Abstract
INTRODUCTION
The aims of this study were to examine the trends in performance of open and laparoscopic appendicectomy at a district general hospital, and to compare the diagnostic outcomes in the two patient groups.
PATIENTS AND METHODS
Data were collected prospectively from patients undergoing an open or laparoscopic procedure for cted appendicitis in an 8-year period between January 2000 and December 2007.
RESULTS
A total of 1700 patients (873 women, 827 men) with a median age of 24 years underwent surgery for suspected appendicitis in the study period. There were 1357 patients (group A) who underwent an open procedure for presumed appendicitis (610 women and 747 men [F:M ratio, 1:1.2]). There were 343 patients (group B) who underwent laparoscopy with or without laparoscopic appendicectomy (82 men and 261 women [F:M ratio, 1:0.31]). Over the study period, there was an increasing trend towards the performance of laparoscopic procedures for suspected appendicitis, increasing from 4% to 39% of the total per year. In group A, 1172 (86%) patients had appendicular pathology, while the appendix was normal histologi-cally in 178 (13%). Other pathologies were diagnosed intra-operatively in 1%. In group B, 193 patients (56%) had appendicular pathology while in 150 (44%) the appendix was normal. In the subgroup with a normal appendix, 56 patients (37%) had another cause for their symptoms identified.
CONCLUSIONS
Laparoscopic appendicectomy is increasingly being performed. Laparoscopy is often used as a diagnostic tool in general surgical patients, particularly women, with lower abdominal pain. In effect, these patients are undergoing diagnostic laparoscopy, with or without appendicectomy. This has resulted in a lower positive appendicectomy rate, but a higher yield of diagnoses other than appendicitis, in the laparoscopic group. Overall appendicectomy rates, however, have remained unchanged.
Keywords: Appendicectomy, Laparoscopic appendicectomy, Laparoscopy
Appendicitis remains one of the commonest conditions requiring emergency surgical intervention.1 Following the description by Charles McBurney of open appendicectomy in 1889,2 this procedure has remained the treatment of choice for appendicitis for almost 100 years. Since the introduction of laparoscopic appendicectomy by Semm in 1983,3 there has been debate about the relative merits of laparoscopic and open procedures for appendicitis.
The aim of this study was to examine the changes in the performance of laparoscopic and open appendicectomy, in patients with a diagnosis of suspected appendicitis, over a period of 8 years at a district general hospital. The study also aimed to investigate the differences in the diagnostic outcome between patients undergoing laparoscopic and open procedures, with a clinical diagnosis of suspected appendicitis.
Laparoscopic appendicectomy was introduced at our hospital in the 1990s. The decision to perform an open or a laparoscopic procedure is left to the admitting or operating surgeon. We have not produced guidelines on whether or not to remove an apparently normal appendix; the decision to do so, or to leave it in situ, is also left to the operating surgeon.
Patients and Methods
Demographic and operative data were collected prospectively from patients undergoing surgery for suspected appendicitis between January 2000 and December 2007. Age, gender, operative findings, procedures, operating surgeon, time of operation and histological diagnosis were recorded. Results in patients managed with open appendicectomy were compared to those who underwent laparoscopy with or without appendicectomy (patients undergoing open appendicectomy following initial laparoscopy were included in the laparoscopic group).
All patients who had appendicectomy performed as part of another procedure (incidental appendicectomy) were excluded from the study.
The data were retrieved from the hospital's computerised histopathology and operating theatre records. The operative notes and histopathology reports were reviewed. The data were analysed using Microsoft Excel spreadsheets.
Results
A total of 1700 patients (873 women, 827 men [F:M ratio, 1:0.94]) with a median age of 24 years (range, 2–91 years) underwent an operative procedure for suspected appendicitis in the study period.
There were 1357 patients (group A) with a median age of 24 years (range, 2–91 years) who underwent an open procedure. In group A, there were 610 women and 747 men (F:M ratio, 1:1.2). There were 343 patients (group B) with a median age 24 years (range, 9–82 years) who underwent laparoscopy with or without laparoscopic appendicectomy. In this group, there were 261 women and 82 men (F:M, ratio 1:0.31).
In the initial 12 months of the study period, 4% of patients underwent a laparoscopic procedure. In the final 12 months, this proportion had risen significantly to 39% (P < 0.0001; chi–squared = 22.310). The total number of procedures performed each year for suspected appendicitis remained unchanged (Fig. 1).
Figure 1.
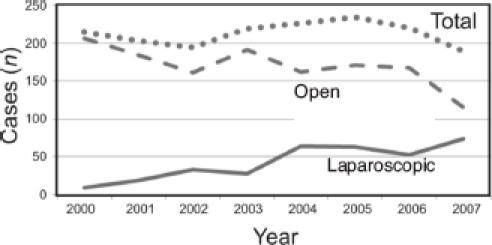
Trends in performance of laparoscopic and open appendicectomy.
In group A, 1172 (86%) patients had appendicular pathology, while the appendix was normal histologically in 178 (13%). Other pathologies were diagnosed intra-opera-tively in less than 1% (Table 1).
Table 1.
Pathological findings of group A (open appendicectomy)
| Total open procedures | 1357 |
| Appendicitis | 1161 |
| Carcinoid | 9 |
| Mucinous neoplasm of appendix | 1 |
| Adenocarcinoma of appendix | 1 |
| Normal | 178 |
| Ovarian cysts/other ovarian pathology | 7 |
In group B, 193 patients (56%) had appendicular pathology, while in 150 (44%) the appendix was considered normal in appearance at laparoscopy (Table 2). The appendix was removed in 63 patients (in whom absence of appendicitis was confirmed histologically), and left in situ in 87 (25% of group B). In this subgroup of 150 patients with a normal appendix, 56 patients (37%, or 16% of group B) had another cause for their symptoms identified, e.g. pelvic inflammatory disease, ovarian cysts, retrograde menstruation, hydrosalpinx (Fig. 2). The number of alternative diagnoses in group B was significantly higher than that in group A (P < 0.0001; chi-squares = 181.502).
Table 2.
Pathological findings of group B (laparoscopic procedure)
| Total laparoscopic procedures | 343 |
| Histological appendicitis | 189 |
| Carcinoid | 2 |
| Adenocarcinoma of appendix | 1 |
| Foreign body in appendix | 1 |
| Normal histology | 63 |
| Normal appendix on laparoscopy | 87 |
| No cause of abdominal pain | 31* |
| Alternate diagnosis on laparoscopy | 56* |
These patients had normal appendix on laparoscopy (i.e. 31 + 56 = 87).
Figure 2.

Alternative diagnoses made during the laparoscopy.
There was no difference in the timing of procedures between the two groups. The majority of procedures were performed in the evening and night time with a significant proportion being performed during routine working hours (Fig. 3).
Figure 3.
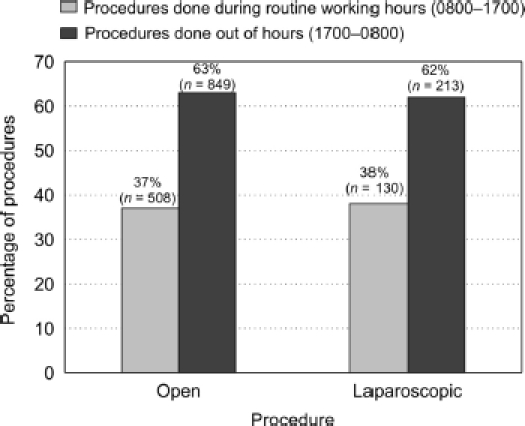
Timing of procedures.
A middle-grade doctor (specialist registrar or staff grade) performed most of procedures in both groups (75% in the open and 79% in the laparoscopic group). A consultant surgeon was the main operating surgeon in 14% of cases in the open group and 21 % in the laparoscopic group. A small proportion (10%) of cases were performed by senior house officers in the open group (Fig. 4).
Figure 4.
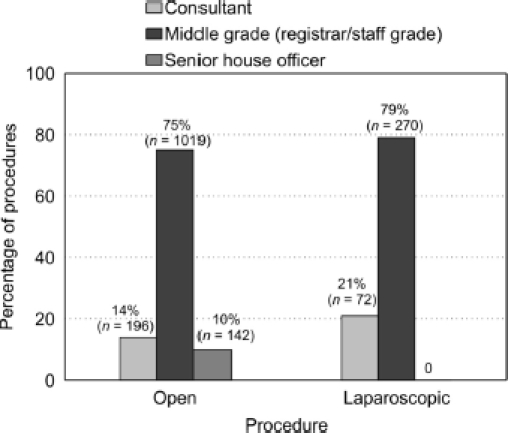
Grade of operating surgeon.
Discussion
Access by open appendicectomy allows only a limited assessment for other pathologies, and appendicectomy is usually performed even if the gross appearance of the appendix is normal. This prevents the diagnostic confusion of having appendicitis with a scar in the right iliac fossa in the future. This results in a normal appendicectomy rate of around 10–25%.1,4 The average negative appendicectomy rate in Wales was 29.2% in a recent study.5
In our study, the negative procedure (normal appendix) rate was 13% in the open appendicectomy group (group A) and 44% in the laparoscopic group (group B). The overall negative appendicectomy rate (combining groups A and B) was 19%, which compares favourably with previous studies.6–8 It is clear that, in our practice, patients undergoing laparoscopy for suspected appendicitis have a much lower rate of appendicitis than those undergoing an open procedure. Taking into consideration those patients in group B who had an alternative diagnosis, the rate of no positive findings (i.e. normal laparoscopy) was 27%, still considerably higher than that in group A. This suggests that we are using different indications for surgery in these two groups of patients. Baigrie et al.9 also found a similarly high proportion of normal appendices in one-third of laparoscopic cases, and Grabham et al.10 found similar result in their study.
Our study shows that a diagnosis other than acute appendicitis could be made in less than 1% of patients undergoing open appendicectomy, but an alternative diagnosis could be made in 16% of those undergoing a laparoscopic procedure. This may be due to the better visualisation of the intra-abdominal and pelvic organs (e.g. ovaries, fallopian tubes) which is possible during laparoscopy, compared with open appendicectomy. The laparoscopic approach, therefore, offers an advantage over the open approach, in terms of a higher yield of alternative diagnoses and may spare the patients a negative appendicectomy. The figure of 16% is higher than the negative appendicectomy rate in group A, also suggesting that the indications for surgery are different in patients undergoing open and laparoscopic surgery for suspected appendicitis. It is likely that patients with an uncertain diagnosis for their abdominal pain (often women) are being selected for laparoscopy (with or without appendicectomy), rather than open appendicectomy. There has, however, been no official policy in our hospital for such selection, although we plan to draw up such a policy in the light of this study's findings. Our overall procedure rate for acute appendicitis remained unchanged during the study period, suggesting that we have not lowered our threshold to operate in patients with suspected appendicitis. This is contrary to the suggestion made previously by McGreevy et al.,11 that the threshold for operating has lowered.
Computerised tomography (CT) was not used routinely in our study, and indeed is not widely used in our department for the diagnosis of acute appendicitis. One reason for this is concern about the radiation dose involved. However, an increase in the use of CT is an alternative diagnostic approach which could reduce the rate of negative appen-dicectomy. In a recent study, Jones et al.12 claimed to decrease the incidence of negative appendicectomy to 2% with appropriate use of computerised tomography. This approach requires further evaluation.
Conclusions
There has been a paradigm shift in the surgical management of patients with suspected appendicitis over the 8-year period in our hospital. Laparoscopy is being used increasingly as a diagnostic tool in patients, particularly women, with lower abdominal pain. These patients may or may not undergo appendicectomy, depending on laparoscopic findings and the surgeon's preference. This has not resulted in a significantly higher rate of excision of a normal appendix, but has allowed a higher yield of diagnoses other than appendicitis. There has, however, been a lower rate of finding acute appendicitis in the laparoscopic group, compared with the open appendicectomy group. This may be due to a predominance of female patients who are more likely to have other pathology, as well as those patients with an equivocal presentation who may be less likely to have appendicitis.
In view of the difference between patients selected for open or laparoscopic surgery, it is inappropriate to make direct comparison between these groups (e.g. normal appendix rates). A normal appendix rate of 44% may come to be regarded as acceptable practice for this group of predominantly female patients with uncertain clinical findings, who undergo laparoscopy with or without appendicectomy. The optimum indications for the surgical intervention, either laparoscopic or open, are yet to be established, and further studies are required.
References
- 1.Nicolson A, Patel P, Jambulingam P. Laparoscopic era yields higher negative appendicectomy rate. Br J Surg. 2008;95(Suppl 3):143. [Google Scholar]
- 2.McBurney C. Experience with early operative interference in cases of disease of the vermiform appendix. NY Med J. 1889;1:676–84. [Google Scholar]
- 3.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 4.Sweeney KJ, Keane FBV. Moving from open to laparoscopic appendicectomy. Br J Surg. 2003;90:257–8. doi: 10.1002/bjs.4070. [DOI] [PubMed] [Google Scholar]
- 5.Ansell J, Rees BI. The negative appendectomy in Wales. Ann R Coll Surg Engl. 2004;86:477–8. [Google Scholar]
- 6.Berry J, Jr, Malt RA. Appendicitis near its centenary. Ann Surg. 1984;200:567–75. doi: 10.1097/00000658-198411000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajan P, Sharma DC, Watson CJ. A retrospective review of appendicectomy management in a UK teaching hospital. Internet J Surg. 2006;7(2) < http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijs/vol7n2/appendicectomy.xml>. [Google Scholar]
- 8.Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg. 1997;174:723–6. doi: 10.1016/s0002-9610(97)00183-9. discussion 726–7. [DOI] [PubMed] [Google Scholar]
- 9.Baigrie RJ, Dehn TCB, Fowler SM, Dunn DC. Analysis of 8651 appendicectomies in England and Wales during 1992. Br J Surg. 1995;82:933. doi: 10.1002/bjs.1800820726. [DOI] [PubMed] [Google Scholar]
- 10.Grabham JA, Sutton C, Nicholson ML. Laparoscopic appendicectomy for the ‘normal’ appendix. Br J Surg. 1997;84(Suppl 2):59. [Google Scholar]
- 11.McGreevy JM, Finlayson SR, Alvarado R, Laycock WS, Birkmeyer CM, Birkmeyer JD. Laparoscopy may be lowering the threshold to operate on patients with sus pected appendicitis. Surg Endosc. 2002;16:1046–9. doi: 10.1007/s00464-001-8332-2. [DOI] [PubMed] [Google Scholar]
- 12.Jones K, Pena AA, Dunn EL, Nadalo L, Mangram AJ. Are negative appendec tomies still acceptable? Am J Surg. 2004;188:748–54. doi: 10.1016/j.amjsurg.2004.08.044. [DOI] [PubMed] [Google Scholar]


