Therapeutic paracentesis is a common procedure for patients with ascites and is commonly done without image guidance. The preferred site by many physicians is the right or left lower quadrant. Rarely, hemorrhage may occur due to inadvertent injury to a branch of the inferior epigastric artery.
CASE REPORT
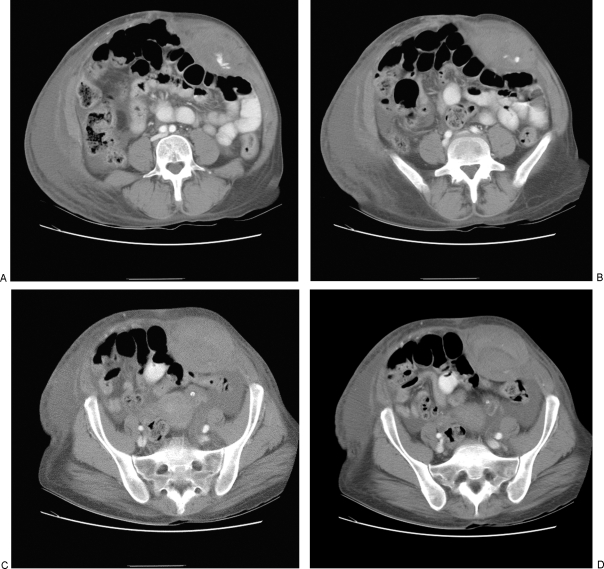
A 44-year-old African American woman with human immunodeficiency virus (HIV), hepatitis C infection, and a history of alcohol abuse presented to our emergency department with left lower quadrant swelling. She had undergone paracentesis (4.5 L) 2 days earlier after a large volume of fluid was noted on ultrasound examination (Fig. 1). One day after the procedure, she was seen in the emergency department and described a constant pressure across the abdomen with worsening pain during movement. Her hemoglobin was noted to have fallen from 14.8 to 10.5 mg/dL. She was referred for urgent computed tomography (CT) examination (Fig. 2), which demonstrated a large rectus sheath hematoma with active bleeding.
Figure 1.
Left lower quadrant ultrasound shows large amount of ascites.
Figure 2.
Abdominal computed tomography performed after paracentesis. (A, B) Axial image shows left rectus sheath hematoma with active extravasation. (C) Axial image lower in the pelvis shows maximal diameter of hematoma. (D) Axial image at level of sacrum shows hematoma extending through the lower pelvis.
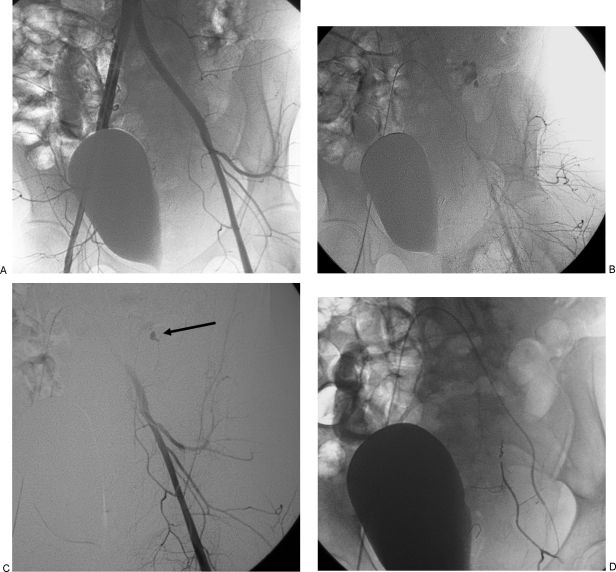
The patient remained hemodynamically stable and was brought directly from the CT scanner to the IR suite. The right common femoral artery was catheterized, and a 5F sheath was inserted. A pelvic arteriogram (Fig. 3A) was performed but failed to show active bleeding. Selective catheterization of the left common iliac artery was then performed and angiography was repeated. The second angiogram (Fig. 3B, C) showed active bleeding from the inferior epigastric artery. The artery was selectively catheterized using a microcatheter (Renegade STC, Boston Scientific, Natick, MA), and multiple 4-mm microcoils were deployed until stasis was observed in the artery (Fig. 3D).
Figure 3.
Angiogram with embolization of left inferior epigastric artery. (A) Pelvic arteriogram shows normal appearing arteries without evidence of active extravasation. Note the bladder deviated to the left. (B) Arterial phase of a selective left common iliac angiogram shows active bleeding from the inferior epigastric artery. (C) Digital subtraction left common iliac angiogram shows bleeding site (arrow). (D) Inferior epigastric angiogram after coil embolization shows complete occlusion of vessel.
She was transferred to the intensive care unit and received 4 units of packed red blood cells and 2 units of fresh frozen plasma with complete stabilization of her hemoglobin. Abdominal pain slowly improved and the patient made an uneventful recovery.
DISCUSSION
Abdominal paracentesis is a very safe procedure with a major bleeding complication rate of less than 1%. In fact, in many institutions, preprocedure coagulation tests are regarded as unnecessary. Nonetheless, similar to any invasive procedure, untoward bleeding can occur and an arterial injury of the inferior epigastric artery may be a lethal complication.
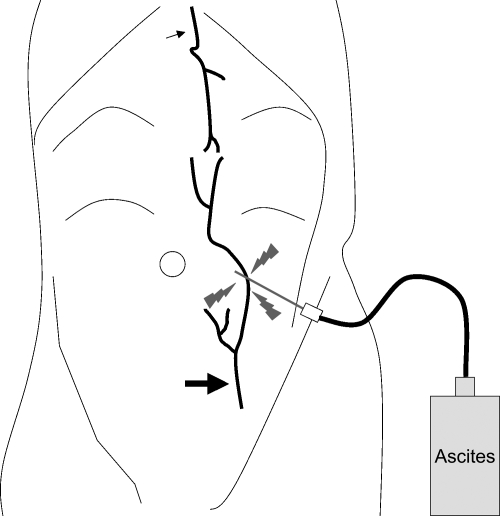
The lower two thirds of the rectus sheath derive its arterial supply from the inferior epigastric artery. This artery is located on the dorsal surface of the muscle and is separated from the abdominal cavity by the peritoneum. Perforating branches of the inferior epigastric artery dive into the muscle. Significant rectus sheath hematomas may be caused by paracentesis (Fig. 4) or, more commonly, occur spontaneously in patients who are anticoagulated. In some cases, a pseudoaneurysm of the inferior epigastric artery may be found. Embolization may be used to successfully treat abdominal wall hematomas; however, its role remains poorly defined due to the lack large reported series in the medical literature.
Figure 4.
Illustration of injury to inferior epigastric artery during paracentesis.
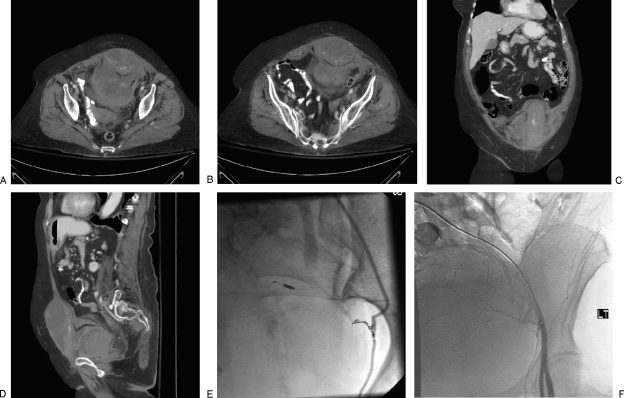
Spontaneous bleeding into the rectus sheath is often thought to be diffuse and microvascular in etiology; therefore, many of these patients are not referred for urgent embolization. Conservative therapy usually successfully controls bleeding in all but a minority of patients. In patients who exhibit continued bleeding or in whom the hematoma ruptures into the prevesical space (Fig. 5), embolization can be a valuable therapy. However, in the two reported series by Rimola et al (19 patients) and Sobkin et al (20 patients), 25% and 30%, respectively, of the patients died even after successful embolization. When a rectus sheath hematoma ruptures into the prevesical space, it does so below the arcuate line, which is ~5 cm below the umbilicus. Above the arcuate line, the aponeuroses of the oblique muscles and transversalis muscle invest the rectus muscle both anteriorly and posteriorly. This usually helps to contain hemorrhage. Below the arcuate line, the aponeuroses remain intact anteriorly but not posteriorly; this relatively weak point is the most common site of rupture into the extraperitoneal space.
Figure 5.
Spontaneous rectus sheath hemorrhage in an anticoagulated patient. (A, B) Axial enhanced computed tomography (CT) images show large rectus sheath hematoma ruptured into the prevesical space with active bleeding. (C) Coronal reformatted CT image shows bleeding site in left rectus muscle. (D) Sagittal reformatted CT image shows extent of hemorrhage in prevesical space. (E) Angiogram of left inferior epigastric artery shows vasospasm of the artery. (F) Angiogram after embolization shows complete occlusion of the artery.
As a general rule, the common femoral artery opposite to the site of bleeding is punctured, and a curved 4 or 5F catheter such as a Rosch-Inferior Mesenteric or Cobra-2 (Cook, Bloomington, IN) is used to catheterize the orifice of the contralateral inferior epigastric artery. A microcatheter may then be used for superselective embolization. A variety of agents have been used for occlusion. I favor microcoils because they are easy to see and deploy accurately and tend to control bleeding in most cases. In some patients, it may be necessary to perform both a proximal and distal embolization (i.e., “front-door and back-door”) because there is a rich collateral supply to the muscle, with the upper one third being supplied from the superior epigastric artery from the internal mammary artery.
SUGGESTED READINGS
- Mulpuru S K, Mori N A, Levey R L, Leonardo R. Life-threatening hematoma associated with paracentesis: a case report. Blood Coagul Fibrinolysis. 2006;17:491–493. doi: 10.1097/01.mbc.0000240924.95801.91. [DOI] [PubMed] [Google Scholar]
- Levy J M, Gordon H W, Pitha N R, Nykamp P W. Gelfoam embolization for control of bleeding from a rectus sheath hematoma. AJR Am J Roentgenol. 1980;135:1283–1284. doi: 10.2214/ajr.135.6.1283. [DOI] [PubMed] [Google Scholar]
- Rimola J, Perendreu J, Falcó J, Fortuño J R, Massuet A, Branera J. Percutaneous arterial embolization in the management of rectus sheath hematoma. AJR Am J Roentgenol. 2007;188:497–502. doi: 10.2214/AJR.06.0861. [DOI] [PubMed] [Google Scholar]
- Sharafuddin M J, Andresen K J, Sun S, Lang E, Stecker M S, Wibbenmeyer L A. Spontaenous extraperitoneal hemorrhage with hemodynamic collapse in patients undergoing anticoagulation: management with selective arterial embolization. J Vasc Interv Radiol. 2001;12:1231–1234. doi: 10.1016/s1051-0443(07)61686-8. [DOI] [PubMed] [Google Scholar]
- Sobkin P R, Bloom A I, Wilson M W, et al. Massive abdominal wall hemorrhage from injury to the inferior epigastric artery: a retrospective review. J Vasc Interv Radiol. 2008;19:327–332. doi: 10.1016/j.jvir.2007.11.004. [DOI] [PubMed] [Google Scholar]