Abstract
Chronic inflammatory demyelinating polyneuropathy (CIDP) is characterised by the occurrence of symmetrical weakness and sensory impairment in arms and legs. The course is relapsing or chronic and progressing. CIDP is considered to be an autoimmune disease, which is supported by the beneficial response to immunomodulating therapies in most patients. We report on a patient with CIDP who has been in remission for more than 3 years after treatment with high dose cyclophosphamide and autologous blood stem cell transplantation in CIDP on two occasions.
BACKGROUND
Chronic inflammatory demyelinating polyneuropathy (CIDP) is characterised by the occurrence of symmetrical weakness and sensory impairment in arms and legs. The course is relapsing or chronic and progressing. CIDP is considered to be an autoimmune disease, which is supported by the beneficial response to immunomodulating therapies in most patients.1 Benefit from treatment with corticosteroids, plasmapheresis and intravenous immunoglobulin (IVIG) has been confirmed1 but not all patients respond. Beneficial effects in previously treatment resistant CIDP have been reported for ciclosporin, etanercept, mycophenolate mofetil, rituximab and pulse cyclophosphamide treatment.1 In 2002, Brannagan et al2 reported long term remission after high dose cyclophosphamide in four patients with CIDP refractory to conventional treatment. The same year Vermeulen and Van Oers3 reported on successful autologous blood stem cell transplantation (ASCT) in one patient with CIDP. To our knowledge, no reports exist on repeated treatment with high dose cyclophosphamide and/or ASCT.
We report on a patient with CIDP who has been in remission for more than 3 years after treatment with high dose cyclophosphamide and ASCT on two occasions.
CASE PRESENTATION
A 56-year-old man presented at his local hospital in August 2001 with a history of progressive weakness in his arms and legs for 3 weeks. Neurological examination showed pronounced weakness in the limbs and areflexia. Cranial nerves, coordination and sensory function were normal. CSF showed increased protein (0.90 g/l) but no cells. The condition was diagnosed as Guillain–Barré syndrome. The patient was treated with IVIG 2 g/kg and muscle strength increased. After 3 weeks the patient deteriorated and was bedridden. Because of the short lasting effect, treatment with IVIG had to be repeated every 3 weeks. At examination in May 2002 in our department, the patient had pronounced weakness in the hands and moderate weakness in the legs. The tendon reflexes were either weak or absent. Cranial nerves and sensory functions were normal. Neurophysiological examination confirmed the clinical suspicion of CIDP. The patient deteriorated rapidly and was almost tetraparetic. He was treated with IVIG 2 g/kg, but this time without any response after 1 week. Methylprednisolone 30 mg/kg/day was given intravenously for 2 days followed by prednisone 80 mg/day. Treatment was also started with azathioprine 150 mg/day. Two weeks later the patient was substantially improved before he deteriorated again. In further attempts to treat the patient, plasmapheresis was given at 2 week intervals. Every time the patient responded rapidly, but the good response did not last more than about 10 days. When the plasmapheresis was delayed more than 2–3 days, he was bedridden and unable to lift his limbs from the bed.
Because of the difficult situation for the patient we decided to treat him with high dose cyclophosphamide and ASCT. In August 2002, we mobilised peripheral blood stem cells after a course of cyclophosphamide 3200 mg intravenously (2000 mg/m2) for 1 day followed by subcutaneous granulocyte colony stimulating factor (5 μg/kg/day) for 6 days until the stem cell harvest. In September 2002, the patient was treated with cyclophosphamide 4950 mg/day (50 mg/kg/day) for 4 days. Two days after the eradication procedure the stem cells were returned. The patient subsequently improved and the treatments with plasmapheresis were stopped in November 2002. Four weeks after the last plasmapheresis, gait, muscle strength and sensation were normal and all tendon reflexes except the Achilles reflexes could be elicited. However, approximately 2 years after the stem cell transplantation the patient relapsed. On examination in October 2004 he had mild weakness in the shoulders and feet, moderate weakness in the elbows, and pronounced weakness in the wrists, hands and hips. The patient was again treated with cyclophosphamide and underwent ASCT as described above. In addition, antithymocyte globulin was given for 2 days. As a complication he suffered a 3 week episode of fever, bronchitis and elevated liver enzymes which seemed to be caused by Epstein–Barr virus and cytomegalovirus reactivation. Muscle strength was normal at examination 3 weeks after the combined treatment, and after 3 years (October 2007) the patient still remains in clinical remission without any treatment.
INVESTIGATIONS
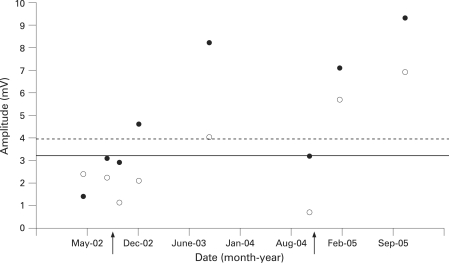
Repeated nerve conduction studies showed the typical findings of CIDP. There were signs of motor conduction blocks, reduced nerve conduction velocities and prolonged or absent F responses. Sensory nerve action potentials were either reduced in amplitude or unobtainable. It was of interest to note that the amplitudes of the compound motor action potential (CMAP) on distal nerve stimulation correlated well with the clinical condition of the patient. Figure 1 illustrates changes in CMAP amplitudes for the left median and ulnar nerves during May 2002–October 2005. Despite the low amplitude CMAPs on distal nerve stimulation that were observed when the patient was clinically severely deteriorated (eg, May 2002 and September 2004), electromyography showed only slight denervation activity indicative of axonal damage.
Figure 1. Compound motor action potential (CMAP) amplitudes on stimulation of the left median (•) and ulnar (o) nerves at the wrist.
Lower normal limits for CMAP amplitudes are indicated by the solid (median) and broken (ulnar) horizontal lines. Arrows indicate dates for the combined treatment with cyclophosphamide and blood stem cell transplantation.
DISCUSSION
This is the first report of repeated treatment with high dose cyclophosphamide and ASCT in a patient with CIDP. Our patient stopped responding to IVIG, did not respond to corticosteroids and azathioprine, and had a very short lasting benefit from plasmapheresis. He may have responded to other drugs such as ciclosporin or mycophenolate mofetil, but we considered further attempts with long term medication and repeated laboratory controls to be more difficult for the patient than ASCT. In our hospital the treatment related mortality in ASCT is less than 1% (unpublished and excluding patients with amyloidosis). This experience corroborates well with results from a recent multicentre study on patients with severe rheumatoid arthritis.4 In the lack of controlled trials with ASCT in CIDP and because most patients respond well to standard immunomodulating treatment with IVIG or corticosteroids without serious side effects, we do not recommend routine use of high dose cyclophosphamide and ASCT. In refractory patients, however, it may be a good alternative. Our case shows that the treatment, if necessary, can be repeated with a good result. It remains, however, to be seen whether we have cured the patient or whether we have only induced another long lasting remission (3 years as of October 2007).
LEARNING POINTS
Chronic inflammatory demyelinating polyneuropathy (CIDP) is characterised by the occurrence of symmetrical weakness and sensory impairment in arms and legs. CIDP has either a relapsing or chronic progressive course.
CIDP is considered to be an autoimmune disease,
Remission from treatment resistant CIDP may be possible after treatment with cyclophosphamide and autologous stem cell transplantation, which may be repeated.
Acknowledgments
This article has been adapted with permission from Axelson HW, Öberg G, Askmark H. Successful repeated treatment with high dose cyclophosphamide and autologous blood stem cell transplantation in CIDP. J Neurol Neurosurg Psychiatry 2008;79:612–14.
Footnotes
Competing interests: None.
REFERENCES
- 1.Köller H, Kieseier BC, Jander S, et al. Chronic inflammatory demyelinating polyneuropathy. N Engl J Med 2005; 352: 1343–56 [DOI] [PubMed] [Google Scholar]
- 2.Brannagan TH, Pradham A, Heiman-Patterson T, et al. High-dose cyclophosphamide without stem-cell rescue for refractory CIDP. Neurology 2002; 58: 1856–8 [DOI] [PubMed] [Google Scholar]
- 3.Vermeulen M, Van Oers MH. Successful autologous stem cell transplantation in a patient with chronic inflammatory demyelinating polyneuropathy. J Neurol Neurosurg Psychiatry 2002; 72: 127–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snowden JA, Passweg J, Moore JJ, et al. Autologous hemopoietic stem cell transplantation in severe rheumatoid arthritis: a report from the EBMT and ABMTR. J Rheumatol 2004; 31: 482–8 [PubMed] [Google Scholar]