Abstract
Purpose
For correction of angular deformity, tension band plating has been proposed as a safe and minimally invasive technique. The purpose of this study was to assess the experiences and report the rate of correction obtained with this procedure in patients with idiopathic genu valgum.
Methods
This study was a retrospective review of 47 valgus deformities of the knee treated with medial hemiepiphysiodesis using a tension band plate. The tibiofemoral angle (TFA) and the anatomic lateral distal femoral angle (aLDFA) were assessed on anteroposterior (AP) radiographs of the lower extremity taken at multiple time intervals. The values were charted to determine the change in orientation of the joint surface over time. Pearson’s correlation was used to analyze the correction over time. A subanalysis was performed evaluating the effect of age and the number of plates utilized.
Results
A total of 47 deformities in 25 patients were reviewed. The average time of follow-up from index surgery was 12.7 months, with an average correction of 0.96° every 3 months or 3.8° per year. The aLDFA corrected at a faster rate in knees with two plates per hemiepiphysiodesis than those with one plate, 4.2° and 3.3° per year, respectively (P = 0.035). Girls <11 years of age and boys <13 years of age corrected at a rate of 4.5°, while older children corrected at a rate of 3.4° per year (P = 0.39). There were no complications or instrumentation breakages.
Conclusion
Hemiepiphysiodesis with tension band plating provides an effective and predictable correction of idiopathic genu valgum. Two plates appear to provide a greater rate of correction. There is also a trend toward faster correction in younger patients as well.
Keywords: Tension band plate, Genu valgum, Hemiepiphysiodesis
Introduction
During early childhood development, the alignment of the knee should follow a predictable change from varus to valgus as described by Salenius and Vankka [1]. At approximately 6 years of age, this transition stabilizes at approximately 5–7° of tibiofemoral valgus. By 10 years of age, a 10° valgus deformity cannot be expected to improve spontaneously [1]. The presence of deformity leads to abnormal joint overload, which can result in future degenerative joint disease. In addition, the deformity can lead to cosmetic concerns, functional limitations, and abnormal gait mechanics [2–5].
The treatment of angular deformities of the knee has evolved significantly over time. The major principles began to take shape with the studies of Phemister and then Haas, early in the 20th century [6, 7]. Through their different studies, they showed that, by altering physeal growth, they could achieve angular correction that was simpler and safer than osteotomies. Blount subsequently popularized the technique of epiphyseal stapling [8]. He proposed the use of three staples, suggesting that this was the ideal construct to maximize the correction while minimizing the risk of hardware failure. Blount also observed that, after removing the staples, the physis recovered its ability for continued growth [3, 8, 9]. This is in contrast to methods typically performed near the end of growth which cause complete, irreversible growth arrest [9, 10]. The concern with Blount staples was that the stiffness of the staple construct and injury to the periosteum would occasionally lead to growth arrest. Therefore, it was recommended that stapling be done near the end of growth.
Recently, Stevens proposed a new construct consisting of a nonlocking extraperiosteal plate and two screws, serving as a tension band. Instead of the rigid fulcrum caused by the staples, the screws spread over time with the pivot point in the periphery. This would lead to a faster correction due to a longer moment arm. He also suggested that only one plate is required to obtain the desired tension band effect, with two plates offering no biomechanical advantage [11].
A rate of correction using a tension band plate for patients with idiopathic genu valgum has not been clearly established in the literature. Bowen et al. suggested a hypothetical 7° correction per year of angular deformity about the knee with hemiepiphysiodesis. This was determined by extrapolating longitudinal growth data from the Green–Anderson growth charts [2]. The purpose of this study is to report the experiences at our institution using the extraperiosteal plate and screw system. It was our intent to establish a rate of correction for this particular technique in patients with idiopathic genu valgum and an otherwise normal physis.
Methods
After receiving Institutional Review Board approval, a retrospective review of patients diagnosed with and treated for idiopathic genu valgum from 2005 to 2008 at our institution was performed. Data were collected from 25 patients (47 knees), all of whom received a medial distal femoral hemiepiphysiodesis with a tension band plate. Indications for surgery included residual genu valgum deformity of >10°, with anterior and/or lateral joint pain, patellofemoral instability, gait disturbance, or cosmetic concerns.
Inclusion criteria comprised of patients 16 years of old or younger with idiopathic genu valgum, and sufficient clinical and X-ray follow-up. Patients were excluded if they suffered from non-idiopathic diagnoses such as Blount’s disease, cerebral palsy, multiple hereditary exostosis, or spina bifida. Patients who had undergone previous surgeries such as an osteotomy were excluded as well. In all cases, the primary deformity was in the distal femur. Patients with a primary deformity only in the proximal tibia were excluded. However, patients undergoing a simultaneous proximal tibia hemiepiphysiodesis with tension band plating were included.
All medical records for each patient were reviewed, including clinical exams, surgical reports, and radiographs. Clinical and surgical data collection included gender, age at the time of plate insertion, diagnosis, patient history, plate and screw positioning, complications, and if treatment resulted in an endpoint of skeletal maturity or removal of the hardware. The use of one or two plates per physis was recorded (Figs. 1 and 2). Selection of the plate numbers were based on surgeon preferences. Some members of our institutions were concerned about implant failure as well as the creation of a sagittal deformity with a single plate. Therefore, they placed two plates. Others placed a single plate as recommended by Stevens [11]. All plates (either one or two) were placed using fluoroscopic guidance through a single lateral incision.
Fig. 1.
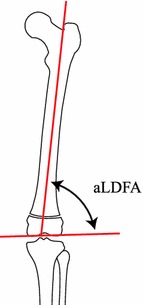
Schematic representation of the measurement of the anatomic lateral distal femoral angle (aLDFA). The angle is formed by a line parallel to the distal femur articular surface and the anatomic axis of the femur (normal = 79°–83°)
Fig. 2.
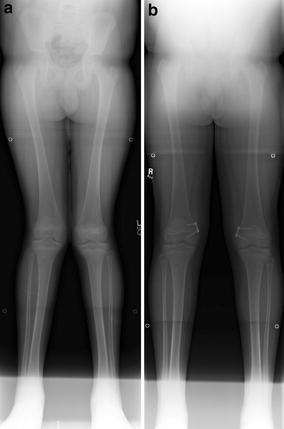
a An 11-year-old male with bilateral genu valgum (left aLDFA: 79°, right aLDFA: 75°). b The patient underwent bilateral hemiepiphysiodesis with a single tension band plate. He underwent removal at 11 months from the index procedure (left aLDFA: 88°, right aLDFA: 82°)
A review of interval radiographs from pre-operative assessment to completion of treatment was performed. Radiographic evaluation was the primary source of analysis to document the rate of correction over time by evaluating the change in orientation that the joint surface underwent as the femoral condyle alignment was modified by the hemiepiphysiodesis. A lower extremity long anteroposterior (AP) standing X-ray of all patients was obtained at their pre-operative visit and at periodic follow-up times. The anatomic tibiofemoral angle (TFA) and the anatomic lateral distal femoral angle (aLDFA) were measured for each X-ray using the methods described by Paley and Herzenberg [12]. The anatomic TFA is the angle between the anatomic lines of the femur and the tibia. The aLDFA is the angle formed between the anatomic axis of the femur and a line drawn through the knee joint line of the femur in the frontal plane (Fig. 3).
Fig. 3.

a A 12-year-old female with bilateral genu valgum (left aLDFA: 80°, right aLDFA: 80°). b The patient underwent bilateral hemiepiphysiodesis with two tension band plates. She underwent removal at 18 months from the index procedure (left aLDFA: 84°, right aLDFA: 86°)
Statistical methods
Change in both the aLDFA and the TFA were calculated for each post-operative time point (post-operative minus pre-operative value). An increase in the aLDFA value from pre-operative to post-operative indicates an improvement in alignment. Conversely, a decrease in the TFA measurement is indicative of an improvement in alignment. Variables were evaluated for normal distribution with a Q-Q plot of the residuals. Pearson’s correlation coefficient was calculated to determine whether a significant linear relationship existed between change in the aLDFA and time (represented as months post-operative). Scatter plots were produced to demonstrate these relationships. For some relationships, a regression line was fitted to provide regression coefficients—of particular interest was the slope of the regression line which yielded the rate of growth or change of angle over time. In order to compare the magnitude of the correlations found between different groups, meta-analytic techniques were calculated to evaluate for significance (significance was indicated when P ≤ 0.05). All analyses were conducted utilizing SPSS v12.0.1 (SPSS, Inc., Chicago, IL).
Results
A total of 47 idiopathic genu valgum knees in 25 patients were reviewed. Of the 47 knees, six knees also received a proximal tibial hemiepiphysiodesis with a tension band plate. Additionally, 14 patients (25 knees) received one tension band plate per physis and 11 patients (22 knees) received two tension band plates per physis. There were nine boys (16 knees) and 16 girls (31 knees), with an average age of 12.5 years (range 10–16 years) at the time of surgery. There was an average of 12.7 months follow-up from the date of surgery. Of the 25 patients analyzed, 13 patients underwent removal of hardware within the study’s timeline parameters and the average time to plate removal was 13.5 months (range 5.9–20.7 months).
The average starting TFA for all 47 knees was 11.2° (5°–16°) and the average TFA at the patients’ last follow-up was 6.0° (0°–14°), indicating an overall improved alignment. Excluding the six knees that also had a proximal tibial hemiepiphysiodesis, the average starting TFA was 11.1° (5°–16°) and the average TFA at the last follow-up was 5.7° (0°–13°). For the 47 knees, the average starting aLDFA was 78.7° (74°–84°) and the average aLDFA at the patients’ last follow-up was 83.7° (75°–91°), also indicating overall improved alignment.
A significant positive correlation was found between change in the aLDFA and time (months post-operative) (r = 0.65, P ≤ 0.001) (Fig. 4). Analysis of a regression equation indicated beta = 0.32 per month, which equates to a rate of 0.96° improvement in the aLDFA every 3 months or 3.8° in 1 year.
Fig. 4.
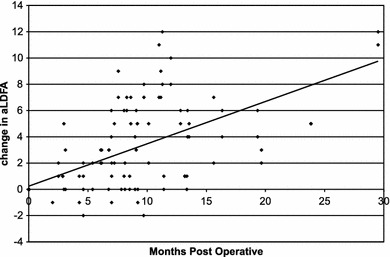
Scatterplot of change in the aLDFA over time in all patients
To determine if there was a difference in the effect secondary to the number of plates, a subanalysis was performed comparing those with one or two plates. Significant positive correlations were found between change in the aLDFA and months post-operative for both patients with one plate (r = 0.56, P ≤ 0.001) and two plates in the femur (r = 0.74, P ≤ 0.001) (Fig. 5). Patients with one plate had an average pre-operative aLDFA of 79.4° and an average aLDFA of 83.0° for the patients’ last follow-up, while patients with two plates yielded aLDFA values of 77.9° and 84.4°, respectively (Table 1). When comparing the rate of change in the aLDFA for one plate versus two plates in the femur, patients with one plate had an average of 0.81° change every 3 months (3.3° in 1 year), while patients with two plates had an average of 1.06° change every 3 months (or 4.2° in 1 year). Meta-analytic techniques indicated that the effect size r was significantly greater for patients with two plates (r = 0.74) compared to patients with only one plate (r = 0.56) in the femur (P = 0.035).
Fig. 5.
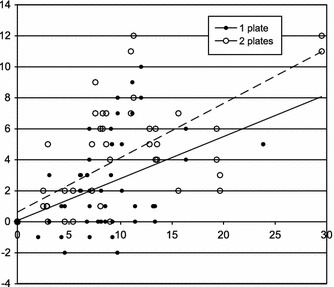
Scatterplot of change in the aLDFA for patients with one plate versus two plates in the distal femur
Table 1.
Comparison of patients with one femoral tension band plate versus two femoral tension band plates
| One plate | Two plates | |
|---|---|---|
| Age at time of surgery (years) | 12.3 | 12.9 |
| Pre-operative aLDFA | 79.4° | 77.9° |
| Final follow-up aLDFA | 83.0° | 84.4° |
| Correlation of aLDFA and time (r) | 0.56 | 0.74 |
| Rate of change (every 12 months) | 3.3° | 4.2° |
Change in the aLDFA over time was also evaluated based on age at the time of surgery by creating two age groups which correlated with the start of the peak growth velocity (boys <13 years and girls <11 years vs. boys ≥13 years and girls ≥11 years). For the younger group (boys <13 years and girls <11 years), the average pre-operative aLDFA was 79.2° and the average value for the patients’ last follow-up was 84.9°, versus 77.7° and 81.4°, respectively, for the older group (boys ≥13 years and girls ≥11 years) (Table 2). In the older group, there were a total of 16 knees, and the average change in the aLDFA after 1 year was 3.4°. For the younger group, there were a total of 31 knees, which averaged a change in the aLDFA of 4.5° after 1 year. In both groups, similar significant positive correlations were found for change in the aLDFA (younger group r = 0.697, P ≤ 0.001; older group r = 0.66, P ≤ 0.001) (Fig. 6). The effect size between the two groups, however, was not found to be significant (P = 0.39).
Table 2.
Comparison of patients based on age at the time of surgery
| Younger (boys <13 years and girls <11 years) | Older (boys ≥13 years and girls ≥11 years) | |
|---|---|---|
| Pre-operative aLDFA | 79.2° | 77.7° |
| Final follow-up aLDFA | 84.9° | 81.4° |
| Correlation of aLDFA and time (r) | 0.70 | 0.66 |
| Rate of change (every 12 months) | 4.5° | 3.4° |
Groups were correlated to the start of the peak growth velocity (boys <13 years and girls <11 years vs. boys ≥13 years and girls ≥11 years)
Fig. 6.
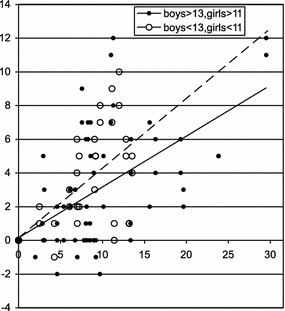
Scatterplot of aLDFA change over time for the two age groups
There were no peri-operative complications. None of the plates or screws failed in either the one plate or the two plate groups. Two patients did develop clinically significant recurvatum over time. One patient treated with bilateral medial distal femur hemiepiphysiodesis developed unilateral recurvatum of 10°. Another patient developed significant recurvatum requiring a second surgery. The re-operation consisted of implant removal and the placement of two tension band plates posterior to the original one. In both cases, it was felt that the single plates were placed too anteriorly.
Discussion
It has been well demonstrated that hemiepiphysiodesis, regardless of the technique, is a safe and easy approach to address angular deformity of the knee. Corrective osteotomy is still a viable option in cases of residual deformity at maturity and in severe cases. However, the risks of neurovascular compromise, ischemia, non-union, post-operative pain, and an extended recovery period outweigh the benefits in patients with less severe deformity [13]. Before tension band plating, staples and transphyseal screws were routinely used [3, 14–16]. The concerns were that, due to the compressive forces across the growth plate, and the possible injury to the growth plate and perichondrial ring with staple removal, physeal bars could occur. However, the greatest concern with staples was loosening, which required replacement. The tension band plate was developed in an attempt to prevent this problem. It has also been suggested that the use of plate and screws minimizes the risk of premature physeal closure, and, therefore, could be used more comfortably in younger patients. This has yet to be proven in long-term studies. The tension band system, however, has been shown to be as effective as staple hemiepiphysiodesis for the correction of angular deformities in children [15].
The aLDFA was of particular interest in this study. This angle reflects the alignment of the distal femur with relation to its anatomic axis and, therefore, is directly affected by the angular correction done by hemiepiphysiodesis. At an average follow-up of 12.7 months, the correction of the aLDFA was from 78.7° to 83.7°. Statistical analysis revealed a correction rate of 0.96° per 3 months or nearly 4° per year. Bowen et al. reported that growth after hemiepiphysiodesis, instead of being linear, behaves as an arc. Extrapolating data from the Green–Anderson chart revealed that, theoretically, 7° of angular correction per year could be obtained after femur hemiepiphysiodesis in a perfect model [2, 17]. Our data reveals that, using this technique in our patient population, 56% of this theoretical correction was obtained. Ballal et al. reported a correction rate of 0.7° per month following tension band plating, which is greater than our reported rate [18]. Their study, however, cannot be directly compared with our patients, considering that they reported on a change in TFA as opposed to the aLDFA. In addition, they had patients with both genu valgum and genu varum, which may respond differently to a hemiepiphysiodesis. Finally, their average age was 11.6 years compared to our average of 12.5 years. They reported a faster correction in younger patients, which is suggested in our study as well. Burghardt et al. found tension band plating to be effective for many different deformities around the knee and ankle [19]. They reported their results in a change in mechanical axis deviation and, similar to Ballal et al.’s study, had a younger average patient age. It is likely that many factors, including age, diagnosis, growth velocity, and the size of the physis, relate to the observed difference in the rate of correction. Our study is the first to report a rate of correction for the application of a medial distal femoral tension band plating for idiopathic genu valgum.
The rate of correction obtained in this study indicates, for the first time, the possibility that a two plate per hemiepiphysiodesis construct could provide a faster improvement than the suggested one-plate design. At 1 year after instituting treatment with two plates, the aLDFA changed an average of 4.2°, compared to 3.3° when only one plate was used. The aLDFA continued to improve at a faster velocity even after 1 year. Currently, it is not clear whether this translates into a clinically significant difference at this time. Further studies are needed. The decision to utilize one or two plates is most likely to be significant for patients near their skeletal maturity and ultimately needs to be balanced with the cost of an additional plate.
It is critical to understand the rate of correction to make accurate decisions on the timing of surgery in patients. Bone age is theoretically preferred in this instance due to providing a more objective criterion to determine the endpoint of growth. Still, no method of predicting the optimal timing for surgery has proven to be consistently accurate [20]. Combining all possible criteria is crucial for choosing the appropriate treatment, especially in patients nearing maturity or in utilizing permanent techniques. Our study would suggest that two plates provide a faster rate of deformity correction and, therefore, should also be considered when treating patients. This greater effect may be secondary to greater implant stiffness or greater physeal coverage with two plates.
Age has been identified as another factor that can independently affect the rate of correction utilizing tension band plating [18]. In our study, patients were grouped based on chronological age as related to the start of their peak growth velocity. Bone age would have been more appropriate. However, not all patients had documented bone age at the time of their index procedure. The younger patients in this study trended to a faster rate of correction than the older age group. Unfortunately, there were not enough patients in the two groups to provide significance. The differences between the age groups were not influenced by plate number, as there was a similar distribution of one and two plates in each group.
The use of one or two plates per physis was based on surgeon preference. Some members of our institution are concerned about implant failure as well as the creation of recurvatum with a single plate. Blount suggested the use of three staples to minimize hardware failure. While there were no plate/screw breakages in our study, failure of a tension band construct has been demonstrated with the use of a single plate in Blount’s disease [21]. It occurred in the metaphyseal screw and was thought to be related to excess weight and abnormal physeal anatomy. The belief is that two plates may be more resistant to breakage. The awareness of creating recurvatum has lead to the suggestion of placing a single plate slightly posteriorly. The thought is that residual posterior growth may lead to a sagittal plane change in the distal femur, resulting in knee recurvatum. Two patients with single plates in our study developed clinically significant recurvatum over time. In one patient, the implant was revised with a second plate placed more posteriorly. Further investigation is needed to truly determine if an improperly placed single plate can lead to a sagittal deformity or if two plates can mitigate this complication.
There were some limitations that we encountered in our study. The aLDFA, for study purposes, provides us with the most direct data on the effect of the plate system on angular correction of the distal femur. For clinical purposes, the assessment of the mechanical axis remains crucial, since it guides treatment recommendations. Due to poor visualization of the hips in some X-rays, we were unable to accurately obtain sufficient data on the mechanical axis (Fig. 7). This still remains a critical factor in determining indications and endpoints of treatment. In addition, we were unable to assess rebound growth due to insufficient follow-up data until skeletal maturity. It has been suggested in the literature, with the use of staples, to allow for 5° of rebound, with 1° or 2° made up by premature growth plate closure [3]. The latter fact may not be encountered with the use of a tension band plate, as it is nonrigid and may have less risk of premature physeal closure. Rebound phenomenon requires further studying, but since it is a simple and well tolerated procedure, it does not preclude re-starting treatment if it occurs [11].
Fig. 7.

Poor visualization of the hip center in some X-rays caused inability to obtain mechanical axis data in these patients
In conclusion, hemiepiphysiodesis with tension band plating is an effective and predictable method for the correction of idiopathic genu valgum. Our study demonstrates that two plates provide a greater rate of correction than one plate. There also appears to be a trend toward a faster rate of correction in younger patients as well. This study also addresses the possibility of creating a sagittal plane deformity with an improperly placed single plate. Further studies are needed in order to investigate this concern.
Acknowledgments
This study was supported by the Children’s Pediatric Orthopedic Fellowship and Education Fund.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Study conducted at Rady Children’s Hospital, San Diego, California, USA.
References
- 1.Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259–261. [PubMed] [Google Scholar]
- 2.Bowen JR, Torres RR, Forlin E. Partial epiphysiodesis to address genu varum or genu valgum. J Pediatr Orthop. 1992;12:359–364. doi: 10.1097/01241398-199205000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 4.Stevens PM, MacWilliams B, Mohr RA. Gait analysis of stapling for genu valgum. J Pediatr Orthop. 2004;24:70–74. doi: 10.1097/01241398-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Janakiramanan N, Teichtahl AJ, Wluka AE, et al. Static knee alignment is associated with the risk of unicompartmental knee cartilage defects. J Orthop Res. 2008;26:225–230. doi: 10.1002/jor.20465. [DOI] [PubMed] [Google Scholar]
- 6.Phemister DB. Operative arrestment of longitudinal growth of bones in the treatment of deformities. J Bone Joint Surg. 1933;15:1–15. [Google Scholar]
- 7.Haas SL. Retardation of bone growth by a wire loop. J Bone Joint Surg. 1945;27:25–36. [Google Scholar]
- 8.Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg Am. 1949;31A:464–478. [PubMed] [Google Scholar]
- 9.Aykut US, Yazici M, Kandemir U, et al. The effect of temporary hemiepiphyseal stapling on the growth plate: a radiologic and immunohistochemical study in rabbits. J Pediatr Orthop. 2005;25:336–341. doi: 10.1097/01.bpo.0000152906.23669.d8. [DOI] [PubMed] [Google Scholar]
- 10.Horton GA, Olney BW. Epiphysiodesis of the lower extremity: results of the percutaneous technique. J Pediatr Orthop. 1996;16:180–182. doi: 10.1097/01241398-199603000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 12.Paley D, Herzenberg JE. Principles of deformity correction. 1. Berlin: Springer; 2002. [Google Scholar]
- 13.Steel HH, Sandrow RE, Sullivan PD. Complications of tibial osteotomy in children for genu varum or valgum. Evidence that neurological changes are due to ischemia. J Bone Joint Surg Am. 1971;53:1629–1635. [PubMed] [Google Scholar]
- 14.Khoury JG, Tavares JO, McConnell S, et al. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27:623–628. doi: 10.1097/BPO.0b013e318093f4f4. [DOI] [PubMed] [Google Scholar]
- 15.Wiemann JM, 4th, Tryon C, Szalay EA. Physeal stapling versus 8-plate hemiepiphysiodesis for guided correction of angular deformity about the knee. J Pediatr Orthop. 2009;29:481–485. doi: 10.1097/BPO.0b013e3181aa24a8. [DOI] [PubMed] [Google Scholar]
- 16.Castañeda P, Urquhart B, Sullivan E, et al. Hemiepiphysiodesis for the correction of angular deformity about the knee. J Pediatr Orthop. 2008;28:188–191. doi: 10.1097/BPO.0b013e3181653ade. [DOI] [PubMed] [Google Scholar]
- 17.Anderson M, Green WT, Messner MB. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45-A:1–14. [PubMed] [Google Scholar]
- 18.Ballal MS, Bruce CE, Nayagam S. Correcting genu varum and genu valgum in children by guided growth: temporary hemiepiphysiodesis using tension band plates. J Bone Joint Surg Br. 2010;92:273–276. doi: 10.1302/0301-620X.92B2.22937. [DOI] [PubMed] [Google Scholar]
- 19.Burghardt RD, Herzenberg JE, Standard SC, et al. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008;2:187–197. doi: 10.1007/s11832-008-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Little DG, Nigo L, Aiona MD. Deficiencies of current methods for the timing of epiphysiodesis. J Pediatr Orthop. 1996;16:173–179. doi: 10.1097/01241398-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Schroerlucke S, Bertrand S, Clapp J, et al. Failure of orthofix eight-plate for the treatment of Blount disease. J Pediatr Orthop. 2009;29:57–60. doi: 10.1097/BPO.0b013e3181919b54. [DOI] [PubMed] [Google Scholar]


