Abstract
Background
Investigating modifiable factors that contribute to functional limitations in patients with total knee arthroplasty (TKA) may guide changes in rehabilitation protocols and improve functional outcomes. Whereas quadriceps muscle weakness has been demonstrated to contribute to functional limitations in TKA, the role of hip abductor weakness has not received attention.
Objective
The purpose of this study was to determine whether hip abductor strength (force-generating capacity) contributes to physical function beyond what can be explained by quadriceps muscle strength in patients after a TKA.
Design
A cross-sectional design was used in the study.
Setting
The study was conducted in a clinical laboratory at an academic center.
Patients
Thirty-one people with TKA (74% female; mean age=68 years, SD=8; mean body mass index=31 kg/m2, SD=5) participated in the study.
Measurements
Strength of quadriceps muscles and hip abductors was measured using an isokinetic dynamometer. Performance-based physical function was assessed with 4 measures: self-selected walking speed, the Figure-of-8 Walk Test, the Stair Ascend/Descend Test, and the 5-Chair Rise Test. Self-reported physical function was assessed with the Western Ontario and McMaster Universities Osteoarthritis Index Physical Function Subscale.
Results
In hierarchical regression models, after accounting for demographic and anthropometric factors, quadriceps muscle strength was associated with performance on the Stair Ascend/Descend Test. After accounting for demographic, anthropometric, and quadriceps strength, hip abductor strength was associated with performance on the Stair Ascend/Descend Test, the Figure-of-8 Walk Test, and the 5-Chair Rise Test.
Limitations
The study design precluded ascertainment of causal relationships.
Conclusions
After TKA, hip abductor strength influenced physical function in participants more than did demographic or anthropometric measures or quadriceps strength. Longitudinal studies with larger samples are warranted. If findings are replicated, they will justify targeting the hip abductors during rehabilitation after TKA.
Although there is a rapid and substantial reduction of knee pain after total knee arthroplasty (TKA), 37% of patients have limited functional improvement 1 year after the surgery.1 The most common limitations of these patients are diminished walking speed, difficulty in ascending and descending stairs, and inability to return to sports played prior to the surgery.2–4 Investigating modifiable factors that contribute to the functional limitations in patients with TKA may help guide rehabilitation protocols and improve functional outcomes.
One such modifiable factor is lower-extremity muscle weakness. The weakness of the quadriceps muscles has received a good amount of research attention, and several studies have tested its contribution to functional limitations after TKA.4–7 The quadriceps muscles control knee flexion during ambulation. Adequate knee-extensor strength (force-generating capacity) is needed for eccentric control of knee flexion, that is, to control the knee-flexion demand moment in the sagittal plane.8 Studies have shown significant deficits in quadriceps muscle strength after TKA that remain unresolved for years after the surgery.4,5 Moreover, quadriceps muscle weakness after TKA has been associated with decreased ability to walk and climb stairs5,6,9,10 and with asymmetrical gait patterns.11,12 Recent evidence also has shown that a progressive strengthening program mainly targeting the quadriceps muscles resulted in significant functional recovery 3 and 12 months after TKA.13 Combined, these studies support the role of quadriceps muscle strength in physical function after TKA. However, quadriceps muscle strength is only necessary for the function and control of knee extensors and, to some degree, of hip flexors (by the action of the rectus femoris muscle). The lack of strength of other lower-extremity muscles also may contribute to the functional limitations of these patients.
Hip abductor strength may contribute to lower-extremity function in patients who have had TKA. The hip abductors are known to stabilize the trunk and hip during ambulation, control limb alignment, and transfer forces from the lower extremities to the pelvis.14 In the frontal plane, hip abduction strength is required for hip stability, that is, to control the hip adduction demand moment.8 Studies have suggested that hip abductor weakness plays a role in functional limitations in older adults. One study demonstrated that hip abductor weakness was associated with poorer physical performance,15 and another study showed that hip abduction weakness was a predictor of future falls in community-dwelling older adults.16 The results of these studies raise the question of whether the role of hip abductors in functional ability and performance may have been overlooked in patients who have undergone TKA. Because the strength of the quadriceps muscles and the strength of hip abductor muscles represent distinct aspects of lower-extremity muscle performance, the purpose of this study was to determine whether hip abductor strength contributes to physical function beyond what can be explained by quadriceps muscle strength. To our knowledge, this aim has not been pursued previously. If it is demonstrated that hip abductor strength contributes to function more than does quadriceps strength, these results will serve as the first step to justify strengthening of the hip abductors during rehabilitation after TKA, and to foster this line of research.
Method
Design Overview
Data for this cross-sectional study were obtained from the baseline assessment of a pilot randomized trial that investigated the efficacy of balance training on lower-extremity performance in individuals with TKA.17
Setting and Participants
Forty-three people participated in the randomized trial. This ancillary study was planned after the parent trial had started. As a result, the first 12 enrolled participants were not included because of the lack of hip abductor strength measures, resulting in inclusion of only 31 participants in this study. Data collection for this study took place from January to November 2007 in the Department of Physical Therapy at the University of Pittsburgh. Participants were recruited from one orthopedic surgeon. Participants who had had a TKA performed in the previous 2 to 6 months were mailed study information. Interested participants were screened over the telephone for eligibility. Participants signed a consent form approved by the University of Pittsburgh Institutional Review Board.
Inclusion criteria required participants to have had unilateral TKA surgery between 2 and 6 months previously and to be 50 years of age or older. Individuals were excluded if they reported having had 2 or more falls within the past year, were unable to independently ambulate a distance of 30.5 m (100 ft), had acute illness or cardiovascular disease, had severe visual impairment, had had a lower-extremity amputation, or had a progressive neurological disorder.
Measurements
Each participant completed demographic and self-report questionnaires of function followed by performance-based measures of function and measures of quadriceps muscle and hip abduction strength. Measurements were performed during one testing session. We were interested in measures of muscle strength on the operated leg to capture weakness secondary to the TKA procedure and recovery.
Muscle strength was measured as torque in newton-meters using an isokinetic dynamometer (Biodex System 3 Pro*). Gravity correction was performed during strength tests. All tests of muscle strength were performed isometrically. Participants performed 3 warm-up contractions with the muscle group being tested using ∼50%, 75%, and 100% of their maximum perceived effort. After a brief rest, each participant was given strong verbal encouragement to produce the maximal voluntary isometric contraction (MVIC). Three MVIC trials were performed during testing of each muscle group. Each MVIC was held for ≈5 seconds.
For quadriceps muscle strength, the participant was seated on the Biodex with the tested knee flexed at 70 degrees. The axis of rotation of the dynamometer was aligned with the lateral femoral epicondyle. The force-sensing arm was secured to the ankle. A thigh strap, a waist strap, and 2 chest straps were secured to stabilize the participant in the dynamometer chair. This procedure has been shown to yield reliable quadriceps femoris muscle torque measurements in our laboratory. The intraclass correlation coefficient (ICC [2,1]) was .96.
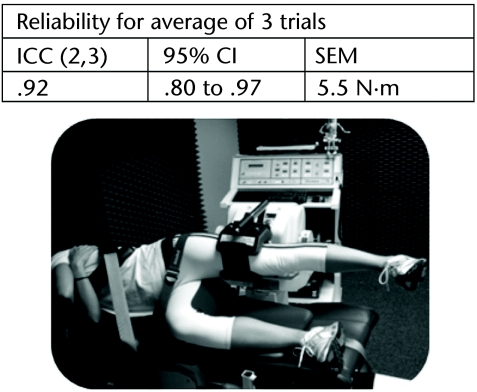
To test hip abductor strength, participants lay on their side (facing away from the dynamometer force sensor) with the tested hip superior to the opposite hip. The knee of the tested leg was extended, and the opposite knee was bent at 90 degrees. The axis of the dynamometer was aligned perpendicular to the hip frontal plane of motion at the level of the superior-posterior border of the greater trochanter. The tested hip was positioned at 0 degrees of hip abduction and neutral rotation. The pad of the dynamometer force-sensing arm was secured just above the lateral knee joint line, proximal to the lateral epicondyle, to prevent imposed adduction moment on the knee. The torso and pelvis were stabilized with Velcro straps† to avoid body rotation. The top hand grasped the border of the chair. Participant setup during this test is shown in the Figure. Intertester reliability of measurements of hip abduction strength was determined during this study. For this purpose, measures of hip abduction strength were repeated on a subset of 21 participants who agreed to being tested a second time. The second measurement session took place 3 to 8 days after the first session, and each session was conducted by an independent tester. Testers were masked to each other's results. We determined reliability using ICC analysis. We calculated the ICC for the average of the 3 trials. Results of the reliability analysis are shown in the Figure.
Figure.
Setup for hip abduction strength measure. ICC (2,3)=intraclass correlation coefficient with 2 raters and the average of 3 measurements, 95% CI=95% confidence interval, SEM=standard error of the measurement. SEM calculated using the formula (SD ×√1−r), where r is the reliability coefficient and SD is the standard deviation of measurements of tester 1 and tester 2.
For performance-based measures, we chose a battery of tests easily done in the clinical setting. Because patients with TKA have limited ability during walking, managing steps, and squatting,3,18 we included performance tasks that encompass these abilities. The battery of tests included 4 timed measures: (1) self-selected walking speed, (2) the Figure-of-8 Walk Test (walk curved and straight paths), (3) the Stair Ascend/Descend Test, and (4) the 5-Chair Rise Test. Walking speed was measured in the self-selected condition (as participants would normally walk) using the GAITRite System.‡ The 5-m instrumented carpet was located in the central part of a 9-m path to avoid including acceleration and deceleration in the measures. The Figure-of-8 Walk Test consisted of timing participants walking a path around 2 cones placed 1.5 m (5 ft) apart. Participants stood in the middle of the 2 cones and then walked 1 continuous figure-of-8 pattern around the cones, ending at the same location from which they began. In the Stair Ascend/Descend Test, participants were timed while climbing up and coming down an isolated set of 11 steps (depth=30 cm, height=17 cm) using a handrail at the preferred side. During the 5-Chair Rise Test, participants were timed while rising from a chair 5 times without using arm support. During the last 3 tests, participants were instructed to complete the tasks as quickly and safely as possible. The 2 walking tests measure regular and skilled walking ability, respectively, whereas the Stair Ascend/Descend Test measures ability to manage steps, and the 5-Chair Rise Test measures ability to change from sitting to standing positions repeatedly. These tests have been shown to be reliable and responsive and have the ability to discriminate from low to high functional ability in individuals at various ages and functional levels.19–24
Self-reported physical function was measured with the Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale (WOMAC-PF).25 The WOMAC-PF has 17 items (each scored from 0 to 4), with a total score of up to 68 points. Higher scores indicate worse function. Validity of data obtained with the WOMAC has been well established.25
Data Analysis
As the distributions of self-selected walking speed, Figure-of-8 Walk Test, Stair Ascend/Descend Test, and 5-Chair Rise Test measurements were positively skewed, the scores were either squared or log-transformed before analysis so that they met the assumption of normality. First, Pearson (for continuous variables) or Spearman (for ordinal/categorical variables) correlations described the bivariate relationships between all variables. Then, we used hierarchical regression analysis to explore how quadriceps and hip muscle strength associate with physical function. Height and weight were decided a priori to be controlled in the regression analysis to account for the effect of body size on muscle strength measures. On the basis of previous literature or reported associations with physical function,5,26 additional potential covariates were sex, age, and time since surgery. These variables were only controlled in the regression models if the bivariate correlation indicated that they were at least moderately correlated (r=.30 or −.30) with both physical function and muscle strength.
In the hierarchical regressions, we hypothesized that quadriceps muscle strength would account for a significant amount of variance in self-reported and performance-based physical function over and above that accounted for by the covariates. We also predicted that hip abduction strength would account for a significant amount of variance in physical function over and above that accounted for by quadriceps muscle strength and the covariates. Separate hierarchical models were used for each of the 5 dependent variables (WOMAC-PF, Stair Ascend/Descend Test, Figure-of-8 Walk Test, 5-Chair Rise Test, and self-selected walk speed). Each model had 3 steps. In step 1, we entered the covariates. In step 2, we entered quadriceps muscle strength. In step 3, we entered hip abduction strength. Goodness of fit was evaluated by testing the residuals for normality and homoscedasticity. Because of the exploratory nature of this study, we did not correct alpha to account for multiple analyses, and P<.05 (2-tailed) was considered to be significant. We used PASW statistical software, version 17,§ for the statistical calculations.
Last, as we expected quadriceps muscle and hip abduction strength to be correlated, indicating that they can exert mutual influence in the hierarchical models, we used commonality analysis to partition the physical function variance.27 Commonality analysis decomposes the squared multiple correlation (R2) to determine both the unique and non-unique explained variance of the physical function variables by each predictor (strength of quadriceps muscle and strength of hip abductor muscles).28 The unique contribution of each predictor in a model is defined as the partition of variance attributed to it when entered last in a regression analysis.
Role of the Funding Source
This study was supported, in part, by the Claude D. Pepper Older American Independence Center (P30-AG024827); the Central Research Development Fund, University of Pittsburgh; the University of Pittsburgh Medical Center Health System Competitive Medical Research Fund; the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research (KL2 RR024154–02); and the American College of Rheumatology Research Education Foundation New Investigator Award. The funding sources played no role in the design, conduct, or reporting of the study. Contents of this publication are solely the responsibility of the authors and do not necessarily represent the official view of the funding sources.
Results
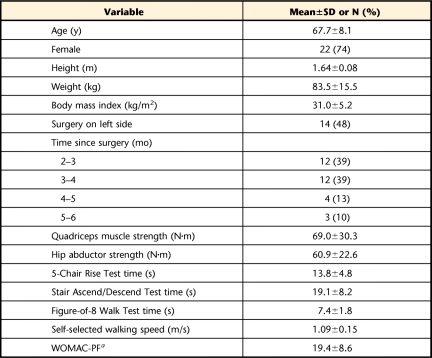
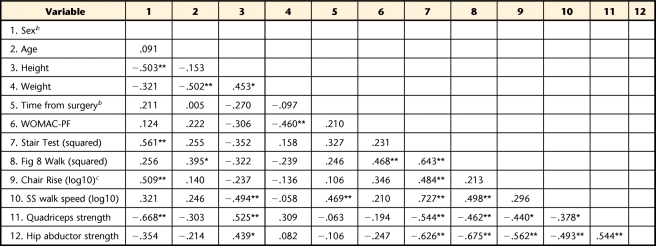
Table 1 summarizes the descriptive statistics of participants' characteristics, muscle strength, and physical function. The characteristics of participants enrolled in this study are similar to the demographic and functional characteristics reported in prior trials of patients with TKA.1,13,26 Table 2 provides the correlation coefficients among all variables. Three participants were unable to perform the 5-Chair Rise Test, and they were excluded from the analyses involving this variable. Quadriceps muscle and hip abduction strength had at least moderate correlation (smallest r value was −.38) with performance-based function. Quadriceps muscle and hip abduction strength had a small correlation with the WOMAC-PF (r=−.194 and −.247, respectively).
Table 1.
Participants' Descriptive Characteristics (N=31)
a WOMAC-PF=Western Ontario and McMaster Universities Osteoarthritis Index physical function subscale.
Table 2.
Correlation Matrix for Covariates, Physical Function, and Quadriceps and Hip Abductor Muscle Strength (N=31)a
WOMAC-PF=Western Ontario McMaster University Osteoarthritis Index physical function subscale, Stair Test=Stair Ascend/Descend Test, Fig 8 Walk=Figure-of-8 Walk Test, Chair Rise=5-Chair Rise Test, SS=self-selected. * P<.05, ** P<.01.
b Values are Spearman ρ.
c n=28.
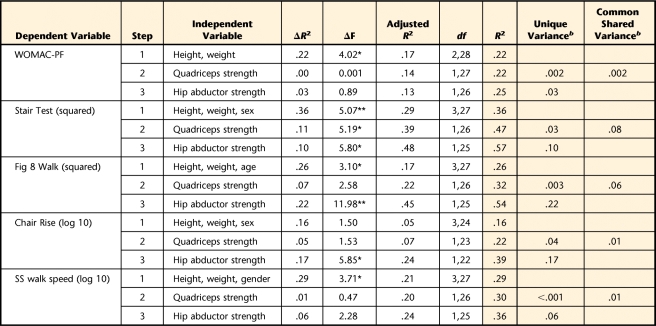
Table 3 shows the hierarchical models. In all of the models, the combination of height, weight, sex, and age explained between 16% and 36% of the variance on physical function. When the dependent variables were the WOMAC-PF or self-selected walking speed, the results indicated no significant additive effect for quadriceps muscle and hip abduction strength. When the Stair Ascend/Descend Test was the dependent variable, the additive effects of quadriceps muscle and hip abduction strength were significant. Quadriceps muscle strength explained an additional 11% of variance in physical function, whereas hip abduction strength explained 10% of variance in physical function above that of quadriceps muscle strength. For the Figure-of-8 Walk Test and 5-Chair Rise Test as dependent variables, we observed no effect for quadriceps muscle strength, but a significant additional effect for hip abduction strength. (Hip abduction strength explained 22% and 17% of variance on Figure-of-8 Walk Test and 5-Chair Rise Test, respectively.) The unique variance (Tab. 3, shaded area) explained by hip abduction strength ranged from 3% to 22%, which was at least threefold higher than the unique variance explained by quadriceps muscle strength (from 0.1% to 3%).
Table 3.
Hierarchical Regression Analysis for Muscle Strength Predicting Physical Functiona
WOMAC-PF=Western Ontario McMaster University Osteoarthritis Index physical function subscale, Stair Test=Stair Ascend/Descend Test, Fig 8 Walk=Figure-of-8 Walk Test, Chair Rise=5-Chair Rise Test, SS=self-selected. * P<.05, ** P<.01. The shaded area indicates the unique and common components of shared variance of quadriceps and hip abductor muscle strength on physical function.
b Equivalent to R2.
Discussion
The purpose of this study was to explore the cross-sectional associations between quadriceps muscle strength and hip abduction strength and physical function in patients with TKA. Although preliminary, the results suggest that hip abduction weakness may contribute to the functional limitations of patients with TKA over and above that of height, weight, age, sex, and quadriceps muscle strength. To the best of our knowledge, this is the first study to investigate these associations in the TKA population. In patients with osteoarthritis (OA) of the knee, the contribution of hip abduction has only been studied indirectly (as hip moments) in the context of how it affects knee joint loads. Chang et al29 investigated the association between hip abduction moments and medial tibiofemoral OA progression in 57 patients with knee OA. The results indicated that a greater hip abduction moment during gait protected against more severe medial OA progression. They further proposed a theory that hip abduction weakness could be a potential contributor to the increased load on the ipsilateral medial tibiofemoral compartment. Mündermann et al30 investigated the association between gait changes in knee OA and loads at the joints of the lower extremities. They reported that patients with more severe knee OA had increased peak knee adduction and decreased peak hip adduction compared with matched controls. They suggested that patients with severe knee OA lack hip abductor strength.
Our results are in agreement with previous research on aging. Brown et al15 investigated the association between several physical impairments and a battery of physical performance tests (PPT) in 107 elderly patients. They reported a significant association between PPT and hip abduction strength (r=.36). Results of their multiple stepwise regression indicated that hip abduction strength was one of the predictors of results of PPT and, when combined with 3 other variables (obstacle course performance, semi-tandem balance, and pegboard coordination), explained 73% of the PPT variance. Hilliard et al31 determined the capacity of measures of mediolateral protective stepping performance, hip abduction strength, and trunk mobility to predict the risk of falls in 51 community-living older people. They reported that people prone to falling demonstrated significantly lower hip abduction strength than people not prone to falling. Moreover, the 2-variable models that optimized the prediction of fall status included hip abduction strength. These studies help to support the findings of our study and the need for further research in this area.
The results of the correlations between physical function and quadriceps muscle strength agree with prior studies of patients with TKA. Mizner and Snyder-Mackler7 tested 14 patients with TKA 3 months after surgery and reported that quadriceps muscle strength of the involved leg correlated positively with the Six-Minute Walk Test (ρ=.64) and negatively with the Stair Ascend/Descend Test (ρ=−.65) and the Timed “Up & Go” Test (ρ=−.43). The same investigators reported extended results in 40 patients at 1, 2, 3, and 6 months after TKA.5 They reported significant correlations for the 4 time points between quadriceps muscle strength (involved side) and the Timed “Up & Go” Test (r=−.31 to −.44) and the Stair Ascend/Descend Test (r=−.33 to −.65). Common to these studies was that the associations were tested only in a bivariate fashion. Factors that may affect the associations, such as age, sex, height, and weight, have not been accounted for. In our study, when covariates were controlled, the contribution of quadriceps muscle strength to physical function was considerably tapered. Despite this tapering, however, care should be taken not to disregard the contribution of quadriceps muscle strength. The hierarchical models show that, although not always statistically significant, quadriceps muscle strength explained at least an additional 5% (ΔR2) of variance in the Stair Ascend/Descend Test, the Figure-of-8 Walk Test, and the 5-Chair Rise Test, which probably can be considered clinically significant. In addition, the common effects of quadriceps muscle and hip abductor strength on the Stair Ascend/Descend Test and the Figure-of-8 Walk Test seem clinically important. The common shared variances of the quadriceps muscle and hip abductors explained 8% of the Stair Ascend/Descend Test performance and 6% of the Figure-of-8 Walk Test performance (Tab. 3).
The fact that different approaches used to analyze the data yielded consistent results further supports the observation that hip abduction weakness may contribute to the functional limitations of patients with TKA more than that of quadriceps muscle strength alone. Bivariate correlations demonstrated that hip abduction strength had a higher correlation with measures of physical function than did quadriceps muscle strength. As a corollary, results of communality analysis demonstrated that the unique variance on physical function explained by hip abduction strength when quadriceps muscle strength was controlled for was higher than the unique variance explained by quadriceps muscle when the hip abduction strength was controlled for. This meant that the explanatory power of hip abduction strength on physical function was consistently higher than the explanatory power of quadriceps muscle strength. Finally, hierarchical regressions have shown that quadriceps muscle strength was associated with 1 performance-based measure over and above that of covariates and that hip abduction strength was associated with 3 performance-based measures over and above that of covariates and quadriceps muscle strength.
Several observations in our results warrant further discussion. First, the correlations between muscle strength and self-selected gait speed, although significant, were somewhat smaller than the correlations with the other performance tests, and, during the hierarchical regression, self-selected walking speed did not covary with muscle strength. We believe the reason for the small association between gait speed and muscle strength is that walking at a self-selected pace is not a demanding task. There is a procedural difference in the way self-selected gait speed and the other performance-based tests are performed. During the walking test, the participants were asked to walk at a self-selected speed, whereas during the other tests they were asked to perform the task as quickly as possible within safe limits. Prior studies in patients with TKA have shown higher associations between quadriceps muscle strength and functional performance during more demanding tasks.26 Second, the smaller associations between muscle strength and the WOMAC-PF, when compared with the performance-based measures of function, were not surprising. Recent studies in patients with TKA have shown discrepancies in the pattern of associations between the WOMAC-PF and performance-based measures of function. In a sample of patients before and 8 weeks after TKA, the WOMAC-PF scores improved compared with their preoperative values, whereas performance scores worsened.32 Stratford and Kennedy33 reported that within 16 days after TKA, whereas the WOMAC-PF scores did not change, performance-based scores markedly worsened.
The clinical implication of this study is the new finding that hip abduction strength is an independent correlate of physical function in patients with TKA. To date, strength training after TKA has emphasized the quadriceps muscles. If our findings are replicated, the results will be the first step in justifying the need to specifically target the hip abductors during rehabilitation after TKA. Strengthening of the hip abductors could enhance the physical function of these patients. However, before hip abductor strength training becomes a fundamental component of rehabilitation after TKA, longitudinal studies will be needed to determine whether increases in hip abduction strength will improve physical function in patients with TKA.
This study has limitations. The cross-sectional design precludes ascertainment of temporal and causal relationships. For example, functional limitations can adversely affect the strength of quadriceps and hip abduction muscles. Longitudinal studies are needed to confirm the findings. Moreover, this was a pilot and exploratory study with small samples. To deal with this issue, we tried to be very judicious in the selection of covariates. As a result, the models had either 4 or 5 independent variables and a sample size of about 30 participants, which is considered a reasonable sample size for a good prediction level.34 Given the method in which participants were recruited, there also is a possibility of selection bias. Although all patients who had had a TKA during the study time frame were mailed study information, those who were willing to enroll in the study could have been the highly motivated or top performers. We do not believe this was the case because: (1) during the initial interview, we asked the participants why they enrolled in the study, and the common answer was that they believed their performance was below expectations, and (2) the functional level of the participants enrolled in this study is in line with the functional performance of the general population of patients after TKA at a similar time frame after the surgery.1,13,26 Finally, we may not have accounted for all potential confounders of the associations between muscle strength and physical function, such as pain or physical activity. Future and larger studies should consider these issues to improve our understanding of the associations between hip abduction strength and physical function.
Conclusions
The results of this study demonstrated that in patients after TKA, hip abduction strength contributed to physical function over and above demographic or anthropometric measures and quadriceps muscle strength. It appears that the contribution of hip abduction strength to functional limitations in patients with TKA may be as relevant as or more relevant than the contribution of quadriceps muscle strength. Longitudinal studies with larger samples are needed to determine whether increases in hip abduction strength will improve physical function in patients with TKA.
The Bottom Line
What do we already know about this topic?
Although quadriceps femoris muscle weakness has been demonstrated to contribute to functional limitations in patients following total knee arthroplasty, the role of hip abductor weakness is not known.
What new information does this study offer?
Hip abductor strength influenced physical function in patients following total knee arthroplasty more than quadriceps strength or demographic or anthropometric variables.
If you're a patient, what might these findings mean for you?
If the same findings are replicated in larger studies, the hip abductors should be strengthened during rehabilitation after total knee arthroplasty.
Footnotes
Dr Piva, Mr Teixeira, Mr Almeida, Dr DiGioia, Mr Levison, and Dr Fitzgerald provided concept/idea/research design. Dr Piva, Mr Teixeira, Mr Almeida, Dr Gil, Mr Levison, and Dr Fitzgerald provided writing. Mr Teixeira, Mr Almeida, and Dr Gil provided data collection. Dr Piva and Mr Teixeira provided data analysis. Dr Gil provided project management. Dr Piva and Dr Fitzgerald provided fund procurement. Dr DiGioia and Mr Levison provided participants and institutional liaisons. Mr Almeida and Dr Gil provided clerical support. Dr DiGioia, Mr Levison, and Dr Fitzgerald provided consultation (including review of manuscript before submission).
This study was approved by the University of Pittsburgh Institutional Review Board.
This study was supported, in part, by the Claude D. Pepper Older American Independence Center (P30-AG024827); the Central Research Development Fund, University of Pittsburgh; the University of Pittsburgh Medical Center Health System Competitive Medical Research Fund; the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research (KL2 RR024154–02); and the American College of Rheumatology Research Education Foundation New Investigator Award.
Biodex Medical Systems, 20 Ramsay Rd, Shirley, NY 11967-4705.
Velcro USA Inc, PO Box 5218, 406 Brown Ave, Manchester, NH 03103.
CIR Systems Inc, GAITRite Division, 1625 East Darby Rd, Havertown, PA 19083.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1. Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–2604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bradbury N, Borton D, Spoo G, et al. Participation in sports after total knee replacement. Am J Sports Med. 1998;26:530–535 [DOI] [PubMed] [Google Scholar]
- 3. Konig A, Walther M, Kirschner S, et al. Balance sheets of knee and functional scores 5 years after total knee arthroplasty for osteoarthritis: a source for patient information. J Arthroplasty. 2000;15:289–294 [DOI] [PubMed] [Google Scholar]
- 4. Walsh M, Woodhouse LJ, Thomas SG, et al. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258 [DOI] [PubMed] [Google Scholar]
- 5. Mizner RL, Petterson SC, Snyder–Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436 [DOI] [PubMed] [Google Scholar]
- 6. Mizner RL, Petterson SC, Stevens JE, et al. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. J Rheumatol. 2005;32:1533–1539 [PubMed] [Google Scholar]
- 7. Mizner RL, Snyder–Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–1090 [DOI] [PubMed] [Google Scholar]
- 8. Pathokinesiology Service and Physical Therapy Department Observational Gait Analysis. Los Amigos Research and Education Institute Inc, Rancho Los Amigos National Rehabilitation Center: Downey, CA; 2001 [Google Scholar]
- 9. Huang CH, Lee YM, Liau JJ, et al. Comparison of muscle strength of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. J Arthroplasty. 1998;13:779–783 [DOI] [PubMed] [Google Scholar]
- 10. Lorentzen JS, Petersen MM, Brot C, et al. Early changes in muscle strength after total knee arthroplasty: a 6-month follow-up of 30 knees. Acta Orthop Scand. 1999;70:176–179 [DOI] [PubMed] [Google Scholar]
- 11. Berman AT, Bosacco SJ, Israelite C. Evaluation of total knee arthroplasty using isokinetic testing. Clin Orthop Relat Res. 1991;271:106–113 [PubMed] [Google Scholar]
- 12. Steiner ME, Simon SR, Pisciotta JC. Early changes in gait and maximum knee torque following knee arthroplasty. Clin Orthop Relat Res. 1989;238:174–182 [PubMed] [Google Scholar]
- 13. Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183 [DOI] [PubMed] [Google Scholar]
- 14. Lyons K, Perry J, Gronley JK, et al. Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation: an EMG study. Phys Ther. 1983;63:1597–1605 [DOI] [PubMed] [Google Scholar]
- 15. Brown M, Sinacore DR, Binder EF, et al. Physical and performance measures for the identification of mild to moderate frailty. J Gerontol A Biol Sci Med Sci. 2000;55:M350–M355 [DOI] [PubMed] [Google Scholar]
- 16. Shumway–Cook A, Gruber W, Baldwin M, et al. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Phys Ther. 1997;77:46–57 [DOI] [PubMed] [Google Scholar]
- 17. Piva SR, Gil AB, Almeida GJM, et al. A balance exercise program appears to improve function for patients with total knee arthroplasty: a randomized clinical trial. Phys Ther. 2010;90:880–894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Noble PC, Gordon MJ, Weiss JM, et al. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165 [DOI] [PubMed] [Google Scholar]
- 19. Cesari M, Kritchevsky SB, Newman AB, et al. Added value of physical performance measures in predicting adverse health-related events: results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2009;57:251–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Curb JD, Ceria–Ulep CD, Rodriguez BL, et al. Performance-based measures of physical function for high-function populations. J Am Geriatr Soc. 2006;54:737–742 [DOI] [PubMed] [Google Scholar]
- 21. Guralnik JM, Seeman TE, Tinetti ME, et al. Validation and use of performance measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano). 1994;6:410–419 [DOI] [PubMed] [Google Scholar]
- 22. Seeman TE, Charpentier PA, Berkman LF, et al. Predicting changes in physical performance in a high-functioning elderly cohort: MacArthur studies of successful aging. J Gerontol. 1994;49:M97–M108 [DOI] [PubMed] [Google Scholar]
- 23. Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56:M644–M649 [DOI] [PubMed] [Google Scholar]
- 24. Van Swearingen JM, Brack JS, Hess R, et al. Clinical correlates of motor control in walking: the Figure of 8 Walk. Presented at: Annual Meeting of the Gerontological Society of America; November 16–21, 2006; Dallas, Texas [Google Scholar]
- 25. Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840 [PubMed] [Google Scholar]
- 26. Kennedy DM, Stratford PW, Hanna SE, et al. Modeling early recovery of physical function following hip and knee arthroplasty. BMC Musculoskelet Disord. 2006;7:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rowell RK. Partitioning predicted variance into constituent parts: how to conduct regression commonality analysis. Advances in Social Science Methodology. 1996;4:33–43 [Google Scholar]
- 28. Pedhazur EJ. Multiple Regression in Behavioral Research. New York, NY: Harcourt Brace College Publishers; 1982 [Google Scholar]
- 29. Chang A, Hayes K, Dunlop D, et al. Hip abduction moment and protection against medial tibiofemoral osteoarthritis progression. Arthritis Rheum. 2005;52:3515–3519 [DOI] [PubMed] [Google Scholar]
- 30. Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844 [DOI] [PubMed] [Google Scholar]
- 31. Hilliard MJ, Martinez KM, Janssen I, et al. Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil. 2008;89:1708–1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70–80 [DOI] [PubMed] [Google Scholar]
- 33. Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol. 2006;59:160–167 [DOI] [PubMed] [Google Scholar]
- 34. Knofczynski GT, Mundfrom D. Sample sizes when using multiple linear regression for prediction. Educ Psychol Meas. 2008;68:431–442 [Google Scholar]