Fig. 1.
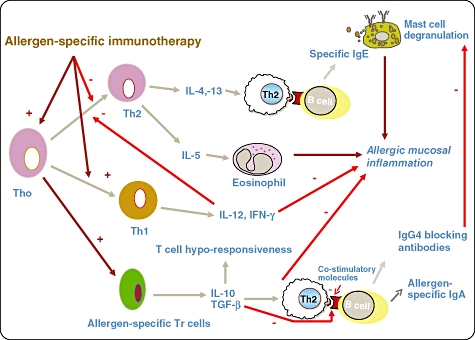
Mechanisms underlying the action of specific immunotherapy (SIT): there is T helper type 2 (Th2) predominance in allergic disease and it is characterized by secretion of interleukin (IL)-4, IL-5 and IL-13. IL-5 is involved in eosinophil survival, activation and maturation and IL-4 and IL-13 play a key role in class-switching of B cells for immunoglobulin (Ig)E production. Th1 response induces IL-12 and interferon (IFN)-γ production and this has inhibitory effects on Th2 cells. SIT up-regulates Th1 response, dampens Th2 response and induces allergen-specific Tr cells to secrete IL-10 and transforming growth factor (TGF)-β. IL-10 induces T cell ‘anergy’ or ‘unresponsiveness’ to the allergen. Allergen-specific immunotherapy induces production of allergen-specific IgG4 and IgA2, the former may play a role in interfering with allergen binding to IgE on the mast cell. The changes in Th1/Th2 balance has been shown to occur within days following initiation of ‘ultra-rush’ bee venom immunotherapy and is associated with loss of T cell responsiveness in vitro to the venom – this response is reversed by anti-IL-10 in the culture medium. A similar pattern of shift from Th2 to Th1 cytokine pattern is seen in the nasal mucosa of patients undergoing grass pollen immunotherapy and is strikingly associated with reduction of Th2 cell and eosinophil influx during the pollen season; this parallels the clinical response.
