Abstract
Purpose of review
High-resolution manometry (HRM) coupled with high-resolution esophageal topography plots (HREPT) has dramatically changed the paradigm of manometric studies. The purpose of the current review is to discuss the salient advantages of HRM that are likely to change the clinical practice of manometry.
Recent findings
Recent studies evaluating HRM suggest a significant improvement in the sensitivity for the diagnosis of achalasia when compared with conventional manometry. By reproducibly subtyping achalasia into classic achalasia, achalasia with pressurization, or spastic achalasia with differential responses to treatment, HRM has potential to predict clinical outcomes. Preliminary observations with HRM suggest that much of what was labeled distal esophageal spasm is in fact achalasia with esophageal compression and pseudorelaxation, or spastic achalasia. HRM is capable of selectively analyzing discrete esophagogastric junction contributors (lower esophageal sphincter and crural diaphragm) during deglutitive relaxation to clearly identify the site of abnormally high outflow resistance. HRM has improved the recognition of a clinically heterogeneous entity called functional obstruction with potential for directed therapy.
Summary
Improved, accurate and reproducible recognition of manometric diagnoses by HRM will allow the clinician to confidently diagnose esophageal disorders such as achalasia, direct therapy and predict outcomes.
Keywords: achalasia, diffuse esophageal spasm, esophageal pressure topography, high-resolution manometry, nutcracker esophagus
Introduction
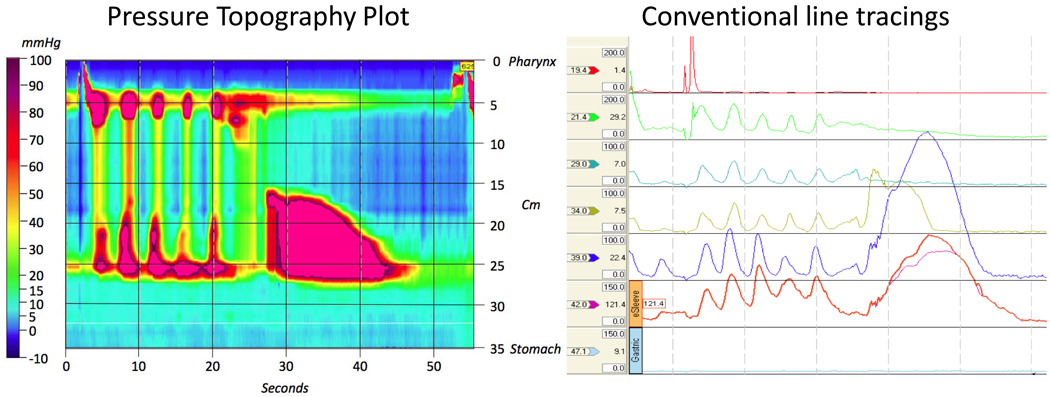
Conceptually, high-resolution manometry (HRM) refers to the use of multiple high-fidelity sensors to capture manometric data as a spatial continuum without the substantial gaps between pressure sensors typical of conventional manometry. Coupled with postrecording processing, this enhanced pressure data dramatically changes the paradigm of manometric studies. The clinician can visualize manometric data as color-encoded pressure topography plots rather than as a series of isolated line tracings, making the studies visually akin to radiographic or endoscopic evaluations of the gastrointestinal tract (Fig. 1). To distinguish these studies from conventional manometry, the term ‘high-resolution esophageal pressure topography’ (HREPT) has recently been adopted. Diagnostic algorithms for defining conventional manometric diagnoses such as achalasia are improved with HREPT, primarily due to the objectivity and accuracy with which it identifies impaired esophagogastric junction (EGJ) relaxation and the metrics of peristaltic contraction. One clear advantage of HREPT studies is in eliminating the need to reposition the recording assembly during the course of the study. As the contractile activity of the entire esophagus is simultaneously assessed, there is no need for pull-through techniques to gauge sphincter pressure. This has resulted in significant improvement in the objectivity of the EGJ evaluation, both at rest [during which time the relative contributions of the lower esophageal sphincter (LES) and crural diaphragm can be discerned], and in response to swallowing. Similarly, by providing a pressure profile of the entire esophagus in a standardized format without blank areas between sensors, HREPT depicts contraction patterns with greater reproducibility than conventional manometry.
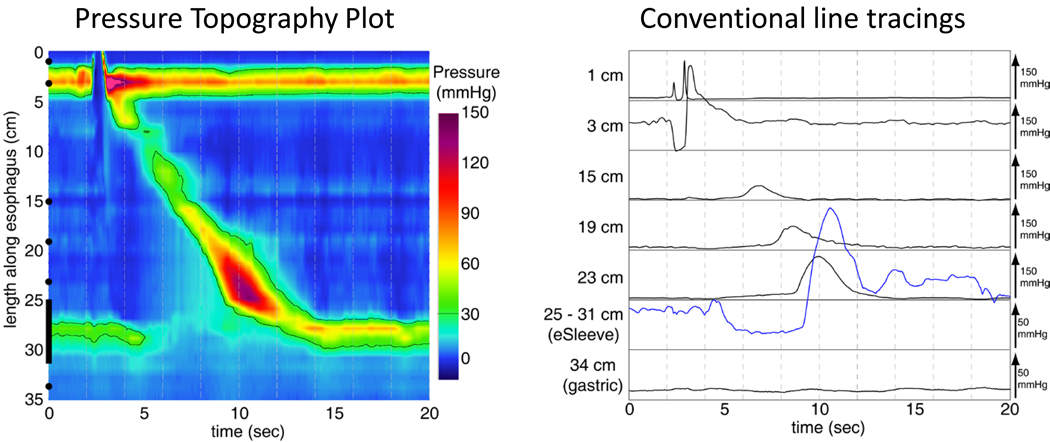
Figure 1. Esophageal pressure topography and conventional manometry of a normal swallow.
The conventional system incorporates a sleeve sensor traversing the 25–31 cm span across the sphincter, and seven other pressure sensors positioned so as to sample key physiological zones within the esophagus. In contrast to the pressure continuum of the EPT plot on the left, it is evident that substantial detail is missed by the conventional system because there is no sampling between manometric sensors.
High-resolution esophageal pressure topography versus high-resolution manometry
The mere act of capturing high-quality pressure data from a large number of closely spaced sensors (1 cm apart) by HRM does not constitute HREPT. This large quantity of data has to be presented in an interpretable manner and therein lies the value of HREPT. Simply put, HREPT is a method for viewing and analyzing manometric data, regardless of how many pressure sensors were utilized in its acquisition. Alternatively called isobaric contour plots or, in recognition of the individual who first pioneered the technique, Clouse Plots [1,2], HREPT plots lay out a coordinate system of time on the x axis, sensor position in the esophagus on the y axis, and localized pressure values represented by color, 3-D elevation, or both (Fig. 2) within that coordinate system. Pressure topography plotting can also be applied to manometric data sets with fewer sensors, but the validity of this practice is questionable once the sensor spacing widens to the point that important contractile events between sensors are missed.
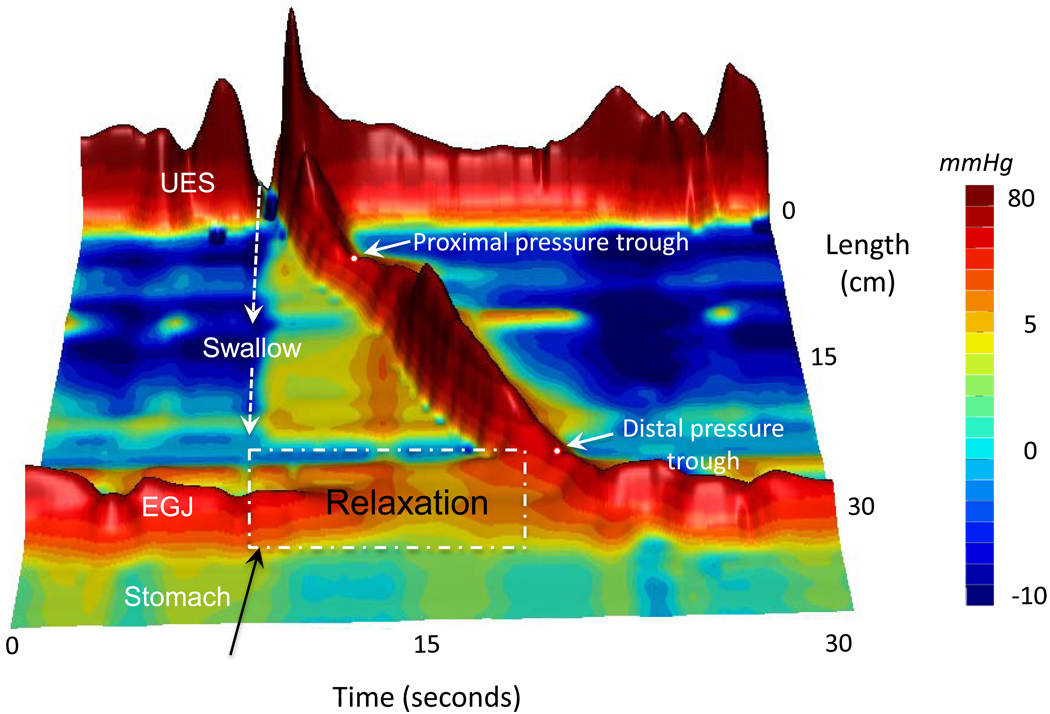
Figure 2. Landscape (3D) plots of HRM data are an alternative visualization technique that highlights regional pressure gradients and relationships.
This example illustrates the key landmarks of the normal swallow response and the normal architecture of the peristaltic contraction with two dominant pressure troughs isolating the proximal from distal esophagus and the distal esophagus from the LES.
HREPT minimizes the guesswork often associated with the positioning of conventional manometric assemblies, an essential prerequisite for obtaining high-quality tracings. By observing the locations of the upper and lower esophageal sphincters and the location of the crural diaphragm, one can readily ascertain the advancement of the HRM catheter during placement and quickly identify technical problems such as coiling of the catheter within the esophagus. As there is no need for uncomfortable and time-consuming pull-throughs or repeated repositioning of the recording assembly, HRM also improves the expediency of obtaining a complete manometric evaluation. A comparison of HRM and conventional manometry confirms that the procedure time required to complete HRM is significantly less than that for conventional manometery (mean procedure time 8.2 vs. 24.4 min, P < 0.0001) [3].
High-resolution esophageal pressure topography improves the sensitivity for the diagnosis of achalasia
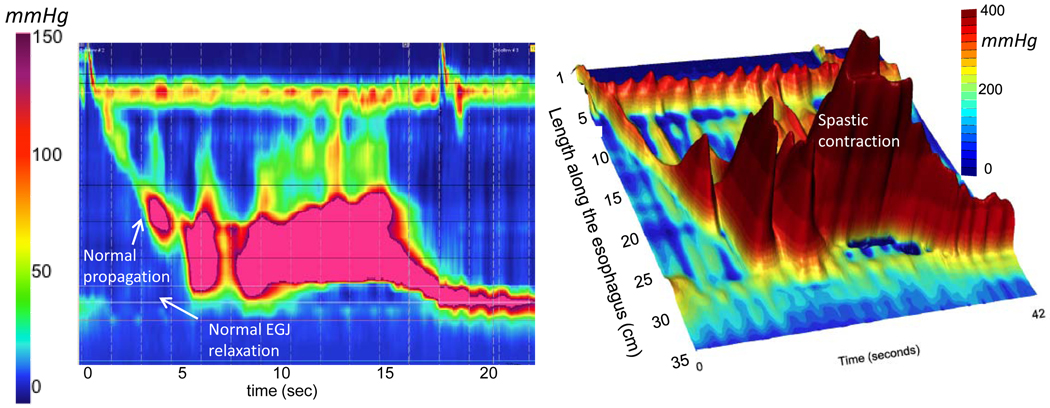
Achalasia is the best described manometric abnormality with the most well defined treatment options of all the esophageal motility disorders. The two cardinal criteria for the diagnosis of achalasia are absent peristalsis and incomplete relaxation of the EGJ (Fig. 3) [4]. However, absent peristalsis is not synonymous with absent pressurization within the body of the esophagus, and a major contribution of HREPT has been in distinguishing subtypes of achalasia by the pattern of esophageal pressurization. These distinctions were difficult to recognize with conventional manometry, which lumped these achalasia subgroups along with ‘atypical disorders of LES relaxation’ categorized as instances with some preserved peristalsis, instances of esophageal contractions with amplitudes more than 40 mmHg, and instances of complete LES relaxation but of inadequate duration. The second group was sometimes referred to as ‘vigorous achalasia’, but that terminology was discouraged in the conventional classification because no consensus existed as to whether or not such subclassification was meaningful. With HREPT, esophageal pressurization in patients with achalasia can be differentiated into that attributable to peristalsis, to elevated intrabolus pressure, or to rapidly propagated (nonperistaltic or spastic) contractions. Thus, by HREPT achalasia can be subtyped into classic achalasia (in which there is essentially no esophageal pressurization with swallowing), achalasia with esophageal pressurization, and spastic achalasia (Fig. 4). Achalasia with esophageal pressurization is characterized by compression of the water bolus between the upper and incompletely relaxing EGJ, whereas spastic achalasia is characterized by nonpropulsive, high-amplitude contractions in the body of the esophagus. Although further validation is required, it appears important to differentiate among the achalasia subtypes as there may be substantial differences in their responses to therapy, be that Botox injection, pneumatic dilation, or Heller myotomy [5••].
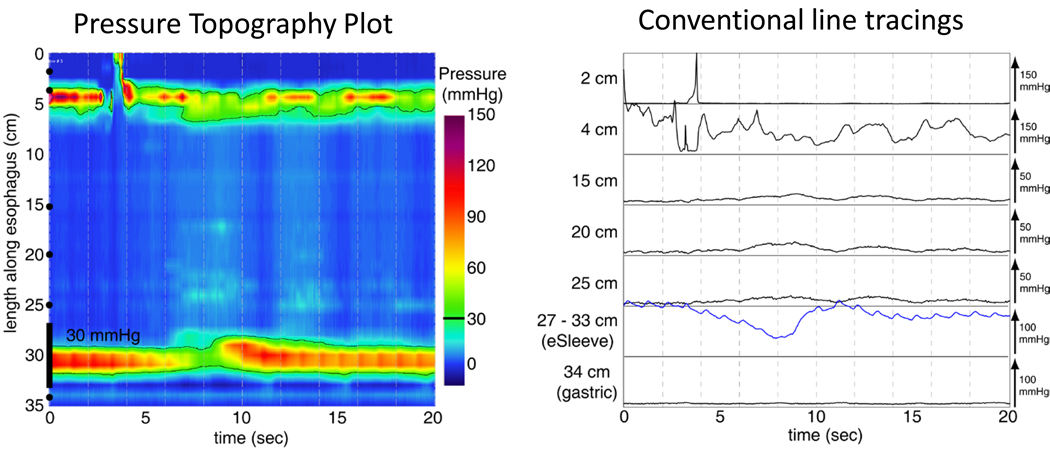
Figure 3. Classic achalasia In pressure topography and conventional manometry In the same format as Fig. 1.
Both illustrate the cardinal features of absent peristalsis and impaired deglutitive EGJ relaxation.
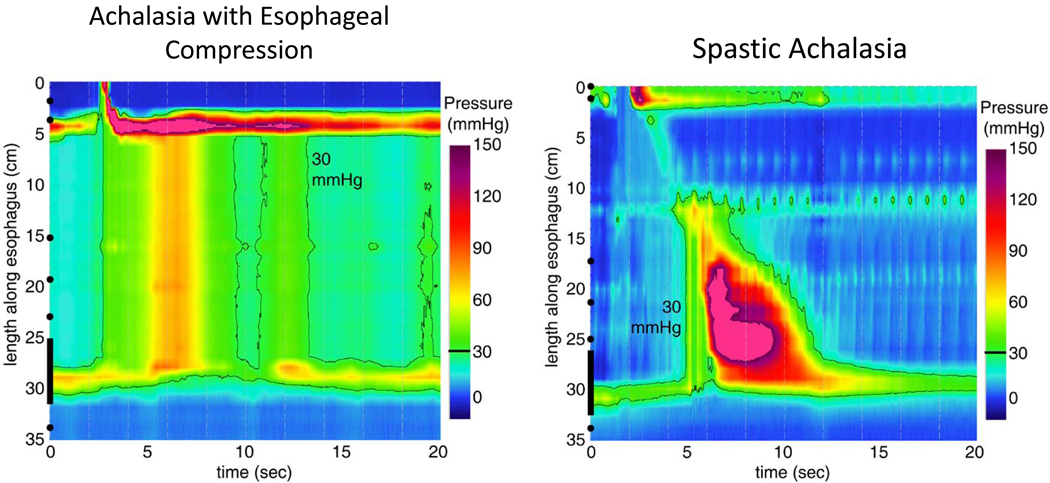
Figure 4. Subtypes of achalasia distinguished by EPT characteristics.
In achalasia with esophageal compression, no lumen obliterating contraction occurs but the esophagus empties by a global contraction in conjunction with some degree of shortening. Radiographically, there is no esophageal retention and minimal if any dilatation. In spastic achalasia, there is a lumen obliterating spastic contraction often visualized radiograpically as a corkscrew esophagus.
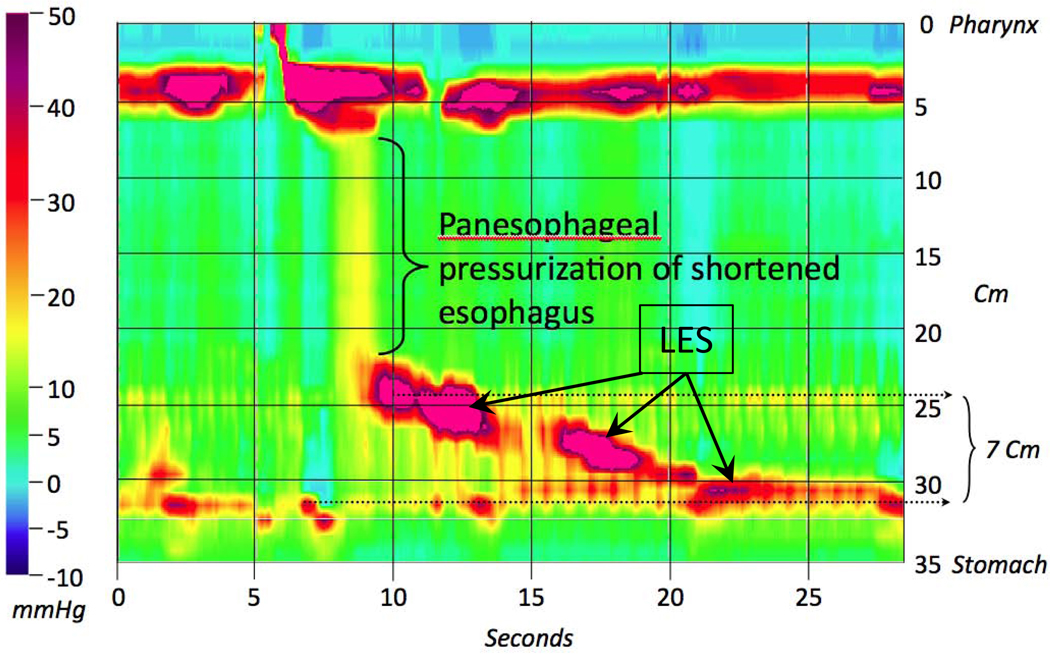
In addition to absent peristalsis, the other cardinal feature of achalasia is impaired LES (or EGJ) relaxation. Despite the key importance of this feature, no universally accepted criteria were ever available for defining impaired LES relaxation by conventional manometry. With HREPT, it has been possible to standardize the measurement of EGJ relaxation, with the resulting EGJ pressure measurement representing the contributions of the LES, the crural diaphragm, and the intrabolus pressure. By HREPT, several nuances of LES relaxation emerge [6,7]. First and foremost, LES relaxation with swallowing rarely reaches the level of intragastric pressure and, when that does occur, it is only for a brief interval. Consequently, a numerical threshold incorporating both the nadir relaxation pressure and the duration with which that relaxation is sustained needs to be established. Second, the LES moves proximally at an average of 2 cm during swallowing as a consequence of longitudinal muscle contraction and esophageal shortening; in extreme instances the LES can move proximally as much as 9 cm (Fig. 5). With conventional manometry, this is a big problem because movement of the LES relative to the pressure sensor creates the appearance of sphincter relaxation when esophageal shortening causes the sensor to be relocated into the stomach. Although inadequate LES relaxation is a sine qua non for the diagnosis of achalasia, this ‘pseudorelaxation’ phenomenon could spuriously change the manometric diagnosis from achalasia to absent peristalsis, or from spastic achalasia to diffuse esophageal spasm (DES).
Figure 5. Pseudorelaxation in a case of achalasia with esophageal compression.
In this example, the LES moves 7 cm proximally after the swallow. Conventional systems would have failed to recognize this degree of axial LES displacement and would have interpreted the findings as LES relaxation (pseudorelaxation), likely resulting in a misdiagnosis of DES.
The problem of pseudorelaxation limited the sensitivity of conventional manometry for diagnosing achalasia. To correct that problem, the HREPT-EGJ relaxation metric of the integrated relaxation pressure (IRP) was developed [7]. The IRP, which is measured within the deglutitive window beginning at the time of initiation of the swallow until the arrival of the peristaltic contraction at the LES (or 10 s in the absence of peristalsis), captures the axial movement of the LES that is attributable to longitudinal muscle contraction. The IRP is similar to measuring EGJ relaxation with an older device called a Dent sleeve, with the added stipulation that the relaxation pressure being reported is the average value persisting for a period of up to 4 s after the swallow. The improved sensitivity of the IRP measure compared with using the nadir relaxation pressure or even the HREPT-nadir relaxation pressure is evident in Table 1, which shows the sensitivity of each for detecting impaired EGJ relaxation in a series of 62 well defined patients with achalasia. This improvement is of clinical importance because the failure to detect impaired EGJ relaxation by conventional manometry resulted in spurious alternative diagnoses, most commonly ineffective esophageal motility or DES (Fig. 6) [4]. The improved sensitivity of HREPT may also allow for early detection of achalasia, before there is dilatation and deformity of the esophagus that can adversely influence the response to treatment [5••].
Table 1.
Relative performance of nadir LES pressure versus integrated relaxation pressure (IRP) in the detection of 62 well defined achalasia cases. Adapted from Ghosh SK, et al. 2007
| EGJ relaxation measure | Achalasia sensitivity (n = 62) | False positive | False negative |
|---|---|---|---|
| Single sensor nadir (<7 mmHg) | 52% | 0 | 48% |
| High resolution nadir (<10 mmHg) | 69% | 0 | 31% |
| 4s integrated relaxation pressure (<15 mmHg) | 97% | 0 | 3% |
Figure 6. EPT and conventional tracings in a case of spastic achalasia demonstrating how similar this can appear to DES.
However, there is a clear impairment of EGJ relaxation, which in conjunction with absent peristalsis establishes this as a case of spastic achalasia.
High-resolution esophageal pressure topography allows a comprehensive evaluation of impaired esophagogastric junction components
A key objective of esophageal function testing is to identify predictors of successful bolus transit, as impaired bolus transit is a key feature of esophageal motility disorders. Bolus transport through the esophagus and across the EGJ is effected by a combination of esophageal closure pressure and intraluminal pressure gradients generated by the interplay among the closure pressure (peristaltic amplitude), intrabolus pressure and EGJ outflow resistance attributable to both the LES and crural diaphragm. Due to limited spatial resolution, conventional manometry usually cannot discriminate between the crural diaphragm and LES components of the EGJ. Similarly, no measure of intrabolus pressure, which reflects outflow obstruction due to incomplete EGJ relaxation, hiatal hernia or stricture, has ever been validated in conventional manometry.
An example of the enhanced interpretation feasible with HREPT is in selectively analyzing discrete EGJ contributors (LES and crural diaphragm) during deglutitive relaxation. Either one of these components can potentially be the site of abnormally high outflow resistance. This was demonstrated in an analysis of a large series of clinical HREPT studies specifically focused on the interaction between dysphagia and hiatal hernia [8]. Owing to the spatial separation between the LES and crural diaphragm in patients with hiatal hernia, it is possible to independently measure the relaxation characteristics of each along with the associated distal esophageal intrabolus pressure. Hernia patients with dysphagia were compared with hernia patients with a dominant complaint related to reflux. Mean residual crural diaphragm pressure during deglutitive relaxation was significantly greater in the dysphagia patients (19 mmHg vs. 12 mmHg, P < 0,05), and this was accompanied by elevated distal esophageal intrabolus pressure, which confirms the effect of the crural diaphragm in resisting bolus transit [8].
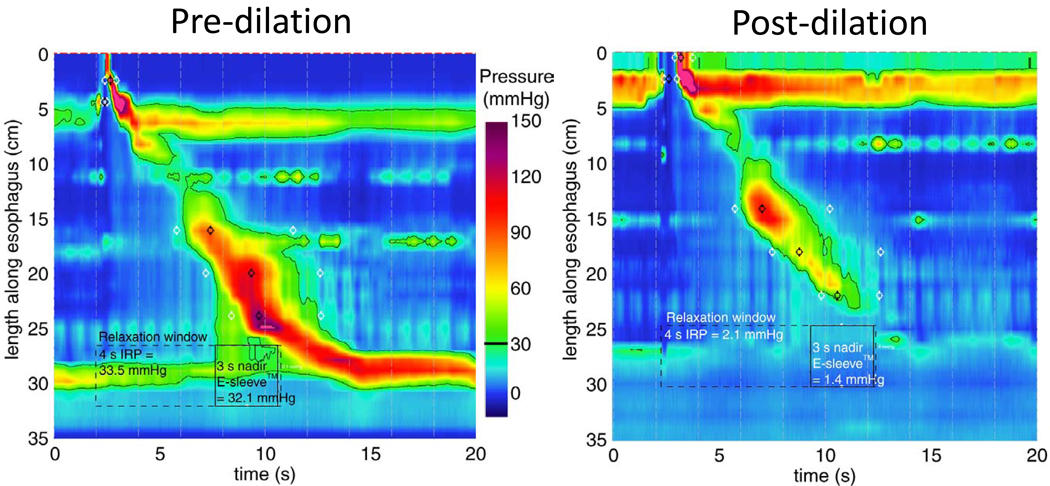
Functional impaired esophagogastric junction obstruction
With conventional manometry, patients were categorized as having ‘atypical disorder of LES relaxation’ when they met some, but not all diagnostic criteria for achalasia. Most commonly, there was some preserved peristalsis or pressurization within the body of the esophagus. Most, but not all, such dilemmas are resolved with HREPT subtyping into classic achalasia, achalasia with pressurization, or spastic achalasia. However, even with HREPT, there are still instances in which individuals demonstrate impaired deglutitive EGJ relaxation with some preserved esophageal peristalsis. These are classified as ‘functional EGJ obstruction’ and comprise a heterogeneous group of disorders that include eosinophilic esophagitis, mechanical obstruction, hiatus hernia (sliding or paraesophageal) or achalasia variants. Given the multiple potential etiologies, it is essential that patients who have functional EGJ obstruction be thoroughly evaluated before embarking on achalasia treatments. The contention that some such cases are indeed variant achalasia is supported by several lines of evidence: immunohistochemical evaluation revealed lack of myenteric ganglia and neuronal nitric oxide synthase in one such case [9], impaired EGJ relaxation can be associated with dysphagia and elevated distal esophageal intrabolus pressure (32 ± 6 vs. 11 ± 4 mmHg in controls, P < 0.05), a significant clinical improvement has been noted in a small number of functional EGJ obstruction patients treated with either Heller myotomy or pneumatic dilation (Fig. 7) [10•]. Nevertheless, this is a difficult clinical scenario and further studies are clearly needed to better delineate subtypes of functional obstruction based on the structural findings and therapeutic outcomes.
Figure 7. Functional EGJ obstruction before and after pneumatic dilation.
Prior to dilation, nadir EGJ relaxation was greater than 30 mmHg as indicated by the unbroken black 30 mmHg isobaric contour. This is associated with obvious distal esophageal intrabolus pressure. Following the (effective) dilation, LES pressure has been ablated and there appears to be a normal peristaltic contraction without distal esophageal intrabolus pressure.
Diffuse esophageal spasm
DES, which is characterized by simultaneous esophageal contractions, is a poorly understood manometric abnormality that does not always correlate with symptoms [11], is poorly reproducible on repeat manometry [11], and is said to evolve into achalasia in 3–5% of patients [12,13]. These limitations seriously call into question the validity of the current diagnostic criteria for DES by conventional manometry. Furthermore, preliminary observations with HREPT suggest that much of what had been labeled DES by conventional manometry was in fact achalasia (spastic or esophageal compression subtypes) with pseudorelaxation (Fig. 6) [14]. Similarly, what appear to be simultaneous contractions of low amplitude by conventional manometry are almost invariably attributable to intrabolus pressure in the setting of a failed peristaltic contraction with subtle obstruction in the distal esophagus. Comparing 400 patients with 75 controls, Pandolfino et al. [15••] showed that by accurately detecting intraesophageal pressurization, as many as 40% of the patients with DES by conventional criteria were reclassified as compartmentalized pressurization, an entity best dealt with by treatments directed at the EGJ. It appears that true DES defined by spastic contraction of the distal esophagus with normal EGJ relaxation (see Fig. 5) is decidedly rare.
Although observations with HREPT suggest that much of what had been considered DES is best considered something else, there are evolving HREPT criteria for hypercontractile disorders like the nutcracker esophagus. These disorders are identified by an abnormally high Distal Contractile Integral (DCI), which integrates the length, contractile amplitude, and duration of contraction of the distal esophageal segment. The DCI is expressed as mmHg s cm, with a normal mean value (10 swallows) being less than 5000 [14,15••]. Unlike DES, spastic nutcracker contractions have a normally propagated contractile front and, hence, do not represent simultaneous contractions (Fig. 8). Rather they have abnormal persistence of contraction, usually with repetitive contractions in the distal esophageal segment. Currently, the diagnostic criteria differentiating hypertensive peristalsis from spastic nutcracker are still in flux as refinements in measurement techniques evolve. However, it appears that having two swallows with average DCI more than 10 000 mmHg s cm will evolve as the distinguishing diagnostic threshold. The importance of this is that spastic nutcracker is the dominant nonachalasia motor disorder of the esophagus. Unlike manometric diagnoses based on the rapidity of propagation, this is a rare but consistent finding among centers. In all likelihood, spastic nutcracker will evolve as the dominant nonachalasia spastic disorder. Affected patients may have chest pain and dysphagia, and are sufficiently homogeneous clinically as to be the object of future therapeutic trials.
Figure 8. Spastic nutcracker contraction with normal EGJ relaxation, normally propagated peristalsis and a markedly abnormal ensuing contraction with DCI more than 50 000 mmHg·s·cm.
Conclusion
In summary, HREPT is a new methodology for assessing esophageal motility that integrates HRM with pressure topography plotting. HREPT, the product of technological advancements, is intended to replace rather than complement conventional manometry. The most obvious advantage of HREPT over conventional manometry is its improved sensitivity and accuracy for detecting achalasia. This is largely due to the objectivity with which it identifies impaired EGJ relaxation and differentiates between luminai pressures generated by contraction as opposed to obstruction. Additionally, HREPT has led to the subcategorization of achalasia that correlates with its responsiveness to treatment. Headway has also been made in understanding hypercontractile conditions, including DES. The most consistent form of esophageal spasm observed with HREPT is a newly described entity of spastic nutcracker that is an excellent target for future study.
Acknowledgements
Author guarantor of the manuscript is Peter J Kahrilas.
Author’s contribution to the paper Conceived and authored.
This work was supported by R01 DK56033 from the Public Health Service (PJK) and a Career Development Grant from the American College of Gastroenterology.
References and recommended reading
Paper of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (pp. 409–410).
- 1.Clouse RE, Staiano A. Topography of the esophageal peristaltic pressure wave. Am J Physiol. 1991;261:G677–G684. doi: 10.1152/ajpgi.1991.261.4.G677. [DOI] [PubMed] [Google Scholar]
- 2.Clouse RE, Staiano A, Alrakawi A, Haroian L. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 2000;95:2720–2730. doi: 10.1111/j.1572-0241.2000.03178.x. [DOI] [PubMed] [Google Scholar]
- 3.Salvador R, Dubecz A, Polomsky M, et al. A new era in esophageal diagnostics: the image-based paradigm of high-resolution manometry. J Am Coll Surg. 2009;208:1035–1044. doi: 10.1016/j.jamcollsurg.2009.02.049. [DOI] [PubMed] [Google Scholar]
- 4.Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut. 2001;49:145–151. doi: 10.1136/gut.49.1.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. For the first time, this large study of patients with achalasia classified three subtypes based on high-resolution manometry and linked them to clinical outcomes.
- 6.Pandolfino JE, Ghosh SK, Zhang Q, et al. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol. 2006;290:G1033–G1040. doi: 10.1152/ajpgi.00444.2005. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol. 2007;293:G878–G885. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 8.Pandolfino JE, Kwiatek MA, Ho K, et al. Unique features of esophagogastric junction pressure topography in hiatus hernia patients with dysphagia. Surgery. 2010;147:57–64. doi: 10.1016/j.surg.2009.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirano I, Tatum RP, Shi G, et al. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology. 2001;120:789–798. doi: 10.1053/gast.2001.22539. [DOI] [PubMed] [Google Scholar]
- 10. Scherer JR, Kwiatek MA, Soper NJ, et al. Functional esophagogastric junction obstruction with intact peristalsis: a heterogeneous syndrome sometimes akin to achalasia. J Gastrointest Surg. 2009;13:2219–2225. doi: 10.1007/s11605-009-0975-7. This study will familiarize the clinician to the newly recognized entity of functional EGJ obstruction with its differential diagnosis.
- 11.Barham CP, Gotley DC, Fowler A, et al. Diffuse oesophageal spasm: diagnosis by ambulatory 24 h manometry. Gut. 1997;41:151–155. doi: 10.1136/gut.41.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kramer P, Harris LD, Donaldson RM., Jr Transition from symptomatic diffuse spasm to cardiospasm. Gut. 1967;8:115–119. doi: 10.1136/gut.8.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vantrappen G, Janssens J, Hellemans J, Coremans G. Achalasia, diffuse esophageal spasm, and related motility disorders. Gastroenterology. 1979;76:450–457. [PubMed] [Google Scholar]
- 14.Ghosh SK, Pandolfino JE, Zhang Q, et al. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol. 2006;290:G988–6997. doi: 10.1152/ajpgi.00510.2005. [DOI] [PubMed] [Google Scholar]
- 15. Pandolfino JE, Ghosh SK, Rice J, et al. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenlerol. 2008;103:27–37. doi: 10.1111/j.1572-0241.2007.01532.x. This is a large, prospective study that is a must read to understand the classification schema of high-resolution manometry.