Abstract
This Classic Article is a reprint of the original work by John Caffey, Multiple Fractures in the Long Bones of Infants Suffering from Chronic Subdural Hematoma. An accompanying biographical sketch of John Caffey is available at DOI 10.1007/s11999-010-1665-1. The Classic Article is ©1946, and is reprinted with permission of the American Journal of Roentgenology from Caffey J. Multiple fractures in the long bones of infants suffering from chronic subdural hematoma. Radiology. 1946;194:163–173.
Fractures of the cranium are not infrequently associated with infantile subdural hematoma but fractures in the long bones have rarely been reported as complications of this intracranial lesion. An old fracture of the radius is mentioned by Sherwood [1] in his fifth case, Ingraham and Heyl [2] demonstrated greenstick fractures roentgenographically in the radiuses and ulnas of both forearms of one infant (Case 4) in whom there were neither clinical signs of fracture nor history of injury, Dr. Ingraham has written me that in his extensive experience with more than 100 cases of infantile subdural hematoma, fractures were also found in the humerus of one patient; in the femur of another; and in six ribs of a third [3].
For many years we have been puzzled by the roentgen disclosure of fresh, healing and healed multiple fractures in the long bones of infants whose principal disease was chronic subdural hematoma. The subject of this paper is the description of 6 such patients who exhibited 23 fractures and 4 contusions of the long bones. In not a single case was there a history of injury to which the skeletal lesions could reasonably be attributed and in no case was there clinical or roentgen evidence of generalized or localized skeletal disease which would predispose to pathological fractures.
Comment
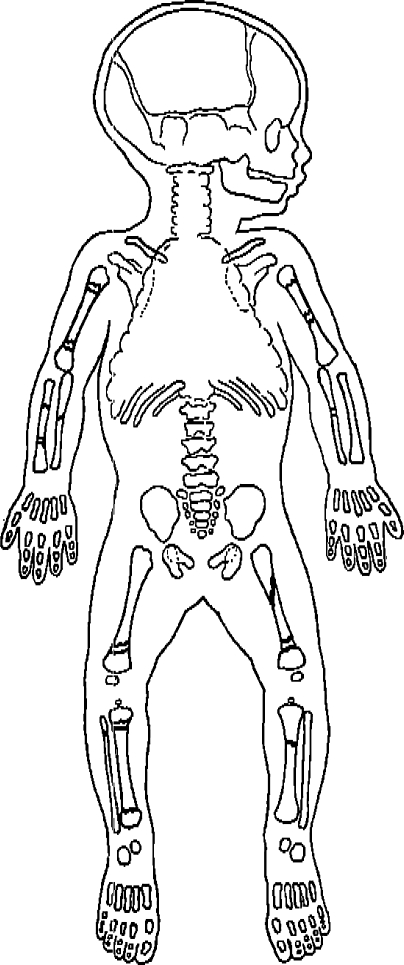
The skeletal changes are summarized in Table 1 and their distribution is depicted schematically in Fig. 7. In the aggregate all of the large bones in the upper and lower extremities were fractured but the small bones of the hands, feet, wrists and ankles were not affected. The epiphyseal ossification centers were all intact and fractures were not found in the cranium or in the flat bones of the pelvis and shoulder girdle.
Table 1.
Summary of important data in six cases
| Case number | Bones affected | Total lesions | Fractures | Contusions | Location fracture | Following subdural hematoma | History trauma | Remarks | |
|---|---|---|---|---|---|---|---|---|---|
| Metaphyseal | Diaphyseal | ||||||||
| I | Radius Ulna Femur |
3 | 3 | 0 | 0 | 3 | 1 | 0 | Fracture of radius during hospital residence without recognized injury |
| II | Femur Humerus (2) Ulna (2) |
5 | 4 | 1 | 2 | 2 | 5 | 0 | Skeleton normal roentgenographically at onset of subdural hematoma |
| III | Femurs (2) Tibia (2) Fibulas |
5 | 5 | 0 | 5 | 0 | 5 | 0 | All fractures located in opposing bones at knee joint |
| IV | Humerus (2) Tibia (2) |
4 | 3 | 1 | 3 | 0 | 4 | 0 | Clinical signs of fracture appeared II months after first convulsion |
| V | Femur Tibia Radius Ulna |
4 | 4 | 0 | 1 | 3 | 2 | 0 | Fractures of radius and ulna probably neonatal fracture of humerus and femur occurred at 7 months of age |
| VI | Humerus (2) Tibia (2) Femur |
6 | 4 | 2 | 3 | 1 | 0 | 0 | Cesarean section; first convulsion in section week of life |
| Total | 26 | 27 | 23 | 4 | 14 | 9 | 17 | 0 | |
Fig. 7.
Spot map of the skeleton showing the distribution of the 23 fractures in 6 patients.
Save for the fractures, the entire skeletons of all patients appeared to be healthy; this was true of the fractured as well as the unfractured bones. There was neither clinical nor roentgen evidence to support the idea that pre-existing systemic or localized skeletal disease weakened the bones and made them unusually vulnerable to trauma.
The large cortical thickenings associated with several of the fractures (see Figs. 2B and 3B) are similar to the cortical thickenings which develop in many cases of scurvy following subperiosteal hemorrhage. The other roentgen signs which characterize active scurvy are, however, conspicuously absent in these cases-changes in the metaphyses, spongiosa, corticalis and epiphyseal ossification centers. Moreover 5 patients (except Case 1) appeared to have taken adequate vitamin C at the time fractures were found and none of them exhibited the clinical manifestations of active scurvy. During the first years of life when the periosteum is normally loosely attached to the underlying corticalis and is normally richly supplied with blood vessels, large subperiosteal hemorrhages commonly develop at the sites of traumatic fractures in nonscorbutic infants (Fig. 8). Two other features make the scorbutic origin of the fractures highly improbable, Nine of the fractures were located deep in the shafts (see ulna, Case I; femur, Case II; femur, Case v; tibia Case vi); scorbutic fractures in contrast develop characteristically in the metaphyses near the cartilage-shaft junctions. Furthermore angular deformities of the fractured bones persisted after healing in several bones (see femur, Case I; femur, Case II; humerus, Case IV; radius and ulna, Case V). Scorbutic fractures in our experience heal without residual angular deformities, Although scurvy has been described in a few cases of infantile subdural hematoma [4, 5], there is no convincing clinical or roentgen evidence that the patients in this group suffered from vitamin C deficiency.
Fig. 8.

Traumatic cortical thickening of the radius and ulna following an injury to an infant four and one-half months of age who had neither subdural hematoma nor scurvy. Orange juice had been taken in daily dosages of 2 ounces since the first weeks of life. In the original history the mother stated that the infant’s forearm had suddenly become swollen one month before without precedent injury. After the demonstration of the roentgen findings she admitted that a few hours before the onset of the swelling of the forearm, the baby had rolled off a table and she had grabbed him by the left forearm and jerked him into the air to prevent his fall to the floor.
When cortical thickenings were demonstrated in the absence of visible fractures, the lesions have been classified as periosteal contusions (see left humerus, Case iv and both humeri, Case v). Trauma to the periosteal blood vessels may cause subperiosteal hemorrhage, elevation of the periosteum, and local cortical thickening in nonscorbutic infants (see Fig. 8). The causal mechanism is similar to that of traumatic ossifying periostitis of the newly born [6]. It is also possible that fractures were actually present in the sites of the cortical thickenings but were invisible roentgeno-graphically, Such was undoubtedly the case in the femur of our second patient. In an early roentgenogram (Fig. 2B) a large subperiosteal swelling was visible but there was no evidence of a fracture line; six months later however (Fig. 2C), at the same site a healed complete fracture, overriding of the fragments and massive callus were all evident.
The traumatic theory of the causation of subdural hematoma has been accepted almost to the exclusion of all other causes [7] despite the fact that a history of injury is lacking in almost one-half of the cases [8]. The negative history of trauma in so many cases can probably be best explained by assuming that sometimes lay observers do not properly evaluate ordinary but causally significant accidents especially falls on the head, and that other important traumatic episodes pass unnoticed or are forgotten by the time delayed cranial symptoms appear. Putman and Cushing [9] have pointed out that weeks or months may elapse between the original cephalic injury and the onset of the clinical signs of subdural hematoma. Also recognized injuries may be denied by mothers and nurses because injury to an infant implies negligence on the part of its caretaker.
The absence of history of trauma to the fractured bones cannot be explained in the same way. The injuries which caused the fractures in the long bones of these patients were either not observed or were denied when observed. The motive for denial has not been established. The clinical signs of fractures in the long bones usually appear immediately after injury and the causal relationship between the traumatic force and damage to the bone is clear. It is unlikely that trivial unrecognizable trauma caused the complete fractures in the femurs in Cases I, II and V; in the humerus in Case IV; and in the radius in Case I. Moreover in several cases ecchymoses were found near the sites of the fractures. There was a striking similarity in the course of events in Case II and Case III. In each case unexplained fresh fractures appeared shortly after the patient had arrived home after discharge from the hospital. In one of these cases the infant was clearly unwanted by both parents and this raised the question of intentional ill-treatment of the infant; the evidence was inadequate to prove or disprove this point. In Case I a fresh complete fracture of the radius with ecchymoses in the neighboring soft tissues developed after a continuous residence of nine days in the hospital and, notwithstanding, injury was not observed or at least not admitted by the hospital attendants.
It is possible that some of the fractures in the long bones were caused by the same traumatic forces which were presumably responsible for the subdural hematomas. However, this was not the case in the majority of the fractures because 17 fresh fractures appeared many weeks and months after the first clinical manifestations of subdural hematoma and after the withdrawal of bloody fluid from the subdural space. In one patient (Case iv) fractures in the long bones developed six months after the subdural tumor had been removed surgically.
We have also considered the possibility that the long bones were injured and fractured during convulsive seizures. There is little evidence to support such a postulate. In not a single case did fresh fractures appear immediately following the convulsive seizure and complete fractures occurred in patients who had only mild convulsions. It has been demonstrated that the vertebral bodies of children may be fractured during the convulsive seizures of tetanus [10] but in these circumstances there were no associated fractures in the extremities. To our knowledge, fractures of convulsive origin in the long bones have never been demonstrated in the common severe convulsive diseases of infancy and childhood such as lead poisoning, meningitis, cerebral neoplasm and hypocalcemic tetany.
Summary
Six infants with chronic subdural hematoma and associated multiple fractures in the long bones are described.
History of injury to the long bones as well as to the head was lacking in all cases.
There was no roentgen or clinical evidence of general or localized skeletal disease which would have predisposed the bones to pathological fractures.
The majority of the fractures developed after the onset of the subdural hematomas.
Conclusions
Fractures of the long bones are a common complication of infantile subdural hematoma.
The fractures appear to be of traumatic origin but the traumatic episodes and the causal mechanism remain obscure.
The presence of unexplained fractures in the long bones warrants investigation for subdural hematoma.
Routine roentgen examination of the long bones in subdural hematoma is necessary for the identification of fractures because many of them are silent clinically.
Footnotes
Richard A. Brand MD (✉) Clinical Orthopaedics and Related Research, 1600 Spruce Street, Philadelphia, PA 19103, USA e-mail: dick.brand@clinorthop.org
References
- 1.Sherwood D. Chronic subdural hematoma in infants. Am. J. Dis. Child. 1930;39:980. [Google Scholar]
- 2.Ingraham FD, Hey HL. Subdural hematoma in infancy and childhood. J. Am. M. Ass. 1939;112:198–204. [Google Scholar]
- 3.Ingraham, F. D. Personal communication, May 7, 1945.
- 4.Gilman BB, Tanzer RC. Subdural hematoma in infantile scurvy. J. Am. M. Ass. 1932;99:989–991. [Google Scholar]
- 5.Ingalls TH. The role of scurvy in the etiology of chronic subdural hematoma. New England J. Med. 1936;215:1279–1281. doi: 10.1056/NEJM193612312152704. [DOI] [Google Scholar]
- 6.Snedecor S, Knapp R,ET, Wilson HB. Traumatic ossifying periostitis of the newborn. Surg. Gynec. & Obst. 1935;61:385–387. [Google Scholar]
- 7.Groff RA, Grant FC. Chronic subdural hematoma; collective review. Internal. Abstr. Surg. 1942;74:9–20. [Google Scholar]
- 8.Ingraham FD, Matson DD. Subdural hematoma in infancy. J. Pediat. 1945;24:1. doi: 10.1016/S0022-3476(44)80138-X. [DOI] [Google Scholar]
- 9.Putnam TJ, Cushing H. Chronic subdural hematoma. Arch. Surg. 1925;11:329–393. [Google Scholar]
- 10.Dietrich HF, Karshner RG, Stewart SF. Tetanus and lesiona of the spine in childhood. J. Bone & Joint Surg. 1940;22:43–54. [Google Scholar]