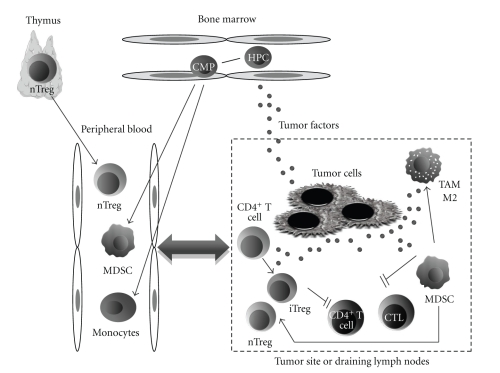
Figure 1.
Schematic representation of the potential role of the immune suppressive cells (ISCs) in cancer. The release into the circulation of ISCs derived from thymus (nTregs) or from bone marrow (MDSCs) is partially driven by factors secreted by the tumor. Successively, ISCs can migrate into the tumor site (or a draining lymph node). Moreover, several factors produced in the tumor microenvironment may induce the conversion of CD4+ T cells into iTregs or drive the polarization of monocytes towards a M2-phenotype. All these phenomena lead to an inhibition of CD4+ T-helper cells and cytotoxic T lymphocytes (effector cells), resulting in a general decrease of the antitumor immune response. Theoretically, the release of ISCs from the thymus, the bone marrow, and the tumor site to the peripheral blood could reflect the immunosuppressive status of the antitumor immune response and could be of use in the real time immune monitoring of patients enrolled in therapeutic vaccine clinical trials. HPC: hematopoietic progenitor cells; CMP: committed myeloid progenitors; nTreg: thymic-derived, naturally occurring regulatory T cells; iTreg: induced or adaptive regulatory T cells; MDSC: myeloid-derived suppressor cells; TAM-M2: tumor-associated macrophages characterized by M2-polarization; CTL: cytotoxic T lymphocytes.