 3/7 (42.9) | 5.250 | 0.40-68.94 |
| Ouchi et al[18] | 1/167 (0.6) | 3/67 (4.5) | 7.781 | 0.79-76.19 |
| Cucinotta et al[4] | 1/5 (20) | 6/7 (85.7) | 24.000 | 1.14-505.2 |
| Wakai et al[6] | 0 | 2/25 (8.0) |
Table 6.
Recurrence cases of T1a gallbladder cancer after surgical treatment (n = 8)
| Operation | Time of recurrence (mo)/site | Survival after op (mo) | |
| Shirai et al[26] | NA1 | NA/CBD | 76 |
| NA1 | NA/CBD | 66 | |
| Ouchi et al[11] | Simple cholecystectomy | NA/CBD | 45 |
| Ouchi et al[18] | Laparoscopic cholecystectomy2 | NA/NA | NA |
| Wakai et al[10] | Laparoscopic cholecystectomy | NA/P. seeding | 52 |
| Cucinotta et al[4] | Laparoscopic cholecystectomy | 7/Port site | 20 |
| Chan et al[12] | Laparoscopic cholecystectomy | 48.3/liver, lung | 51 |
| You et al[3] | Laparoscopic cholecystectomy | 3/CBD | 19 |
Cystic duct margin (+) patients;
Gallbladder perforation during laparoscopic chlecystectomy. CBD: Common bile duct; NA: Not available.
Table 7.
Recurrence pattern of T1b gallbladder cancer after surgical treatment n (%)
| Simple cholecystectomy (n = 375) | Extended cholecystectomy (n = 185) | |
| Loco-regional recurrence | 12 (50.0) | |
| CBD | 3 (6.4) | |
| Lymph node | 5 (10.6) | |
| Port site | 4 (8.5) | |
| Systemic recurrence | 12 (50.0) | 3 (60) |
| Liver | 7 (14.9) | 2 (40) |
| Peritoneal seeding | 4 (8.5) | |
| Lung | 1 (2.0) | 1 (20) |
| Unknown | 23 (48.9) | 2 (40) |
| Totalb | 47 (12.5) | 5 (2.7) |
P < 0.01. CBD: Common bile duct.
Survival rate
Twenty-one publications[1,3,5-11,13-21,27,30,32] described the 5-year survival rate of GB cancer patients. The 5-year survival rate of patients with T1a and T1b GB cancer is 45%-100% and 37.5%-100%, respectively (Table 8).
Table 8.
Five-year survival rates of patients with T1a and T1b gallbladder cancer after surgical treatment
|
N |
5 YSR (%) |
|||
| T1 (T1a/T1b) | T1a (SC/EC) | T1b (SC/EC) | T1 (SC/EC) | |
| Benoist et al[1] | 361 (13/23) | 45 | 44 | 44 |
| You et al[3] | 52 (27/25) | 96.3 | 96 | 96.2 |
| de Aretxabala et al[14] | 24 (11/13) | 100 | 75 | 75 |
| Kang et al[16] | 11 (3/8) | 100 | 100 | 100 |
| Sun et al[19] | 15 (10/5) | 100 | 100 | 100 |
| Kwon et al[20] | 20 (18/2) | 100 | 100 | 100 |
| Kohya et al[21] | 15 (8/7) | 100 | 100 | 100 |
| Yildirim et al[15] | 13 (5/8) | 100 (100/100) | 80 (50/100) | 90 |
| Kim et al[17] | 19 (10/9) | 100 (100/100) | 100 (100/100) | 100 |
| Ouchi et al[11] | 15 (8/7) | (71/100) | (42/100) | |
| Cangemi et al[27] | 15 (4/11) | 100 | (37.5/100) | |
| Ogura et al[13] | 366 (201/165) | 82.6 | 72.5 | |
| Ouchi et al[18] | 234 (167/67) | 99 | 95 | |
| Otero et al[32] | 51 (25/26) | 70 | ||
| Goetze et al[5] | 93 (21/72) | (42/79) | ||
| Wakai et al[6] | 25 (0/25) | 87 (100/75) | ||
| Wagholikar et al[7] | 14 (2/12) | 68 | ||
| Shimada et al[9] | 17 (10/7) | 86.7 | ||
| Eguchi et al[31] | 25 (19/6) | 92 | ||
| Wakai et al[10] | 15 (13/2) | (90/100) | ||
| Yagi et al[8] | 13 (12/1) | 100 | ||
All patients underwent simple cholecystectomy. SC: Simple cholecystectomy; EC: Extended cholecystectomy.
Only 6 publications[5,6,11,15,17,27] compared the survival rates of patients after simple cholecystectomy or extended cholecystectomy. No significant difference was observed in the survival rate of patients with T1a GB cancer after different operative procedures. However, 3 publications[5,11,27] showed a significantly longer survival time of patients with T1b GB cancer after extended cholecystectomy (Table 9).
Table 9.
Five-year survival rates of patients with T1b gallbladder cancer after different surgical procedures
| N (SC/EC) |
5 YSR (%) |
P value | ||
| SC | EC | |||
| Wakai et al[6] | 25 (17/8) | 100 | 75 | NS |
| Kim et al[17] | 9 (6/3) | 100 | 100 | NS |
| Yildirim et al[15] | 8 (5/3) | 50 | 100 | NS |
| Ouchi et al[11] | 7 (5/2) | 42 | 100 | < 0.05 |
| Cangemi et al[27] | 11 (8/3) | 37.5 | 100 | < 0.01 |
| Goetze et al[5] | 72 (49/23) | 42 | 79 | 0.03 |
NS: Not significant; SC: Simple cholecystectomy; EC: Extended cholecystectomy.
Outcome of patients after laparoscopic cholecystectomy and open cholecystectomy
Only two studies[4,12] compared the survival rates of patients with T1 GB cancer after laparoscopic cholecystectomy and open cholecystectomy. No significant difference was observed in the survival rate of patients after the two operative procedures. However, it must be emphasized that the total number of patients included was small. In addition, 6 studies[17-20,22,30] evaluated the safety of laparoscopic cholecystectomy on the basis of recurrent GB cancer and survival rate of GB cancer patients, showing a low recurrence rate and a high survival rate (Table 10). Meta-analysis could not be performed because no studies reported the hazard ratio for overall survival rate according to the surgical procedure.
Table 10.
Clinical outcome of laparoscopic cholecystectomy for T1a and T1b gallbladder cancer
|
N |
Recurrence |
5 YSR (%) |
||||
| T1a | T1b | T1a | T1b | T1a | T1b | |
| Mori et al[22] | 7 | 2 | 0 | 0 | ||
| Kim et al[17] | 9 | 6 | 0 | 1 (port site) | 100 | 100 |
| Sun et al[19] | 10 | 5 | 0 | 0 | 100 | 100 |
| Eguchi et al[31] | 13 | 5 | 0 | 0 | 100 | 100 |
| Kwon et al[20] | 18 | 2 | 0 | 0 | 100 | 100 |
| Ouchi et al[18] | 167 | 67 | 11 | 31 | 99 | 95 |
Site was not described.
DISCUSSION
This review evaluated the surgical outcomes of patients with T1 GB cancer. The evidence was of low quality, because it was obtained from the reviewed articles, and most studies were case series. No study was controlled, and all reviewed articles were retrospective in nature. Furthermore, such studies usually involved a small number of patients, making it difficult to draw a statistically sound conclusion. The inclusion of heterogeneous groups of patients who underwent surgery at different centers by different specialists also made interpretation of results challenging. However, the relatively low incidence of this condition makes it impractical to conduct adequately powered randomized controlled trials to compare different surgical and/or nonsurgical interventions. Therefore, a systematic review of evidence despite a lower scientific level was needed.
Simple cholecystectomy for T1a GB cancer was performed in 84% of patients. Of these patients, 46% underwent laparoscopic cholecystectomy. Lymph node metastasis was found only in 1.8% GB cancer patients with a recurrence rate of 1.1%. Because 50% of the recurrence occurred in the common bile duct, pathological confirmation of cystic duct margin would be important. If cystic duct margin was proved to be positive for GB cancer, resection of the common bile duct should be performed. Although the 5-year survival rate of patients with T1a GB cancer was 45%-100%, the publications[1,11,32] showing a low survival rate did clarify that most deaths were not related to GB cancer. The remaining publications reported a 5-year survival rate of over 90%, indicating that simple cholecystectomy is the adequate surgical treatment of T1a GB cancer. In particular, recent reports[17-20,30] showed a 100% 5-year survival rate of patients with GB cancer following laparoscopic cholecystectomy, indicating that laparoscopic cholecystecotmy is a safe procedure for GB cancer. However, because a report[10] on peritoneal seeding due to GB perforation during laparoscopic cholecystectomy and a report[4] on port site recurrence following laparoscopic cholecystectomy, careful dissection to avoid perforation of GB should be performed and GB should be retrieved using a plastic bag.
Simple cholecystectomy and extended cholecystectomy for T1b GB cancer were performed in 67% and 30% patients, respectively. More patients with T1b GB cancer underwent extended cholecystectomy (P < 0.01). Despite a lack of evidence, many authors agreed that aggressive approach would be needed for T1b GB cancer. This review validated the rationale behind this approach to a certain extent. Lymph node metastasis of T1b GB cancer was 11%, which was significantly higher than that (2%) of T1a GB cancer (P < 0.01). The publications[3,5,13,15,17] reporting lymph node metastasis of T1a and T1b GB cancer showed that the incidence of lymph node metastasis of T1b GB cancer is 1.3-7 times higher than that of T1a GB cancer (Table 4). The recurrence rate of T1b GB cancer was 9%, which was significantly higher than that (1%) of T1a GB cancer (P < 0.01). The publications[3-7,10-12,17,18,26,27,29,32] reporting the recurrence rate of T1a and T1b GB cancer showed that the recurrence rate of T1b GB cancer is 1.3-24 times higher than that of T1a GB cancer (Table 7). In addition, the recurrence rate of GB cancer was higher after simple cholecystectomy than after extended cholecystectomy (12.5% vs 2.7%, P < 0.01). Although the recurrence sites were not available in 50% of the cases reviewed, no patient showed loco-regional recurrence after extended cholecystectomy in the remaining cases. The 5-year survival rate of patients with T1b GB cancer was 37.5%-100%. Studies[1,5,11,15,27] showing a 5-year survival rate of less than 50% discussed simple cholecystectomy cases. Of these publications, 3[5,11,27] showed a significantly higher survival rate after extended cholecystectomy than after simple cholecystectomy. However, the total number of patients included was too small to comment on statistical significance. Except for these studies, the rest showed a 5-year survival rate of over 80% for patients with GB cancer irrespective of surgical procedure. Although there was no definite evidence that extended cholecystectomy was advantageous over simple cholecystectomy in this review, regional lymph node dissection should be included in any surgical procedure for T1b GB cancer considering that the lymph node metastasis rate was relatively high. Although the recurrence rate of GB cancer was high and the survival rate of GB cancer patients was low after simple cholecystectomy, extended cholecystectomy was recommended for T1b GB cancer in several guidelines[33,34]. In view of the inconclusive results obtained from this review, multicenter prospective studies should be performed to clarify the surgical strategy for T1b GB cancer.
In conclusion, T1 GB cancer should be treated based on the outcomes of this review. Simple cholecystectomy for T1a GB cancer is the adequate treatment and laparoscopic cholecystectomy is a safe procedure for T1b GB cancer, provided the port site recurrence is considered. Careful dissection should be conducted considering that the peritoneal seeding is associated with bile spillage. Resection margin of cystic duct should be confirmed histopathologically with possible common bile duct resection in mind. There is no definite evidence that extended cholecystectomy is advantageous over simple cholecystectomy for T1b GB cancer. Because lymph node metastasis is considerable, regional lymphadenectomy should be performed for the treatment and staging of GB cancer.
COMMENTS
Background
Most authors agree that mucosa (T1a) gallbladder (GB) cancer is a local disease and simple cholecystectomy represents its adequate treatment provided that the resection margin is not involved. It has been argued that muscularis (T1b) GB cancers may have spread regionally or systematically at presentation. Therefore, whether T1b cancers should be treated with simple cholecystectomy or extended cholecystectomy still remains debatable.
Research frontiers
Few early GB cancer cases are available and randomized trials are difficult to conduct for the assessment of appropriate surgical procedures. Therefore, a pooled systematic analysis of the efficacy of each surgical produre for early GB cancer is essential to establish the appropriate management of T1a and T1b GB cancer.
Innovations and breakthroughs
Original published studies on surgery for T1 GB cancer were searched from MEDLINE (PubMed, 1966-2008), Cochrane Library (1996-2008), EMBase (1970-2008), and CancerLit (1970-2008).
Applications
Simple cholecystectomy for T1a GB cancer is its adequate treatment and laparoscopic cholecystectomy is safe procedure for T1b GB cancer provided the port site recurrence is considered. There is no definite evidence that extended cholecystectomy is advantageous over simple cholecystectomy for T1b GB cancer.
Terminology
GB cancer confined to T1a or T1b is as an early cancer.
Peer review
This review evaluated the surgical outcomes of T1 GB cancer. The evidence is of low quality, because it was obtained from the reviewed articles, and most studies were case series. No study was controlled and all reviewed articles were retrospective in nature. Furthermore, such studies usually involved a small number of patients, making it difficult to draw a statistically sound conclusion. The inclusion of heterogeneous groups of patients who underwent surgery at different centers by different specialists also made interpretation of results challenging. However, the relatively low incidence of GB cancer makes it impractical to conduct adequately powered randomized controlled trials comparing different surgical and/or nonsurgical interventions. Therefore, systematic review of evidence despite a lower scientific level is needed.
Footnotes
Peer reviewer: Jutta Elisabeth Lüttges, Professor, Doctor of Medicine and Professor of Pathology, Head of Department of Pathology, General Hospital Saarbrücken, Herchenbacher str.60, Riegelsberg, 66292, Germany
S- Editor Sun H L- Editor Wang XL E- Editor Zheng XM
References
- 1.Benoist S, Panis Y, Fagniez PL. Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg. 1998;175:118–122. doi: 10.1016/s0002-9610(97)00269-9. [DOI] [PubMed] [Google Scholar]
- 2.Shirai Y, Yoshida K, Tsukada K, Muto T. Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg. 1992;215:326–331. doi: 10.1097/00000658-199204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.You DD, Lee HG, Paik KY, Heo JS, Choi SH, Choi DW. What is an adequate extent of resection for T1 gallbladder cancers? Ann Surg. 2008;247:835–838. doi: 10.1097/SLA.0b013e3181675842. [DOI] [PubMed] [Google Scholar]
- 4.Cucinotta E, Lorenzini C, Melita G, Iapichino G, Currò G. Incidental gall bladder carcinoma: does the surgical approach influence the outcome? ANZ J Surg. 2005;75:795–798. doi: 10.1111/j.1445-2197.2005.03528.x. [DOI] [PubMed] [Google Scholar]
- 5.Goetze TO, Paolucci V. Immediate re-resection of T1 incidental gallbladder carcinomas: a survival analysis of the German Registry. Surg Endosc. 2008;22:2462–2465. doi: 10.1007/s00464-008-9747-9. [DOI] [PubMed] [Google Scholar]
- 6.Wakai T, Shirai Y, Yokoyama N, Nagakura S, Watanabe H, Hatakeyama K. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001;88:675–678. doi: 10.1046/j.1365-2168.2001.01749.x. [DOI] [PubMed] [Google Scholar]
- 7.Wagholikar GD, Behari A, Krishnani N, Kumar A, Sikora SS, Saxena R, Kapoor VK. Early gallbladder cancer. J Am Coll Surg. 2002;194:137–141. doi: 10.1016/s1072-7515(01)01136-x. [DOI] [PubMed] [Google Scholar]
- 8.Yagi H, Shimazu M, Kawachi S, Tanabe M, Aiura K, Wakabayashi G, Ueda M, Nakamura Y, Kitajima M. Retrospective analysis of outcome in 63 gallbladder carcinoma patients after radical resection. J Hepatobiliary Pancreat Surg. 2006;13:530–536. doi: 10.1007/s00534-006-1104-6. [DOI] [PubMed] [Google Scholar]
- 9.Shimada H, Endo I, Fujii Y, Kamiya N, Masunari H, Kunihiro O, Tanaka K, Misuta K, Togo S. Appraisal of surgical resection of gallbladder cancer with special reference to lymph node dissection. Langenbecks Arch Surg. 2000;385:509–514. doi: 10.1007/s004230000163. [DOI] [PubMed] [Google Scholar]
- 10.Wakai T, Shirai Y, Hatakeyama K. Radical second resection provides survival benefit for patients with T2 gallbladder carcinoma first discovered after laparoscopic cholecystectomy. World J Surg. 2002;26:867–871. doi: 10.1007/s00268-002-6274-z. [DOI] [PubMed] [Google Scholar]
- 11.Ouchi K, Suzuki M, Tominaga T, Saijo S, Matsuno S. Survival after surgery for cancer of the gallbladder. Br J Surg. 1994;81:1655–1657. doi: 10.1002/bjs.1800811131. [DOI] [PubMed] [Google Scholar]
- 12.Chan KM, Yeh TS, Jan YY, Chen MF. Laparoscopic cholecystectomy for early gallbladder carcinoma: long-term outcome in comparison with conventional open cholecystectomy. Surg Endosc. 2006;20:1867–1871. doi: 10.1007/s00464-005-0195-5. [DOI] [PubMed] [Google Scholar]
- 13.Ogura Y, Mizumoto R, Isaji S, Kusuda T, Matsuda S, Tabata M. Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg. 1991;15:337–343. doi: 10.1007/BF01658725. [DOI] [PubMed] [Google Scholar]
- 14.de Aretxabala XA, Roa IS, Burgos LA, Araya JC, Villaseca MA, Silva JA. Curative resection in potentially resectable tumours of the gallbladder. Eur J Surg. 1997;163:419–426. [PubMed] [Google Scholar]
- 15.Yildirim E, Celen O, Gulben K, Berberoglu U. The surgical management of incidental gallbladder carcinoma. Eur J Surg Oncol. 2005;31:45–52. doi: 10.1016/j.ejso.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Kang CM, Lee WJ, Choi GH, Kim JY, Kim KS, Choi JS, Kim BR. Does "clinical" R0 have validity in the choice of simple cholecystectomy for gallbladder carcinoma? J Gastrointest Surg. 2007;11:1309–1316. doi: 10.1007/s11605-007-0225-9. [DOI] [PubMed] [Google Scholar]
- 17.Kim EK, Lee SK, Kim WW. Does laparoscopic surgery have a role in the treatment of gallbladder cancer? J Hepatobiliary Pancreat Surg. 2002;9:559–563. doi: 10.1007/s005340200074. [DOI] [PubMed] [Google Scholar]
- 18.Ouchi K, Mikuni J, Kakugawa Y. Laparoscopic cholecystectomy for gallbladder carcinoma: results of a Japanese survey of 498 patients. J Hepatobiliary Pancreat Surg. 2002;9:256–260. doi: 10.1007/s005340200028. [DOI] [PubMed] [Google Scholar]
- 19.Sun CD, Zhang BY, Wu LQ, Lee WJ. Laparoscopic cholecystectomy for treatment of unexpected early-stage gallbladder cancer. J Surg Oncol. 2005;91:253–257. doi: 10.1002/jso.20318. [DOI] [PubMed] [Google Scholar]
- 20.Kwon AH, Imamura A, Kitade H, Kamiyama Y. Unsuspected gallbladder cancer diagnosed during or after laparoscopic cholecystectomy. J Surg Oncol. 2008;97:241–245. doi: 10.1002/jso.20944. [DOI] [PubMed] [Google Scholar]
- 21.Kohya N, Miyazaki K. Hepatectomy of segment 4a and 5 combined with extra-hepatic bile duct resection for T2 and T3 gallbladder carcinoma. J Surg Oncol. 2008;97:498–502. doi: 10.1002/jso.20982. [DOI] [PubMed] [Google Scholar]
- 22.Mori T, Souda S, Hashimoto J, Yoshikawa Y, Ohshima M. Unsuspected gallbladder cancer diagnosed by laparoscopic cholecystectomy: a clinicopathological study. Surg Today. 1997;27:710–713. doi: 10.1007/BF02384982. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki K, Kimura T, Ogawa H. Is laparoscopic cholecystectomy hazardous for gallbladder cancer? Surgery. 1998;123:311–314. [PubMed] [Google Scholar]
- 24.Puhalla H, Wild T, Bareck E, Pokorny H, Ploner M, Soliman T, Stremitzer S, Depisch D, Laengle F, Gruenberger T. Long-term follow-up of surgically treated gallbladder cancer patients. Eur J Surg Oncol. 2002;28:857–863. doi: 10.1053/ejso.2002.1301. [DOI] [PubMed] [Google Scholar]
- 25.Jacobi CA, Sabat R, Böhm B, Zieren HU, Volk HD, Müller JM. Pneumoperitoneum with carbon dioxide stimulates growth of malignant colonic cells. Surgery. 1997;121:72–78. doi: 10.1016/s0039-6060(97)90185-9. [DOI] [PubMed] [Google Scholar]
- 26.Shirai Y, Yoshida K, Tsukada K, Muto T, Watanabe H. Early carcinoma of the gallbladder. Eur J Surg. 1992;158:545–548. [PubMed] [Google Scholar]
- 27.Cangemi V, Fiori E, Picchi C, De Cesare A, Cangemi R, Galati G, Volpino P. Early gallbladder carcinoma: a single-center experience. Tumori. 2006;92:487–490. doi: 10.1177/030089160609200604. [DOI] [PubMed] [Google Scholar]
- 28.Chijiiwa K, Tanaka M. Carcinoma of the gallbladder: an appraisal of surgical resection. Surgery. 1994;115:751–756. [PubMed] [Google Scholar]
- 29.Z'graggen K, Birrer S, Maurer CA, Wehrli H, Klaiber C, Baer HU. Incidence of port site recurrence after laparoscopic cholecystectomy for preoperatively unsuspected gallbladder carcinoma. Surgery. 1998;124:831–838. [PubMed] [Google Scholar]
- 30.Suzuki K, Kimura T, Ogawa H. Long-term prognosis of gallbladder cancer diagnosed after laparoscopic cholecystectomy. Surg Endosc. 2000;14:712–716. doi: 10.1007/s004640000145. [DOI] [PubMed] [Google Scholar]
- 31.Eguchi H, Ishikawa O, Ohigashi H, Kasugai T, Yokoyama S, Yamada T, Doki Y, Murata K, Miyashiro I, Sasaki Y, et al. Surgical significance of superficial cancer spread in early gallbladder cancer. Jpn J Clin Oncol. 2005;35:134–138. doi: 10.1093/jjco/hyi042. [DOI] [PubMed] [Google Scholar]
- 32.Otero JC, Proske A, Vallilengua C, Luján M, Poletto L, Pezzotto SM, Fein L, Otero JR, Celoria G. Gallbladder cancer: surgical results after cholecystectomy in 25 patients with lamina propria invasion and 26 patients with muscular layer invasion. J Hepatobiliary Pancreat Surg. 2006;13:562–566. doi: 10.1007/s00534-006-1123-3. [DOI] [PubMed] [Google Scholar]
- 33.Eckel F, Brunner T, Jelic S. Biliary cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v65–v69. doi: 10.1093/annonc/mdq167. [DOI] [PubMed] [Google Scholar]
- 34.Benson AB 3rd, Abrams TA, Ben-Josef E, Bloomston PM, Botha JF, Clary BM, Covey A, Curley SA, D'Angelica MI, Davila R, et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw. 2009;7:350–391. doi: 10.6004/jnccn.2009.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]