Abstract
Objective
To validate the verbal autopsy tool for stillbirths of the World Health Organization (WHO) by using hospital diagnosis of the underlying cause of stillbirth (the gold standard) and to compare the fraction of stillbirths attributed to various specific causes through hospital assessment versus verbal autopsy.
Methods
In a hospital in Chandigarh, we prospectively studied all stillbirths occurring from 15 April 2006 to 31 March 2008 whose cause was diagnosed within 2 days. All mothers had to be at least 24 weeks pregnant and live within 100 km of the hospital. For verbal autopsy, field workers visited mothers 4 to 6 weeks after the stillbirth. Autopsy results were reviewed by two independent obstetricians and disagreements were resolved by engaging a third expert. Causes of stillbirths as determined by hospital assessment and verbal autopsy were compared in frequency.
Findings
Hospital assessment and verbal autopsy yielded the same top five underlying causes of stillbirth: pregnancy-induced hypertension (30%), antepartum haemorrhage (16%), underlying maternal illness (12%), congenital malformations (12%) and obstetric complications (10%). Overall diagnostic accuracy of verbal autopsy diagnosis versus hospital-based diagnosis for all five top causes of stillbirth was 64%. The areas under the receiver operator characteristic curve (ROC) were, for congenital malformations, 0.91 (95% confidence interval, CI: 0.83–0.97); pre-gestational maternal illness, 0.75 (95% CI: 0.65–0.84); pregnancy-induced hypertension, 0.76 (95% CI: 0.69–0.81); antepartum haemorrhage, 0.76 (95% CI: 0.67–0.84) and obstetric complication, 0.82 (95% CI: 0.71–0.93).
Conclusion
The WHO verbal autopsy tool for stillbirth can provide reasonably good estimates of common underlying causes of stillbirth in resource-limited settings where a medically certified cause of stillbirth may not be available.
Résumé
Objectif
Valider l'outil de l'autopsie verbale de l'Organisation mondiale de la Santé dans le cadre des mortinaissances en recourant au diagnostic hospitalier de la cause sous-jacente de la mortinaissance (modèle idéal) et comparer la part des mortinaissances attribuée à différentes causes spécifiques selon l'évaluation de l'hôpital d'une part, et l'autopsie verbale, d'autre part.
Méthodes
Dans un hôpital de Chandigarh, nous avons étudié de manière prospective toutes les mortinaissances survenues du 15 avril 2006 au 31 mars 2008 et dont les causes avaient été diagnostiquées dans les 2 jours suivant l'évènement. Toutes les mères devaient avoir eu une grossesse d’une durée minimale de 24 semaines et résider dans un périmètre maximum de 100 km autour de l'hôpital. Pour réaliser l'autopsie verbale, les agents de terrain ont rendu visite aux mères 4 à 6 semaines après la mortinaissance. Les résultats de l'autopsie ont ensuite été examinés par deux obstétriciens indépendants et leurs divergences ont été résolues par l'engagement d'un troisième expert. Les causes des mortinaissances, telles que déterminées par l'évaluation hospitalière et par l'autopsie verbale, ont été comparées en fonction de leur fréquence.
Résultats
L'évaluation hospitalière et l'autopsie verbale ont rapporté cinq causes sous-jacentes principales identiques de la mortinaissance: hypertension liée à la grossesse (30%), hémorragie ante partum (16%), pathologie maternelle sous-jacente (12%), malformations congénitales (12%) et complications obstétriques (10%). L'exactitude générale de l'autopsie verbale au regard du diagnostic hospitalier, pour les cinq causes principales de mortinaissance, était de 64%. Les aires sous la courbe de caractéristique de fonctionnement du récepteur étaient, pour les malformations congénitales, 0,91 (95% intervalle de confiance, IC: 0,83–0,97); les pathologies maternelles prégestationnelles, 0,75 (95% IC: 0,65–0,84); l'hypertension due à la grossesse, 0,76 (95% IC: 0,69–0,81); l'hémorragie ante partum, 0,76 (95% IC: 0,67–0,84) et les complications obstétriques, 0,82 (95% IC: 0,71–0,93).
Conclusion
L’outil d’autopsie verbale de l’OMS en matière de mortinaissance peut fournir des estimations relativement bonnes des causes communes sous-jacentes de la mortinaissance chez les familles aux ressources limitées, pour lesquelles une cause de mortinaissance médicalement certifiée peut ne pas être disponible.
Resumen
Objetivo
Validar las entrevistas verbales a parientes y allegados para determinar las causas de la mortinatalidad que utiliza la Organización Mundial de la Salud (OMS), empleando el diagnóstico hospitalario de las causas subyacentes a la mortinatalidad («criterio de referencia») y comparar la proporción de mortinatos atribuidos a determinadas causas específicas, a través de la valoración del hospital, en comparación con los resultados de las investigaciones verbales.
Métodos
Realizamos un estudio prospectivo de todos los mortinatos que nacieron en un hospital de Chandigarh (India) entre el 15 de abril de 2006 y el 31 de marzo de 2008 y cuya causa de defunción se diagnosticó dentro de un plazo de 2 días. Todas las madres debían encontrarse como mínimo en la semana 24 de gestación y vivir dentro de un radio de 100 km del hospital. Para las entrevistas verbales, los trabajadores en el terreno visitaron a las madres entre las 4 y las 6 semanas posteriores a la mortinatalidad. Dos obstetras independientes revisaron los resultados de las autopsias y, en caso de desacuerdo, se solicitó la participación de un tercer experto. Se comparó la frecuencia de las causas de la mortinatalidad, según lo establecido por la valoración hospitalaria y por las investigaciones verbales.
Resultados
Tanto la valoración hospitalaria como la entrevista verbal coincidieron en cuáles eran las cinco causas de mortinatalidad más frecuentes: preeclampsia (30%), hemorragia prenatal (16%), enfermedad subyacente de la madre (12%), malformaciones congénitas (12%) y complicaciones obstétricas (10%). La precisión general del diagnóstico mediante investigación verbal, en comparación con el diagnóstico basado en la información hospitalaria para las cinco causas más frecuentes de mortinatalidad, fue del 64%. Las áreas bajo la curva de eficacia diagnóstica (ROC) fueron: para las malformaciones congénitas, 0,91 (intervalo de confianza del 95%, IC: 0,83–0,97); enfermedad pre-gestacional de la madre, 0,75 (95%, IC: 0,65–0,84); preeclampsia, 0,76 (95%, IC: 0,69–0,81); hemorragia prenatal, 0,76 (95%, IC: 0,67–0,84) y complicaciones obstétricas, 0,82 (95%, CI: 0,71–0,93).
Conclusion
La herramienta de investigación verbal de la mortinatalidad que emplea la OMS puede ofrecer unas estimaciones razonablemente aceptables de las causas subyacentes más frecuentes a la mortinatalidad en los ámbitos con recursos limitados, en los que la causa de mortinatalidad pueda no estar certificada por un médico.
ملخص
الغرض
التحقق من صلاحية التشريح السردي كأداة لمنظمة الصحة العالمية في تحديد أسباب الإملاص عن طريق استخدام تشخيص المستشفى للسبب الدفين للإملاص (والذي يعد معياراً ذهبياً) ومقارنة نسبة الإملاص لمختلف الأسباب المحددة من خلال مقارنة تقييم المستشفى لقاء التشريح السردي.
الطريقة
أجرى الباحثون، في مستشفى تشانديغارا، دراسة مستقبلية لجميع حالات الإملاص التي وقعت منذ 15 نيسان/أبريل 2006 حتى 31 آذار/مارس 2008 والتي جرى تشخيصها خلال يومين. جميع الأمهات كن حوامل لمدة 24 أسبوعاً على الأقل ويعشن على بعد أقل من 100 كيلومتر من المستشفى. وقد زار العاملون الميدانيون الأمهات خلال 4 إلى 6 أسابيع بعد ولادتهن لولدان أموات. وروجعت نتائج التشريح من قبل طبيبين مستقلين مختصين في الولادة، وفي حال وجود اختلاف للرأي يبت في الأمر بينهما خبيرٌ ثالث، ثم قورن تواتر أسباب الإملاص حسب تقييم المستشفى وحسب التشريح السردي.
النتائج
أفضى تقييم المستشفى والتشريح السردي إلى نفس أعلى خمسة أسباب دفينة مفضية للإملاص وهي: فرط ضغط الدم الناجم عن الحمل (30%) والنزف في الفترة السابقة للولادة (16%)، وأمراض الأمومة الدفينة (12%)، والتشوهات الخلقية (12%)، ومضاعفات الولادة (10%). وبلغت دقة التشخيص في التشريح السردي مقابل التشخيص المعتمد على المستشفى لأعلى خمسة أسباب مفضية للإملاص 64%. والمساحة أسفل منحنى خواص العامل المتلقي كانت، بالنسبة للتشوهات الخلقية 0.91 (فاصلة الثقة CI 95%: 0.83-0.97) وبالنسبة لأمراض الأمومة السابقة للحمل 0.75(فاصلة الثقة CI 95%: 0.65-0.84)؛ وفرط ضغط الدم الناجم عن الحمل 0.76 (فاصلة الثقة CI 95%: 0.69-0.81)؛ والنزف السابق للولادة 0.76 (فاصلة الثقة CI 95%: 0.67-0.84)؛ ومضاعفات الولادة 0.82(فاصلة الثقة CI 95%: 0.71-0.93).
الاستنتاج
إن التشريح السردي كأداة لمنظمة الصحة العالمية في تحديد الإملاص يوفّر تقديراتٍ جيدة بدرجة معقولة حول الأسباب الدفينة الشائعة للإملاص وذلك في المواقع المحدودة الموارد حيث لا يتوفّر سبب طبي موّثق للإملاص.
Резюме
Цель
Оценить надежность разработанного Всемирной организацией здравоохранения (ВОЗ) стандартного инструмента по проведению вербальной аутопсии при определении причин мертворождений путем использования поставленного в больнице диагноза основной причины мертворождения («золотого стандарта») и сравнить процентные доли мертворождений, вызванных различными конкретными причинами, по материалам оценки, проведенной в больнице, и по данным вербальной аутопсии.
Методы
Нами проведено проспективное исследование всех мертворождений в больнице г. Чандигарх в период с 15 апреля 2006 г. по 31 марта 2008 г., причины которых были диагностированы в течение двух дней. Срок беременности у всех матерей должен был составлять не менее 24 недель, и они должны были проживать в радиусе 100 км от больницы. Для проведения вербальной аутопсии полевые работники посещали матерей в течение 4–6 недель после мертворождения. Результаты аутопсии проверялись двумя независимыми акушерами, а для разрешения возникающих разногласий привлекался третий эксперт. Причины мертворождений, установленные в результате оценки, проведенной в больнице, и вербальной аутопсии, сравнивались по частоте.
Результаты
Оценка, проведенная в больнице, и вербальная аутопсия выявили одни и те же пять основных причин мертворождений: повышенное давление, вызванное беременностью (30%), послеродовое кровотечение (16%), имеющееся в анамнезе заболевание матери (12%), врожденные пороки (12%) и акушерские осложнения (10%). В целом точность диагнозов, поставленных на основании вербальной аутопсии, по сравнению с диагнозами, поставленными в больнице, для пяти главных причин мертворождений, составляла 64%. Области под кривой рабочей характеристики наблюдателя (receiver operator characteristic curve, ROC) составляли: для врожденных пороков -- 0,91 (доверительный интервал (ДИ) 95%: 0,83–0,97); для заболевания матери до беременности – 0,75 (95% ДИ: 0,65–0,84); для повышенного давление, вызванного беременностью, – 0,76 (95% ДИ: 0,69–0,81); для послеродового кровотечения – 0,76 (95% ДИ: 0,67–0,84) и для акушерского осложнения – 0,82 (95% ДИ: 0,71–0,93).
Вывод
С помощью разработанного ВОЗ инструмента по проведению вербальной аутопсии при определении причин мертворождений можно достаточно качественно оценить наиболее распространенные основные причины мертворождений в условиях ограниченности ресурсов, когда невозможно установить медицински-сертифицированную причину мертворождения.
摘要
目的
旨在通过死胎根本死因的医院诊断(金标准)证明世界卫生组织的死胎死因推断工具的有效性,并通过医院评估及死因推断来比较各种具体原因的死胎比率。
方法
在昌迪加尔的一家医院,我们前瞻性地研究了从2006年4月15日至2008年3月31日期间发生的所有死胎,其原因均在死亡发生后的两天内确诊。所有母亲至少有24周的身孕并且住在医院方圆100公里的范围以内。为了进行死因推断,实地调查员在死胎发生后的4至6周内走访了这些母亲们。死因推断结果由两位独立的产科医师审查,如有分歧通过第三位专家解决。由医院评估确定的死胎原因和通过死因推断确定的死胎原因做了频率比较。
发现
医院评估和死因推断得出了相同的五大根本死胎原因:妊娠高血压(30%),产前出血(16%),潜在产妇疾病(12%),先天畸形(12%)和产妇并发症(10%)。对于五大死胎原因,死因推断诊断相对医院诊断的准确率为64%。受试者工作特征曲线(ROC)下的面积分别为:先天畸形,0.91(95%置信区间,Cl:0.83-0.97);妊娠前产妇疾病,0.75(95%置信区间,Cl:0.65-0.84);妊娠高血压,0.76(95%置信区间,Cl:0.69-0.81);产前出血,0.76(95%,Cl:0.67-0.84)和产妇并发症,0.82(95%置信区间,Cl:0.71-0.93)。
结论
世界卫生组织的死因推断工具能够为资源有限且无法提供死胎原因医学证明的地区提供一个较为理想的估计方法。
Introduction
Over 3 million stillbirths occur in the world every year.1 Whereas the main direct causes of neonatal death have been identified as preterm birth, severe infections and asphyxia,2 data on the causes of stillbirth are grossly insufficient. The available data, which is largely hospital-based, suggests that in developing countries prolonged and obstructed labour, pre-eclampsia and infections account for the majority of stillbirths,3 yet such data may be unreliable because in countries in development most deliveries take place at home.4 Furthermore, hospitals are poorly equipped to assign causes of stillbirth appropriately and civil registration systems with medical certification of causes of death are not well established.
Several countries rely on verbal autopsies to generate information on causes of death. However, verbal autopsy questionnaires, field operations and the definitions used to classify the deaths vary widely in different places.5 To fulfil the need for a standard international classification system for assigning cause of death by verbal autopsy,3 the World Health Organization (WHO) developed a tool containing a set of standards for neonatal deaths and stillbirths.6 However, the tool requires validation in countries having different patterns of mortality.7
Whereas several verbal autopsy validation studies have been performed for infant and early childhood deaths,8–10 only two validation studies for stillbirth have been reported so far.11,12 Both were retrospective hospital-based studies, one of which had a long recall period and the other combined stillbirths with early neonatal deaths. Moreover, differences in the prevalence of underlying causes of death make it important to conduct verbal autopsy validation studies in different epidemiological settings.13 Hence, this study was conducted to assess the validity of the WHO verbal autopsy tool for ascertaining major causes of stillbirth and to compare the fraction of stillbirths attributed to specific causes on the basis of hospital assessment versus verbal autopsy.
Methods
This prospective study was carried out during 2006–2008 in a tertiary care hospital in Chandigarh, a city in northern India. Participants of a WHO proposal development workshop assessed proposals submitted by research teams from Bangladesh, Ghana, India and Pakistan, all of whom attended the workshop, and selected this particular study after considering each team’s experience in evaluating verbal autopsy, the overall quality of each proposal and the rates of stillbirth and neonatal mortality in the four candidate countries. Moreover, verbal autopsies were felt to be useful in monitoring the impact of efforts being made by the Government of India to improve maternal and neonatal care through innovative schemes, such as janani suraksha yojna [women’s safety plan], to promote institutional deliveries for safe childbirth. At the time of the study, the rate of stillbirth, defined as the number of fetal deaths divided by the number of live births plus fetal deaths in a particular year, was around 30 per 1000 births in the neighouring states of Punjab and Haryana.14,15 The year before this study was initiated, a total of 3913 deliveries and 281 stillbirths had taken place in the institute covering Chandigarh and the nearby states of Punjab, Haryana, Himachal Pradesh and Uttar Pradesh.
All stillbirths that occurred in the study hospital from 15 April 2006 to 31 March 2008 to mothers who resided no more than 100 km from the hospital and who were at least 24 weeks pregnant were eligible for the study. An additional inclusion criterion was the assignment of the cause of death within 2 days of the stillbirth to minimize recall bias and ensure as accurate a hospital-based diagnosis as possible. The first set of criteria were met by 353 stillbirths, but only 294 of them had had a cause of death assigned within the stipulated 2 days. Verbal autopsies were conducted between 4 and 6 weeks after the event in 225 of these 294 cases (77%), since 50 families could not be traced and either the mother was not available or consent was denied in another 19 cases. These 225 cases, for which complete hospital and verbal autopsy information was available, were the ones included in our analysis. We compared the stillbirths that were included in the final analysis with those for which verbal autopsy could not be performed to check for any systematic difference between the two groups in terms of maternal age, gestational age, birth weight, maternal haemoglobin status, occurrence of multiple births or lethal congenital malformations. No specific questions were asked about acute infectious or traumatic conditions that may have affected the pregnancy and led to stillbirth, although general questions regarding problems in the first, second and third trimester were formulated and the details were recorded.
Study tools
A structured clinical case sheet was used to record maternal age; date of last menstrual period; maternal history of chronic conditions such as diabetes mellitus, chronic hypertension, epilepsy, renal or hepatic disease; obstetric and antenatal history; findings on clinical examination; fetal heart sounds and antenatal ultrasound results; details of labour and delivery and results of gross examination of the stillborn and placenta. The case sheet was also structured to record the results of relevant laboratory tests.
To conduct the verbal autopsies we used the WHO verbal autopsy tool for stillbirths, slightly modified to improve cultural sensitivity and eliminate questions unrelated to the purpose of our study. The tool’s questionnaire, which contained seven sections, was translated in the local languages (Hindi and Punjabi), back-translated to ensure content validity and pre-tested. The first page was designed to enter the data from the hospital case sheet. Sections 1 and 2 were for background information, such as identification number, interview date and sociodemographic characteristics of the respondents. Section 3 contained questions to differentiate between a stillbirth and a neonatal death. Specific questions related to stillbirth were subsequently asked only if the event had been identified as a stillbirth in section 3. Section 4 was for recording verbatim an open narrative of the history of the entire pregnancy until delivery of the stillborn. This was followed by specific close-ended questions to explore maternal history during the pregnancy, labour and delivery (section 5), the condition of the baby when delivered (section 6) and the stillborn’s appearance (section 7). Photographs of macerated and fresh stillborn babies and of neonates having low birth weight and major congenital malformations were shown to the families while questions relating to the stillborn’s condition were being asked. A professional photographer took the photographs in the local hospital with family consent. A few photographs of rarer major congenital anomalies and macerated stillbirths were downloaded from the Internet. The entire set of photographs was pretested on health workers and on women in the postnatal ward who had recently given birth.
Training of the study team
Field workers with school-level education (10th grade) were trained to conduct interviews and record the responses to the verbal autopsy questionnaires using the interview guide. Training methods included classroom presentation, discussion and role plays. All questions were discussed with project staff to clarify the clinical terms and the response choices. Pictures and other visual aids were used as required. Completed verbal autopsy forms from a former study were used as models by the principal investigator to train field workers. Each worker conducted five interviews in which the principal investigator acted as the mother and responded in accordance with the completed verbal autopsy form. Repeat interviews were conducted by the same field worker in a different order. The principal investigator observed and noted the differences in the responses obtained for the same case by different workers and also by the same worker. Workers were then given feedback about the discrepancies observed in the interview. The process was repeated with different case studies until no more discrepancies were noted. Later, one of the investigators (AKA) observed the process of conducting the verbal autopsy in the homes. This helped make the staff more sensitive to bereavement-related issues.
Project medical officers were trained to retrieve the clinical information from the clinical case files, and supervisors were taught to check data collection forms for completeness and accuracy. A senior supervisor randomly checked members of the project team to ensure that the project was proceeding as planned and to resolve any problems on site. The senior supervisor also gave the principal investigator a list of the verbal autopsies conducted every week from which to draw a sample for the supervisory visits in the homes. Data managers were trained on how to maintain the data set, generate periodic reports and keep data backups. A team of clinicians was trained to record the causes of stillbirths on the international death certificate and to codify them in accordance with the International statistical classification of diseases and related health problems, 10th revision (ICD-10).16 All team members received instruction on ways to ensure confidentiality.
Definitions of stillbirth
In the hospital, a baby was classified as stillborn if no fetal heart sounds could be heard during labour by a trained obstetrician using a stethoscope (with confirmation by Doppler ultrasound whenever this was available, which was in most cases) and the neonatologist perceived no signs of life in the neonate upon physical examination at delivery. For a baby to be considered stillborn by verbal autopsy, the family had to report that the baby had been “born dead” and had never been observed to cry, move or breathe even slightly.
Enrolment of stillbirths
Trained medical officers visited the hospital on all working days and recorded the stillbirths that had occurred over the previous 24 hours. Stillbirths that took place on Sundays or holidays were registered on the following working day. The medical officer who recorded the identification details for each stillborn took down the family’s complete address and telephone number, if available, and prepared a guide map to locate the house. The medical officers retrieved the clinical information in the clinical case files and discussed it with the appropriate attending physician within 48 hours of the occurrence of each stillbirth to fill any potential gaps in the clinical history and laboratory data. They then gave the complete information to the clinical investigator. All stillbirths that occurred in the hospital during the study period were screened for compliance with inclusion criteria and eligible stillbirths were enrolled in the study. As explained earlier, however, only 225 cases were eventually considered in the final analysis.
Verbal autopsy interviews
From 4 to 6 weeks after each stillbirth, two trained female field workers visited the household of the deceased to conduct a verbal autopsy interview. If a telephone number was available, an advance appointment was made with an appropriate respondent (e.g. the mother or, in her absence, an adult respondent who had been with her at the time of the stillbirth). If the respondent was not available on the first visit, at least one repeat visit was made until the respondent was found. The field workers obtained written informed consent in the local language in every household they visited before conducting each interview, also in the local language. To obtain consent, they read the contents of the consent information sheet out loud to each respondent, who was given the opportunity to ask the questions. During the interview, photographs of babies with major congenital malformations and of babies who were stillborn and appeared macerated or who had various grades of prematurity or low birth weight were used to help respondents’ recall. It took an average of 30 minutes to complete all seven sections of the verbal autopsy, which were administered in sequence.
Quality assurance
The study was approved by the hospital’s ethics committee and WHO’s Ethics Review Committee. Respondents’ information was kept confidential. Quality was assured through weekly review meetings and supervisory field visits. Investigators drew a weekly random sample of 10% of the stillbirths. Field visits were also conducted during two of the review meetings by a staff member of WHO, the funding organization, to determine if procedures were being properly followed in the hospital and in the field.
Supervisors visited the sampled houses to verify whether the field workers had come by and interviewed an appropriate respondent. The households of 12 stillborns were revisited. The families had been pre-informed by field workers during the verbal autopsy visits that a supervisor would perhaps be calling on them. Supervisors called the sampled families whose telephone numbers were available to obtain their verbal consent for the supervisory interview, and they again sought the families’ consent upon reaching the households. After confirming that a field worker had already visited and conducted an interview, the supervisors filled out a form with information about the stillborn and explained to the families that the information was being collected again to verify the correctness of the facts taken down by the field worker. The forms filled out by the supervisors and the field workers were subsequently compared.
We calculated kappa values to assess agreement between field workers and supervisors on five key questions aimed at: (i) distinguishing a stillbirth from a neonatal death; (ii) determining the presence of underlying chronic maternal illness and high blood pressure; (iii) differentiating spontaneous labour from induced labour; and (iv) distinguishing spontaneous delivery from instrumental or Caesarean delivery. Any discordant results were discussed with the entire team at weekly meetings to ensure continuous quality improvement in recording and collecting the data.
Cause of death assignment
The clinical investigator (VJ) discussed all the available clinical and laboratory information on each stillbirth with the team of attending obstetricians and filled the international death certificate, where an underlying cause of death had to be indicated. The hospital diagnosis was based on standard obstetric guidelines and reflected the best judgment of the clinical investigator and the attending obstetricians. Thus, it was used as the gold standard for validating WHO’s verbal autopsy tool for stillbirth.
Verbal autopsy forms were reviewed by a second panel of two independent obstetricians whose experience was similar to that of the obstetricians working in the study hospital. These independent experts were blinded to the clinical information and to the hospital-based diagnosis of the cause of death and were provided with standard definitions (Box 1) and asked to follow the ICD-10 to hierarchically classify the causes of stillbirth. The ICD-10 defines the underlying cause of stillbirth as the disease or condition that triggered the chain of events leading to the death. Conditions that occurred early in the chronological order of events are placed higher in the hierarchy than conditions that originated later. For example, if a neonate with a severe congenital anomaly was also premature at birth, the underlying cause of stillbirth was recorded as congenital anomaly. The definitions were based on those developed by WHO in 20036 and the classification system for causes of death was adapted from the Neonatal and Intrauterine Death Classification according to Etiology (NICE).17 The obstetricians who read the verbal autopsies filled out a death certificate similar to the one used by the clinical investigator. In cases of disagreement between the two obstetricians, a third expert was asked to review the forms. If this third expert’s diagnosis agreed with that of either obstetrician, that diagnosis was taken as the final one. If the third expert did not agree with either obstetrician, the cause of death was classified as undetermined.
Box 1. Definitions used in study conducted to validate the World Health Organization’s verbal autopsy tool for stillbirth,6 Chandigarh, India.
Antepartum death: death before labour as evidenced by either maceration of the stillborn or by a report of loss of fetal movements before the onset of labour, even without maceration.
Intrapartum death: death during labour, as evidenced by lack of maceration and by a reporting of fetal movements after the onset of labour.
Congenital malformations: any lethal physical anomaly or one accompanied by a markedly increased risk of death (e.g. anencephaly, large meningomyelocoele).
Underlying chronic maternal illness predating the pregnancy and parameter(s) for determining its presence:
Diabetes mellitus: report of diagnosed diabetes mellitus before pregnancy;
Chronic hypertension: report of hypertension diagnosed before pregnancy or in the first 20 weeks of pregnancy;
Epilepsy: history of epileptic convulsions or of use of anti-epileptic drugs during pregnancy;
Liver disease: history of deep jaundice during pregnancy, with or without severe itching and altered state of consciousness.
Pregnancy-induced hypertension: report of high blood pressure with swelling of hands or face, blurring of vision and severe headache:
Eclampsia: if hypertension associated with convulsions or unconsciousness.
Antepartum haemorrhage: vaginal bleeding (sometimes retained in the uterus) after the 22nd week of gestation. Causes:
Placenta previa: bleeding not associated with pain;
Abruptio placentae: bleeding associated with intermittent or constant abdominal pain (other than labour pain).
Obstetric complications:
Malpresentations: any part of the body other than the head delivered first;
Cord prolapse: umbilical cord delivered first;
Obstructed labour: labour lasting > 12 hours. Eventual delivery with manual manipulation, use of instruments for extraction or surgical intervention.
Statistical analysis
The fraction of stillbirths attributed to specific underlying causes was calculated for both hospital and verbal autopsy diagnosis. The sensitivity, specificity, positive predictive value and negative predictive value of verbal autopsy were estimated, with their 95% confidence intervals (CIs), for the five most common underlying causes of stillbirths, with the hospital diagnosis used as the gold standard. The diagnostic accuracy of verbal autopsy was also calculated for each of these five causes of death, both individually and for all causes combined.
The calculations were repeated after these most common underlying causes of stillbirths resulting from verbal autopsy were re-categorized to allow for multiple causes of death. If any of these five causes of stillbirth were registered as a direct, antecedent or underlying cause in the verbal autopsy death certificate, by either reviewer, it was considered a cause of death and its frequency after hospital and verbal autopsy assessment was compared. The area under the receiver operator characteristic (ROC) curve, which shows the trade-off between sensitivity and specificity, was calculated for both classification methods. For the performance of the verbal autopsy tool to be considered adequate, the area under the ROC curve had to be at least 0.75 and the tool’s sensitivity and specificity had to be above 60% and 85%, respectively.6,18
Results
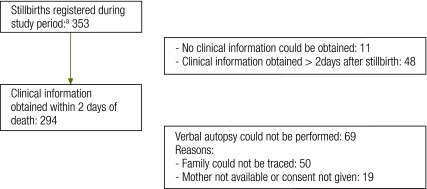
A total of 570 stillbirths occurred in the hospital during the study period. Of these stillbirths, 353 met the study’s inclusion criteria but only 294 could be enrolled. The final analysis was based on 225 cases for which a verbal autopsy was performed (Fig. 1). Verbal autopsy interview respondents had mean age of 27 years (standard deviation, SD: 5.6) and a mean of 8 (SD: 5.4) years of schooling. Of the stillbirths that met the inclusion criteria, those that were included in the final analysis did not differ significantly from those that could not be included with respect to maternal age, gestational age, birth weight, maternal haemoglobin status, occurrence of multiple births or lethal congenital malformations. The kappa values to test the agreement between field workers and supervisory information revealed that for different questions it ranged from 0.437 to 1.0 indicating good to perfect agreement.
Fig. 1.
Selection of stillbirths for inclusion in study conducted to validate the World Health Organization’s verbal autopsy tool for stillbirth, Chandigarh, India
a 15 April 2006 to 31 March 2008.
Stillbirths and neonatal deaths
During verbal autopsy, the families of 18 stillborns reported that the babies had been born alive. Almost half of these stillborns had lethal congenital anomalies or fetal conditions. Based on the clinical information available and on the results of verbal autopsy, the clinical investigator and the panel of obstetricians respectively classified all deaths as being either antepartum or intrapartum, regardless of the cause. In the hospital, 150 (66.6%) stillbirths were classified as antepartum, 69 (30.6%) as intrapartum and 6 (2.7%) as indeterminate; after verbal autopsy, 114 (50.7%) stillbirths were classified as antepartum, 93 (41.3%) as intrapartum and 18 (8%) as indeterminate.
Cause-specific mortality
The fraction of stillbirths attributed to the five leading underlying causes as determined by hospital assessment versus verbal autopsy are presented in Table 1. Clinical diagnosis yielded a somewhat higher proportion of stillbirths due to underlying maternal disease, pregnancy-induced hypertension and specific fetal conditions than did verbal autopsy. On the other hand, the proportion of stillbirths with unexplained preterm birth, asphyxia unexplained by the mother’s condition and other unexplained problems was somewhat higher for verbal autopsy. In total, verbal autopsy resulted in 18.2% unexplained stillbirths, compared with 12.4% for hospital diagnosis. Babies who were small for gestational age comprised a good fraction of unexplained stillbirths in the case of hospital-based as well as verbal autopsy diagnosis. Preterm births comprised 4% of the unexplained stillbirths diagnosed through verbal autopsy and 0% of those diagnosed in the hospital.
Table 1. Causes of stillbirth, unexplained stillbirths and unexplained non-specific fetal problems, as determined through clinical assessment versus verbal autopsy conducted with the World Health Organization’s verbal autopsy tool for stillbirth,6 Chandigarh, India.
| Diagnostic category | Clinical assessment (n = 225) | Verbal autopsy (n = 225) |
|---|---|---|
| No. (%) | No. (%) | |
| Congenital malformations | 27 (12.0) | 31 (13.8) |
| Multiple pregnancy | 5 (2.2) | 7 (3.1) |
| Underlying maternal illnessa | 29 (12.9) | 19 (8.4) |
| Pregnancy-induced hypertension | 69 (30.7) | 57 (25.3) |
| Antepartum haemorrhage | 35 (15.6) | 38 (16.9) |
| Obstetric complications | 19 (8.4) | 21 (9.3) |
| Asphyxia not explained by any maternal condition | 4 (1.8) | 11 (4.9) |
| Other specific fetal problem | 9 (4.0) | 0 (0) |
| Unexplained stillbirth | 23 (10.2) | 18 (8.0) |
| Unexplained small size for gestational date | 0 (0) | 10 (4.4) |
| Unexplained preterm birth (< 37 weeks gestation) | 5 (2.2) | 13 (5.7) |
a The main underlying chronic maternal illnesses were, in descending order of frequency, chronic hypertension, epilepsy, renal disease, liver disease and diabetes mellitus.
Diagnostic accuracy
The five leading causes explained 80% of the stillbirths, and each cause accounted for at least 8% of them. Hence, these five leading causes were used to calculate the diagnostic accuracy of WHO’s verbal autopsy tool for stillbirth against that of hospital assessment.
Table 2 shows the sensitivity, specificity, positive predictive value, negative predictive value and area under the ROC curve for the verbal autopsy tool when used to diagnose a single underlying cause of stillbirth among the five leading causes identified. The overall diagnostic accuracy of the tool was 64% for these top five underlying causes of stillbirth combined. However, its diagnostic accuracy for any single cause was very high (78–95%).
Table 2. Validity of the World Health Organization’s verbal autopsy tool for stillbirth6 as determined by comparing the underlying cause of stillbirth diagnosed with the toola with hospital-based diagnosis, Chandigarh, India.
| Underlying cause of stillbirtha | Sensitivity |
Specificity |
PPV |
NPV |
DAb |
Area under ROC curvec |
|||
|---|---|---|---|---|---|---|---|---|---|
| VAD/HDd | % (95% CI) | VAD/HDe | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | Value (95% CI) | ||
| Congenital malformations | 23/27 | 85.2 (65.4–95.1) | 190/198 | 96.0 (91.9–98.1) | 74.2 (55.1–87.5) | 97.9 (94.5–99.3) | 95 (82–106) | 0.91 (0.83–0.97) | |
| Underlying maternal illnessf | 15/29 | 51.7 (32.9–70.1) | 192/196 | 98.0 (94.5–99.3) | 78.9 (53.9–93.0) | 93.2 (88.6–96.1) | 92 (74–109) | 0.75 (0.65–0.84) | |
| Pregnancy-induced hypertension | 42/69 | 60.9 (48.4–72.2) | 141/156 | 90.4 (84.4–94.3) | 73.7 (60.1–84.1) | 83.9 (77.3–89.0) | 81 (69–93) | 0.76 (0.69–0.81) | |
| Antepartum haemorrhage | 21/35 | 60.0 (42.2–75.6) | 173/190 | 91.1 (85.8–94.5) | 55.3 (38.5–71.0) | 92.5 (87.3–95.7) | 86 (70–102) | 0.76 (0.67–0.84) | |
| Obstetric complications | 13/19 | 68.4 (43.5–86.4) | 198/206 | 96.1 (92.2–98.2) | 61.9 (38.7–81.0) | 97.1 (93.4–98.8) | 94 (76–111) | 0.82 (0.71–0.93) | |
CI, confidence interval; DA, diagnostic accuracy; HD, hospital-based diagnosis; NPV, negative predictive value; PPV, positive predictive value; ROC, receiver operator characteristic; VAD, verbal autopsy diagnosis.
a The underlying causes of stillbirth were classified in accordance with the International statistical classification of diseases and related health problems, 10th revision.16 Diseases or conditions that occur early in the chronology of events are placed higher in the order.
c The area under the ROC curve captures the relationship between the sensitivity and specificity of a diagnostic tool or method and is therefore indicative of diagnostic performance with respect to a given condition. Because it is a probability, it takes on values between 0 and 1. A larger value generally indicates better diagnostic performance.
d Number of positives correctly diagnosed through verbal autopsy divided by number of positives diagnosed in hospital (gold standard).
e Number of negatives correctly diagnosed through verbal autopsy divided by number of negatives diagnosed in hospital (gold standard).
f The main underlying chronic maternal illnesses were, in descending order of frequency, chronic hypertension, epilepsy, renal disease, liver disease and diabetes mellitus.
b ([True positives + true negatives] ÷ 225) × 100.
When the scope of verbal autopsy diagnosis was expanded from a single underlying cause to multiple causes (i.e. when the diagnosis was listed as either an underlying cause, a direct cause, an antecedent cause or a contributory cause by any of the reviewers), the sensitivity of the tool for most causes of death improved. However, its specificity dropped for all causes (Table 3).
Table 3. Validity of the World Health Organization’s verbal autopsy tool for stillbirth6 as determined by comparing the cause of stillbirth of any type (direct, antecedent or underlying) diagnosed with the toola with hospital-based diagnosis, Chandigarh, India.
| Cause of stillbirth | Sensitivity |
Specificity |
PPV |
NPV |
DAb |
Area under ROC curvec |
|||
|---|---|---|---|---|---|---|---|---|---|
| VAD/HDd | % (95% CI) | VAD/HDe | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | Value (95% CI) | ||
| Congenital malformations | 25/27 | 92.6 (74.2–98.7) | 187/198 | 94.4 (90.0–97.1) | 69.4 (51.7–83.1) | 98.9 (95.8–99.8) | 94 (82–106) | 0.93 (0.88–0.99) | |
| Underlying maternal illnessf | 19/29 | 65.5 (45.7–81.4) | 168/196 | 85.7 (79.8–90.1) | 40.4 (26.7 −55.7) | 94.4 (89.6–97.1) | 83 (67–99) | 0.76 (0.66–0.85) | |
| Pregnancy-induced hypertension | 45/69 | 65.2 (52.7–76.0) | 131/156 | 84.0 (77.1–89.2) | 64.3 (51.9 −75.1) | 84.5 (77.6–89.6) | 78 (66–90) | 0.75 (0.68–0.81) | |
| Antepartum haemorrhage | 24/35 | 68.6 (50.6–82.6) | 159/190 | 83.7 (77.5–88.5) | 43.6 (30.6–57.6) | 93.5 (88.4–96.6) | 81 (67–95) | 0.76 (0.68–0.84) | |
| Obstetric complications | 14/19 | 73.7 (48.6–89.9) | 193/206 | 93.7 (89.2–96.5) | 51.9 (32.4–70.8) | 97.5 (93.9–99.1) | 92 (74–110) | 0.83 (0.73–0.94) | |
CI, confidence interval; DA, diagnostic accuracy; HD, hospital-based diagnosis; NPV, negative predictive value; PPV, positive predictive value; ROC, receiver operator characteristic; VAD, verbal autopsy diagnosis.
a This includes any cause of stillbirth reported by either of two reviewers as the direct, antecedent or underlying cause of death. For example, pregnancy-induced hypertension could have been designated as the underlying cause by one reviewer and as the antecedent cause by another.
c The area under the ROC curve captures the relationship between the sensitivity and specificity of a diagnostic tool or method and is therefore indicative of diagnostic performance with respect to a given condition. Because it is a probability, it takes on values between 0 and 1. A larger value generally indicates better diagnostic performance.
d Number of positives correctly diagnosed through verbal autopsy (true positives) divided by number of positives diagnosed in hospital (gold standard).
e Number of negatives correctly diagnosed through verbal autopsy (true negatives) divided by number of negatives diagnosed in hospital (gold standard).
f The main underlying chronic maternal illnesses were, in descending order of frequency, chronic hypertension, epilepsy, renal disease, liver disease and diabetes mellitus.
b ([True positives + true negatives] ÷ 225) × 100.
Potential contributory factors
According to clinical records, 39.8% of the mothers included in the analysis had a blood haemoglobin of < 10 g/dl. During verbal autopsy, 29.3% of the mothers who were interviewed for verbal autopsy reported having been told by a health worker during an antenatal care visit that they had “less blood than normal” or anaemia.
Discussion
This is, to our knowledge, the first prospective study for the validation of the WHO verbal autopsy tool for stillbirth. Of two previous validation studies conducted on other verbal autopsy instruments, one was hospital-based and retrospective and had a lengthy recall period,11 and the other combined stillbirths with early neonatal deaths.12
Several findings have important implications for maternal and neonatal health programmes. First, over two-thirds of the stillbirths were attributable to causes for the majority of which, if not all, preventive and therapeutic interventions are available, namely pregnancy-induced hypertension, antepartum haemorrhage, underlying maternal illness and obstetric complications. Interventions targeting these conditions should be integrated into antenatal and childbirth care. Second, the similarity in the fractions of stillbirths attributed to specific causes by verbal autopsy and hospital assessment, despite an overall diagnostic accuracy of 64%, suggests that the distribution of causes of death as determined by verbal autopsy can be confidently used to plan public health interventions. Third, the diagnostic accuracy of the verbal autopsy tool for each of the five major causes of stillbirths was very high. The fraction of stillbirths attributed to a specific cause can heavily influence the size of the error for given levels of sensitivity and specificity, and if such a fraction is small (< 10%), specificity becomes more important than sensitivity in terms of the accuracy of the diagnosis made with the verbal autopsy instrument.18
Currently, most studies of stillbirth based on verbal autopsy assign a single underlying cause of death. However, some experts6 have suggested that this may not be appropriate and that multiple causes of death should be considered. When we took multiple causes into account, the sensitivity of verbal autopsy in identifying common causes of stillbirth increased from 4% to 13% at the expense of a reduction in specificity of 2–12%.
In this study, as has been reported elsewhere,12 differentiating stillbirths from neonatal deaths occurring in the first few minutes of life caused considerable difficulty. Furthermore, while the hospital obstetricians classified about one-third of the stillbirths as having occurred intrapartum, the verbal autopsy panel classified half of them as such. This possible overreporting of intrapartum stillbirths by verbal autopsy should be taken into account when producing estimates of intrapartum stillbirths based on verbal autopsy results.19
There were some noteworthy differences in the cause-specific mortality fractions resulting from verbal autopsy and clinical diagnosis. Verbal autopsy yielded a lower proportion of stillbirths assigned to more specific causes (e.g. underlying maternal illness, pregnancy-induced hypertension or specific fetal conditions) than did verbal autopsy. On the other hand, verbal autopsy tended to result in a somewhat higher prevalence of non-specific conditions, such as unexplained prematurity or asphyxia. The reason may be that more or better information was available in the hospital than was provided through recall during verbal autopsy. Nonetheless, it is remarkable that clinical assessment and verbal autopsy resulted in similar cause-specific mortality fractions for most causes of stillbirth.
This study has several strengths. First, the hospital-based causes of death were ascertained by highly-experienced obstetricians who used all available clinical and laboratory information. The diagnosis was made within 2 days of when the stillbirths occurred, when the events surrounding them were still fresh in the minds of the attending team. For consistency, the same clinical investigator ascertained the hospital-based diagnosis for all stillbirths. Second, the verbal autopsy was conducted within 2 months of the event by well trained field workers who used the standard WHO tool. Third, the causes of stillbirths determined by verbal autopsy were based on standard case definitions and a hierarchical pre-defined classification. The use of photographs of stillborns with major congenital anomalies, maceration or low birth weight may have improved families’ recall and field workers reported no negative emotional reactions to the photographs on the part of the respondents. No similar experience is available in the literature.
The study has some limitations as well. First, all the stillbirths enrolled in the study occurred in a tertiary hospital. As a result, some may argue that the results obtained may not be applicable to the general population because of potential differences in the distribution of causes between the general population and the validation sample, or because of possible differences in recall between the groups being compared. Also, interaction with health-care providers may have influenced recall later, during verbal autopsy. However, a community-based validation study cannot be conducted because of the lack of an acceptable gold standard against which to validate the verbal autopsy tool. Furthermore, in a community-based verbal autopsy study of stillbirths in Himachal Pradesh, India, 63% of the mothers had consulted a health-care provider at least once before the stillbirth, and 35% had already contacted a physician at first consultation.20 Thus, a community-based study would be susceptible to recall bias just as much as a hospital-based study. Second, we used only one method of assigning cause of death by verbal autopsy, namely a review by a panel of obstetricians. Several methods have been reported in the literature, including physician review, pre-defined computer algorithms and probabilistic models.17,19,21,22 However, the most commonly used method for interpreting verbal autopsy results is review by a panel of physicians. Third, we used clinical assessments supported by tests, including ultrasonography, instead of the final autopsy-based diagnosis to assign the hospital-based cause of death, as our objective was to assess the validity of verbal autopsy against hospital-based diagnosis.
Conducting verbal autopsy 4 to 6 weeks after the stillbirths may have introduced recall bias. However, a mourning period of at least one month should be allowed before the interviews for ethical reasons. Obviously the later the verbal autopsy is conducted, the more recall can be impaired. However, after 4 to 6 weeks there is probably less recall based on communication with hospital staff but sufficient recall of the symptoms and signs that preceded the stillbirth. In this study a panel of obstetricians assigned the causes of death after verbal autopsy using standard definitions as guidelines and a hierarchical classification. Some favour using general physicians for this purpose, as specialists may have their own preferences with respect to the specific clinical conditions.12 However, we chose obstetricians for our validation study to ensure similarity in the training and experience of those who assigned the causes of death in the hospital and after verbal autopsy in an effort to prevent reviewer bias in classifying the causes of death. We used the commonly used method of use of third reviewer to settle the disagreement among the two reviewers by agreement of two out of three. The first two reviewers agreed on the underlying cause of death in 59% of cases. We did not attempt to achieve consensus by discussion to avoid the reviewer with seniority within the organization unduly influencing the decision. Further, most differences between reviewers were related to what they chose to be the single underlying cause of death. On considering multiple causes of deaths, the differences were minimal. Classification of small for date babies could be a problem as it may not be the actual cause of death. The problem is compounded in areas with high low-birthweight rates. We therefore classified the cause of stillbirth in this case as unexplained small for date. However, it may be noted that difference in the cause specific mortality fractions between hospital and verbal autopsy is not marked.
In conclusion, the rate of stillbirths in many countries warrants the use of innovative approaches to generate information for decision-making to improve care.23 In our area there is evidence of a high stillbirth rate of around 30/1000 births.14,15 This study shows that verbal autopsy can produce reasonably good estimates of the proportionate causes of death compared with medically certified causes. Thus verbal autopsy methods and tools as used in the study can be used in settings with similar stillbirth rates. As these validation results are based on stillbirths enrolled in a hospital, care must be taken to carefully monitor the quality of verbal autopsy data from stillbirths that occur at home.
Acknowledgements
We acknowledge the technical support provided by Rajiv Bahl, a staff member of WHO, and the assignation of causes of death from the verbal autopsy questionnaires by Poonam Gupta and Rimpy Tandon, from the Department of Obstetrics and Gynaecology, Government Medical College, Chandigarh, India.
Funding:
The study was funded by the Department of Child and Adolescent Health and Development of the WHO, Geneva, Switzerland.
Competing interests:
Rajiv Bahl is a staff member of WHO, the funding source. All authors collectively decided to publish the study findings.
References
- 1.Lawn JE, Cousens S, Bhutta ZA, Darmstadt GL, Martines J, Paul V, et al. Why are 4 million newborn babies dying each year? Lancet. 2004;364:399–401. doi: 10.1016/S0140-6736(04)16783-4. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol. 2006;35:706–18. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- 3.McClure EM, Saleem S, Pasha O, Goldenberg RL. Stillbirth in developing countries: a review of causes, risk factors and prevention strategies. J Matern Fetal Neonatal Med. 2009;22:183–90. doi: 10.1080/14767050802559129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stanton C, Lawn JE, Rahman H, Wilczynska-Ketende K, Hill K. Stillbirth rates: delivering estimates in 190 countries. Lancet. 2006;367:1487–94. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]
- 5.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/BLT.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anker M, Black RE, Coldham C, Kalter HD, Quigley MA, Ross D, et al. A standard verbal autopsy method for investigating causes of death in infants and children Geneva: World Health Organization; 1999. Available from: http://www.who.int/csr/resources/publications/surveillance/WHO_CDS_CSR_ISR_99_4/en/index.html [accessed 11 November 2010]. [Google Scholar]
- 7.Baiden F, Bawah A, Biai S, Binka F, Boerma T, Byass P, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85:570–1. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benara SK, Singh P. Validity of causes of infant death by verbal autopsy. Indian J Pediatr. 1999;66:647–50. doi: 10.1007/BF02726242. [DOI] [PubMed] [Google Scholar]
- 9.Mobley CC, Boerma JT, Titus S, Lohrke B, Shangula K, Black RE. Validation study of a verbal autopsy method for causes of childhood mortality in Namibia. J Trop Pediatr. 1996;42:365–9. doi: 10.1093/tropej/42.6.365. [DOI] [PubMed] [Google Scholar]
- 10.Snow RW, Armstrong JRM, Forster D, Winstanley MT, Marsh VM, Newton CR, et al. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet. 1992;340:351–5. doi: 10.1016/0140-6736(92)91414-4. [DOI] [PubMed] [Google Scholar]
- 11.Edmond KM, Quigley MA, Zandoh C, Danso S, Hurt C, Owusu Agyei S, et al. Diagnostic accuracy of verbal autopsies in ascertaining the causes of stillbirths and neonatal deaths in rural Ghana. Paediatr Perinat Epidemiol. 2008;22:417–29. doi: 10.1111/j.1365-3016.2008.00962.x. [DOI] [PubMed] [Google Scholar]
- 12.Setel PW, Whiting DR, Hemed Y, Chandramohan D, Wolfson LJ, Alberti KG, et al. Validity of verbal autopsy procedures for determining cause of death in Tanzania. Trop Med Int Health. 2006;11:681–96. doi: 10.1111/j.1365-3156.2006.01603.x. [DOI] [PubMed] [Google Scholar]
- 13.Setel PW, Rao C, Hemed Y, Whiting DR, Yang G, Chandramohan D, et al. Core verbal autopsy procedures with comparative validation results from two countries. PLoS Med. 2006;3:e268. doi: 10.1371/journal.pmed.0030268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar R, Singhi S. Risk factors for stillbirths in a rural community. Indian J Pediatr. 1992;59:455–61. doi: 10.1007/BF02751561. [DOI] [PubMed] [Google Scholar]
- 15.Sachar RK, Soni RK. Perinatal mortality in rural Punjab – a population-based study. J Trop Pediatr. 2000;46:43–5. doi: 10.1093/tropej/46.1.43. [DOI] [PubMed] [Google Scholar]
- 16.International statistical classification of diseases and related health problems, 10th revision 2nd edition. Geneva: World Health Organization; 2005. [Google Scholar]
- 17.Winbo IG, Serenius FH, Dahlquist GG, Källén BA. NICE, a new cause of death classification for stillbirths and neonatal deaths. Neonatal and Intrauterine Death Classification according to Etiology. Int J Epidemiol. 1998;27:499–504. doi: 10.1093/ije/27.3.499. [DOI] [PubMed] [Google Scholar]
- 18.Anker M. The effect of misclassification error on reported cause-specific mortality fractions from verbal autopsy. Int J Epidemiol. 1997;26:1090–6. doi: 10.1093/ije/26.5.1090. [DOI] [PubMed] [Google Scholar]
- 19.Quigley MA, Chandramohan D, Rodrigues LC. Diagnostic accuracy of physician review, expert algorithms and data-derived algorithms in adult verbal autopsies. Int J Epidemiol. 1999;28:1081–7. doi: 10.1093/ije/28.6.1081. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal AK, Kumar R, Kumar P. Early neonatal mortality in a hilly North Indian state: socio-demographic factors and treatment seeking practices. Indian J Prev Soc Med. 2003;34:46–52. [Google Scholar]
- 21.Fantahun M, Fottrell E, Berhane Y, Wall S, Högberg U, Byass P. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84:204–10. doi: 10.2471/BLT.05.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winbo IG, Serenius FH, Dahlquist GG, Källen BA. A computer-based method for cause of death classification in stillbirths and neonatal deaths. Int J Epidemiol. 1997;26:1298–306. doi: 10.1093/ije/26.6.1298. [DOI] [PubMed] [Google Scholar]
- 23.Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. 2005;83:409–17. [PMC free article] [PubMed] [Google Scholar]