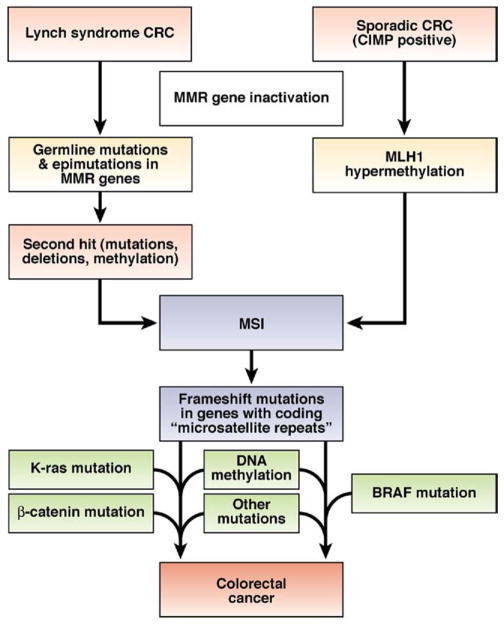
Figure 5.
There are 2 molecular pathways to the development of CRC with MSI. Approximately 20%–25% of colorectal tumors with MSI arise in individuals with Lynch syndrome. These tumors contain a germline mutation in one of the MMR genes, followed by a second hit to the wild-type copy (inherited from the unaffected parent); this could occur via LOH, methylation, or point mutation. Defects in MMR result in MSI and rapid accumulation of somatic mutations. It has been proposed that tumors arise via mutations in a few critical genes, but that large numbers of microsatellite mutations also occur—most of which are simply passengers that provide the mutational signature used to identify tumors with MSI. Colorectal tumors that arise in patients with Lynch syndrome often have mutations in KRAS. Most cases of CRC associated with MSI are not inherited (familial), but arise through sporadic methylation-induced silencing of MLH1. These sporadic tumors have the CIMP signature, resulting in methylation of many gene promoters. When the MLH1 promoter is methylated, MMR activity fails and MSI ensues. Thus, the mutational signature of sporadic tumors includes CIMP and MSI. BRAF mutations are also observed in most sporadic colorectal tumors, but do not occur in tumors of patients with Lynch syndrome.