Abstract
Background
Although there were studies about ethnic differences in aortic valve thickness and calcification that they may play a role in aortic valvular stenosis (AVS) progression, few studies about the progression rate of AVS in Asian population have been reported. The purpose of this study was to evaluate the progression rate of AVS in Korean patients.
Methods
We retrospectively analyzed 325 patients (181 men, age: 67 ± 13 years) with AVS who had 2 or more echocardiograms at least 6 months apart from 2003 to 2008. The patients with other significant valvular diseases or history of cardiac surgery were excluded. The progression rate of AVS was expressed in terms of increase in maximum aortic jet velocity per year (meter/second/year).
Results
Baseline AVS was mild in 207 (64%), moderate in 81 (25%), and severe in 37 (11%). There were no significant differences among the three groups in terms of age, gender, hypertension, smoking, and hypercholesterolemia. The mean progression rate was 0.12 ± 0.23 m/s/yr and more rapid in severe AVS (0.28 ± 0.36 m/s/yr) when compared to moderate (0.14 ± 0.26 m/s/yr) and mild AVS (0.09 ± 0.18 m/s/yr) (p < 0.001). The progression rate in bicuspid AVS was significantly higher than other AVS (0.23 ± 0.35 vs. 0.11 ± 0.20 m/s/yr, p = 0.002). By multivariate analysis, initial maximum aortic jet velocity (Beta = 0.175, p = 0.003), bicuspid aortic valve (Beta = 0.127, p = 0.029), and E velocity (Beta = -0.134, p = 0.018) were significantly associated with AVS progression.
Conclusion
The progression rate of AVS in Korean patients is slower than that reported in Western population. Therefore, ethnic difference should be considered for the follow-up of the patients with AVS.
Keywords: Aortic valvular stenosis, Natural history, Disease progression
Introduction
Aortic valvular stenosis (AVS) is a chronic and progressive disease. According to previous study in Western population, it has been shown that the rate of aortic jet velocity progression is approximately 0.3 meter/second/year (m/s/yr), the aortic valve area (AVA) decreases by 0.1 cm2/yr and the mean gradient increases by 7 to 8 mmHg/yr.1-4) Also, the rate of hemodynamic progression is associated with the severity of AVS, old age, valve calcification, and concurrent coronary artery disease.3-6)
Recently, it has been reported that there was ethnic differences in aortic valve (AV) thickness and calcification7),8) which may play a role in AVS progression. However, the study of the progression rate of AVS in the Korean population is rare.9) Therefore, the present study was performed to evaluate the progression rate of AVS in Korean patients and to determine clinical, echocardiographic, and biochemical characteristics that may have a bearing on the progression of this common clinical problem.
Methods
Study population
We retrospectively analyzed echocardiograms of all patients with AVS diagnosed by 2-D and Doppler echocardiography, and selected patients who had at least 2 echocardiography examinations at intervals of 6 months or longer apart from 2003 to 2008. Initially, 541 patients were enrolled. Exclusion criteria were the presense of other significant valvular disease, left ventricular systolic dysfunction (left ventricular ejection fraction < 40%), congenital heart disease, cardiomyopathy, permanent pacemaker, uncontrolled tachycardia or bradycardia, and history of cardiac surgery. Finally, 326 out of total 541 patients were included in this study.
Clinical data including past medical history and presence of risk factors were obtained by complete review of each patient's medical record and laboratory findings. The presence of hypercholesterolemia (total cholesterol > 200 mg/dL or patients on lipid lowering therapy), diabetes mellitus (fasting plasma glucose > 126, plasma glucose level (anytime) > 200 mg/dL, or patients on antidiabetic medication), hypertension (blood pressure ≥ 140/90 mm Hg or patients on anti-hypertensive medication) and coronary artery disease (documented previous myocardial infarction or angiographically documented coronary artery stenosis more than 50% in luminal diameter) were recorded.
This study was approved by the institutional ethical review board.
Echocardiography
Comprehensive transthoracic echocardiography was performed by commercially available equipments (Vivid 7, GE Medical system, Milwaukee, WI or Acuson 512, Siemens Medical Solution, Mountain View, CA or Sonos 5500, Philips Medical System, Andover, MA, USA). Standard M-mode, 2-D and color Doppler imaging were performed in parasternal, suprasternal, substernal, and apical views with the positional change of the patients. The first and last echocardiograms taken during the study period were used to evaluate the echocardiographic changes. Anatomic measurements were made according to ASE guideline.10) Left ventricular (LV) mass was calculated using the Devereux-modified formula11): LV mass = 0.8 {1.04 [(LVEDD + LVPW + IVS)3-LVEDD3]}+0.6. LV mass index (LVMI) was calculated from LV mass divided by body surface area (m2). AVA was measured using the continuity equation.12) AVS severity was graded on the basis of a variety of hemodynamic data, using maximum aortic jet velocity, mean pressure gradients, and valve area.10) The progression rate in those subjects was expressed by increase of maximum aortic jet velocity per year (m/s/yr). A bicuspid aortic valve (BAV) was diagnosed if only 2 leaflets were present and the commissures were in locations different from those of a normal tricuspid valve.
Statistical analysis
Continuous variables are listed as mean ± standard deviation (SD). Because a mean increase in maximum aortic jet velocity per year is 0.12 m/s, the patients were dichotomously divided into rapid (≥ 0.12 m/s/yr) and slow progressors (< 0.12 m/s/yr). Mean values were compared by the unpaired t test or ANOVA. Kruskall-Wallis test was used when the variances of the groups being compared were unequal. Categorical variables are presented as frequencies or group percentages. Differences in categorical variables were analyzed by Chi-square test or Fisher's exact test. Correlations were evaluated with Pearson's correlation coefficient. Stepwise multiple linear regression analysis was used to identify the factors which were associated with AVS progression. A p value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Baseline patients characteristics
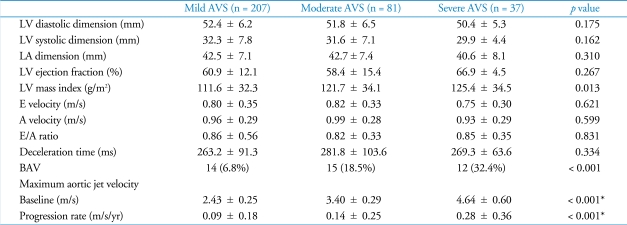
Of the 325 patients, 181 (55%) were men. Their mean age was 67 ± 13 years. The mean value of initial maximum aortic jet velocity in total patients was 2.92 ± 0.81 m/s. The AVS was mild in 207 of 326 patients (63%), moderate in 81 (25%), and severe in 37 (12%). One hundred ninety three patients (59%) had hypertension, 93 (29%) were dia-betics, 53 (17%) were current smokers, and 144 (45%) had hypercholesterolemia. There were no significant differences among the three groups in terms of age, gender, hypertension, smoking, and hypercholesterolemia. The LVMI was larger in severe AVS (125.4 ± 34.5 g/m2) compared to moderate (121.7 ± 34.1 g/m2) and mild (111.6 ± 32.3 g/m2) (p = 0.013). BAV was present in 41 (13%) and more frequent in severe AVS than in moderate and mild AVS (32% vs. 19% vs. 7%, p < 0.001). Table 1 and 2 show initial clinical and echocardiographic characteristics in each group, respectively.
Table 1.
Clinical characteristics
AVS: aortic valvular stenosis, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, LDL: low density lipoprotein, HDL: high density lipoprotein
Table 2.
Echocardiographic parameters
*analyzed by Kruskal-Wallis test AVS: aortic valvular stenosis, LV: left ventricular, LA: left atrium, BAV: bicuspid aortic valve
Progression rate of aortic valvular stenosis
The mean interval of the echocardiographic studies was 28 ± 13 months. Over this period of time, the maximum aortic jet velocity increased from 2.92 ± 0.81 to 3.19 ± 0.99 m/s and the annual progression rate of maximum aortic jet velocity was 0.12 ± 0.23 m/s/yr, indicating a wide variability in AVS progression. The annual progression rate was more rapid in severe AVS (0.28 ± 0.36 m/s/yr) compared to moderate (0.14 ± 0.25 m/s/yr) and mild AVS (0.09 ± 0.18 m/s/yr) (p < 0.001) (Fig. 1). The progression rate in bicuspid AVS was significantly higher than that of tricuspid AVS (0.23 ± 0.35 vs. 0.11 ± 0.20 m/s/yr, p = 0.001) (Fig. 2).
Fig. 1.
Progression rate of maximum aortic jet velocity according to AVS severity. Bars, mean ± SD. A p value indicates difference between groups based on scheffe's multiple comparison test. AVS: aortic valvular stenosis.
Fig. 2.
Progression rate of maximum aortic jet velocity with and without bicuspid aortic valve. Bars, mean ± SD. AVS: aortic valvular stenosis.
Comparison of rapid and slow progressors
At a mean increase in maximum aortic jet velocity per year of 0.12 m/s, the patients were dichotomously divided into rapid (≥ 0.12 m/s/yr) and slow progressors (< 0.12 m/s/yr). As shown in Table 3, the rapid progressor had higher initial maximum aortic jet velocity (p = 0.002), higher mean transvalvular gradient (p < 0.001), smaller AVA (p = 0.007), and lower E velocity (p = 0.018).
Table 3.
Comparison of rapid versus slow progressors of aortic valvular stenosis
*slow progresor n = 154, fast progressor n = 118, †slow progressor n = 113, fast progressor n = 101. BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, LV: left ventricular, LA: left atrium, BAV: bicuspid aortic valve
Multiple regression analysis for factors associated with AVS progression
A stepwise multiple regression analysis was carried out to identify the factors which were associated with the increase in maximum aortic jet velocity per year. In univariate analysis, the progression rate of AVS was significantly related to BAV, creatinine, initial maximum aortic jet velocity, LV end-diastolic dimension, left atrial dimension, and E velocity. All variables with a p-value < 0.10 in the univariate analysis were entered in the model. Annual progression rate was independently influenced by initial maximum aortic jet velocity (Beta = 0.175, p = 0.003), BAV (Beta = 0.127, p = 0.029), and E velocity (Beta = -0.134, p = 0.018). To test potential colinearity, Variance Inflation Factor (VIF) and tolerance for each independent variable were estimated. There is no problem of potential colinearity. This data is summarized in Table 4.
Table 4.
Association between the progression rate of aortic valvular stenosis and clinical and echocardiographic parameters
LV: left ventricular, LA: left atrium, BAV: bicuspid aortic valve
Discussion
Using echocardiography, previous studies have reported the natural history of AVS.1),3),4) However, the progression rate for patients with AVS has not been fully established in Asian population and it may differ from that the Western population. This retrospective study has defined the rate and variability of hemodynamic progression of AVS in Korean population and the factor associated with AVS progression. The initial maximum aortic jet velocity, mitral E velocity, and BAV are related to the rate of hemodynamic progression of AVS.
Rate of AVS progression
The mean progression rate of 0.12 ± 0.23 m/s/yr in this study is substantially less than that reported in previous studies.1),3),4) It could be explained by the result that the initial maximum aortic jet velocity in current study was lower than that in previous reports (2.92 ± 0.81 m/s vs. 3.13 ± 5.0 m/s).1),3),4) However, when the result of the previous study of 176 patients with mild and moderate AVS4) are compared to that of our subgroup whose initial maximum aortic jet velocity is similar to the former study, this explanation may not be persuasive enough. Even though initial maximum aortic jet velocity of moderate AVS in our study is similar or slightly higher than that of mild to moderate AVS in Rosenhek et al's study (3.4 ± 0.29 m/s vs. 3.13 ± 0.39 m/s), the progression rate of AVS in our subgroup is still less than that in Rosenhek et al's study (0.14 ± 0.25 m/s/yr vs. 0.24 ± 0.30 m/s/yr). The mean age of patients, which was reported to be associated with the rate of AVS progression,6) is rather higher in moderate AVS patients in current study than that of mild to moderate AVS patients in Rosenhek et al's study (67 ± 14 yrs vs. 58 ± 19 yrs) and male proportion of patients is not quite different in both groups (53% vs. 59%). In the Japanese study of 41 patients with mild to moderate AVS,13) the mean rates of progression are 0.11 ± 0.13 m/s/yr in patients under 80 yrs and 0.11 ± 0.14 m/s/yr over 80 yrs when the mean initial maximum aortic jet velocity was 2.95 ± 0.43 m/s and 2.52 ± 0.54 m/s, respectively. Those results are very similar to our findings. Also, it has been reported that there were ethnic differences in AV calcification7),8) which play an important role in progression of AVS. Therefore, the progression rate of AVS might be different according to the ethnic differences as well as other causes.
The progression rate of AVS in patients with BAV we observed is 0.23 ± 0.35 m/s/yr. It is similar to the Otto et al.'s study,1) where in 123 patients with AVS including 34 patients (28%) with bicuspid AVS, the progression rate of AVS in patients with BAV was 0.24 ± 0.30 m/s/yr.
Predictors of AVS progression
In our study, progression rate of AVS appeared to be more rapid in severe AVS than in moderate and mild. Furthermore, initial maximum aortic jet velocity was one of the independent predictors of the progression rate of AVS. The advantage of maximum aortic jet velocity as a measure of stenosis severity, when contractility is preserved, is that it is recorded directly on Doppler examination, requires no structural assumptions, and has a low intra and interobserver variability in experienced laboratories. In addition to initial AVA, Bahler et al.5) found the severity index composed of valve calcification and mobility to be the independent predictors of AVS progression. In addition, Palta et al.14) reported that initial aortic valve area, smoking, and serum calcium level were also associated with more rapid progression of AVS. However, in present study, smoking and serum calcium level did not appear to be associated with AVS progression. The severity index using aortic valvular calcification was not measured.
Our data showed that the BAV was associated with more rapid progression of AVS. There was no significant different of BAV between rapid progressor and slow progressor. However, in a stepwise multiple regression analysis, annual progression rate was independently influenced by BAV. This discrepancy would be explained by cut-off value of rapid progression. In our study, a mean increase in maximum aortic jet velocity per year of 0.12 m/s, the patients were dichotomously divided into rapid (≥ 0.12 m/s/yr) and slow progressors (< 0.12 m/s/yr). Although there was no difference in rapid and slow progressor, the progression rate of AVS was significantly related to BAV. This might be because bicuspid valves with asymmetrical leaflet sizes are more prone to rapid valve degeneration which is induced by excessive hemodynamic stress, resulting from straightening and stretching of the leaflets when they are open and close.15)
Interestingly, mitral E velocity is closely related to AVS progression in our study. In patients with AVS, diastolic dysfunction defined as either abnormal relaxation, decreased diastolic filling, or increased myocardial stiffness was observed in approximately 50% of the patients with normal systolic ejection performance, and was found in 100% of the patients with depressed systolic function.16) Thus, E velocity as the factor significantly associated with AVS progression in present study might represent diastolic dysfunction in AVS. The reason for this finding remains uncertain although diastolic dysfunction could be suggested. For better explanation, we have to consider whole diastolic parameters such as E' velocity, deceleration time, isovolumic relaxation time, and E/E' ratio. However, this is a retrospective study in a single center. We did not collect whole diastolic parameters such as E' velocity, deceleration time, isovolumic relaxation time, and E/E' ratio in every patients. Therefore, our findings should be verified by further well-controlled prospective study.
Limitations
This study has several limitations. AV calcification has been shown to be associated with more rapid progression of AVS,3),5) and ethnic difference in valve thickening and calcification might elucidate the mechanism of the slow progression of AVS in current study.7),8) Unfortunately, we did not include the grading of AV calcification by echocardiography or the quantification of AV calcification and thickness by computed tomography (CT) in this study. However, we believe the quantitation of AV calcification by echocardiography is not reliable enough because it depends significantly on the machine setting, image quality and the echocardiographer's experience. Also, we had difficulty to do CT scan in the routine evaluation of AVS because CT scan has the risk of radiation exposure. In present study, the progression rate of AVS is slower than that in previous studies conducted in Western population. However, it is hard to compare the progression rate of AVS among different studies and disclose the cause of difference in the progression rate of AVS because clinical and echocardiographic characteristics among studies are different. E velocity was significantly associated with AVS progression in our study. The reason for this finding remains uncertain although diastolic dysfunction could be suggested. For better explanation, we have to consider whole diastolic parameters such as E' velocity, deceleration time, isovolumic relaxation time, and E/E' ratio. However, this is a retrospective study in a single center. We did not collect whole diastolic parameters such as E' velocity, deceleration time, isovolumic relaxation time, and E/E' ratio in every patients. This is a retrospective study in a single center. Therefore, our findings should be verified by further well-controlled prospective study. Finally, our study focused only on hemodynamic progression, which is not synonymous with clinical progression.
In conclusion, this is the study to estimate the progression rate in Korean AVS patients. In this study, AVS progresses more rapidly in severe AVS than in moderate or mild AVS. Also, AVS severity and BAV are associated with more rapid progression of AVS. Comparing our results with previous studies, the progression rate of AVS in Korean appears to be slower than that in Western population. Therefore, ethnic differences should be considered for the follow-up of the patients with AVS.
References
- 1.Otto CM, Burwash IG, Legget ME, Munt BI, Fujioka M, Healy NL, Kraft CD, Miyake-Hull CY, Schwaegler RG. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation. 1997;95:2262–2270. doi: 10.1161/01.cir.95.9.2262. [DOI] [PubMed] [Google Scholar]
- 2.Otto CM, Pearlman AS, Gardner CL. Hemodynamic progression of aortic stenosis in adults assessed by Doppler echocardiography. J Am Coll Cardiol. 1989;13:545–550. doi: 10.1016/0735-1097(89)90590-1. [DOI] [PubMed] [Google Scholar]
- 3.Rosenhek R, Binder T, Porenta G, Lang I, Christ G, Schemper M, Maurer G, Baumgartner H. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343:611–617. doi: 10.1056/NEJM200008313430903. [DOI] [PubMed] [Google Scholar]
- 4.Rosenhek R, Klaar U, Schemper M, Scholten C, Heger M, Gabriel H, Binder T, Maurer G, Baumgartner H. Mild and moderate aortic stenosis. Natural history and risk stratification by echocardiography. Eur Heart J. 2004;25:199–205. doi: 10.1016/j.ehj.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Bahler RC, Desser DR, Finkelhor RS, Brener SJ, Youssefi M. Factors leading to progression of valvular aortic stenosis. Am J Cardiol. 1999;84:1044–1048. doi: 10.1016/s0002-9149(99)00496-8. [DOI] [PubMed] [Google Scholar]
- 6.Peter M, Hoffmann A, Parker C, Lüscher T, Burckhardt D. Progression of aortic stenosis. Role of age and concomitant coronary artery disease. Chest. 1993;103:1715–1719. doi: 10.1378/chest.103.6.1715. [DOI] [PubMed] [Google Scholar]
- 7.Sashida Y, Rodriguez CJ, Boden-Albala B, Jin Z, Elkind MS, Liu R, Rundek T, Sacco RL, DiTullio MR, Homma S. Ethnic differences in aortic valve thickness and related clinical factors. Am Heart J. 2010;159:698–704. doi: 10.1016/j.ahj.2009.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nasir K, Katz R, Takasu J, Shavelle DM, Detrano R, Lima JA, Blumenthal RS, O'Brien K, Budoff MJ. Ethnic differences between extra-coronary measures on cardiac computed tomography: multi-ethnic study of atherosclerosis (MESA) Atherosclerosis. 2008;198:104–114. doi: 10.1016/j.atherosclerosis.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sim DS, Park JC, Kim W, Kim JH, Park WS, Park OY, Ahn YK, Jeong MH, Cho JG, Oh BS, Ahn BH, Kim SH, Kang JC. Prognostic factors for medically treated patients with valvular aortic stenosis. Chonnam Med J. 2003;39:29–36. [Google Scholar]
- 10.Baumgartner H, Hung J, Bermejo J, Chambers JB, Evangelista A, Griffin BP, Iung B, Otto CM, Pellikka PA, Quiñones M American Society of Echocardiography; European Association of Echocardiography. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22:1–23. doi: 10.1016/j.echo.2008.11.029. quiz 101-2. [DOI] [PubMed] [Google Scholar]
- 11.Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458. doi: 10.1016/0002-9149(86)90771-x. [DOI] [PubMed] [Google Scholar]
- 12.Oh JK, Taliercio CP, Holmes DR, Jr, Reeder GS, Bailey KR, Seward JB, Tajik AJ. Prediction of the severity of aortic stenosis by Doppler aortic valve area determination: prospective Doppler-catheterization correlation in 100 patients. J Am Coll Cardiol. 1988;11:1227–1234. doi: 10.1016/0735-1097(88)90286-0. [DOI] [PubMed] [Google Scholar]
- 13.Kume T, Kawamoto T, Okura H, Watanabe N, Toyota E, Neishi Y, Okahashi N, Yamada R, Yoshida K. Rapid progression of mild to moderate aortic stenosis in patients older than 80 years. J Am Soc Echocardiogr. 2007;20:1243–1246. doi: 10.1016/j.echo.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 14.Palta S, Pai AM, Gill KS, Pai RG. New insights into the progression of aortic stenosis: implications for secondary prevention. Circulation. 2000;101:2497–2502. doi: 10.1161/01.cir.101.21.2497. [DOI] [PubMed] [Google Scholar]
- 15.Edwards JE. The congenital bicuspid aortic valve. Circulation. 1961;23:485–488. doi: 10.1161/01.cir.23.4.485. [DOI] [PubMed] [Google Scholar]
- 16.Villari B, Hess OM, Kaufmann P, Krogmann ON, Grimm J, Krayenbuehl HP. Effect of aortic valve stenosis (pressure overload) and regurgitation (volume overload) on left ventricular systolic and diastolic function. Am J Cardiol. 1992;69:927–934. doi: 10.1016/0002-9149(92)90795-z. [DOI] [PubMed] [Google Scholar]