Abstract
Objectives:
The objectives of this study were to investigate the characteristics and outcome of patients with hydatid disease of the liver who were laparoscopically managed at our clinic and to define technical details including an effective method of omentoplasty with helical fasteners.
Methods:
Between January 1998 and November 2000, 13 patients, mean age 36 years (range 23 to 63 years), with hydatid disease of the liver were considered for laparoscopic surgery in our department. All the patients underwent laparoscopic surgical interventions.
Results:
In all patients, laparoscopic cystotomy, unroofing, and omentoplasty with helical fasteners, which were originally designed for endoscopic hernia repair procedures, were performed. No conversion to laparotomy was necessary. In 1 case, with a single cyst in the right lobe, bile leakage was observed. No radiological recurrence was observed in an average follow-up of 17 months (range 4 to 36 months).
Conclusions:
Obliteration of the residual cystic cavity decreases postoperative complication rates, so an effective omentoplasty is essential especially for laparoscopic procedures. Laparoscopy is quite feasible to perform in hydatid disease of the liver, and the use of helical fasteners allows effective omental flap fixation.
Keywords: Hydatid disease, Laparoscopy, Helical fastener
INTRODUCTION
Human hydatid disease is caused by Echinococcus granulosus, a cestode that is commonly lodged in the liver. Several endemic regions exist; however, the disease may be observed anywhere in the world.1 Surgery remains the main modality of treatment, despite advances in medical and minimally invasive radiological therapies.2
In the last decade, laparoscopic surgery has become a part of the discussion of this issue, and several studies have reported encouraging results.3–5 Whatever the technique, surgeons should focus on safe evacuation and sterilization of the cyst's cavity. On the other hand, obliteration of the cavity with greater omentum has previously been reported to reduce complication rates.6 This method is a most unique way to achieve obliteration in laparoscopic procedures.
Herein, we report our series of patients with hydatid disease of the liver who underwent laparoscopic surgery, including omentoplasty and fixation of the omentum with helical fasteners.
MATERIALS AND METHODS
Between January 1998 and April 2000, 13 patients (5 men and 8 women), mean age 36 years (range 23 to 63 years) with hydatid disease of the liver were considered for laparoscopic surgery at our department. Twelve patients had single cysts, and 1 patient had two. Ten cysts were in the right lobe, and four were in the left. In the patient who had two, both of the cysts were in the right lobe. The cysts' localizations were as follows: five in segment 8, five in segment 5, three in segment 4, and one in segment 2. The average cyst's diameter was 7.2 cm. (range 4 to 12 cm). The diagnoses were made with computerized tomography (CT), ultrasonography (US), and specific serological examinations. Five patients were primarily diagnosed with US and 8 with CT. Nevertheless, CT studies were added to the first group to have an optimum morphological evaluation. No evidence or suspicion existed of biliary rupture upon clinical findings and radiological studies (history of cholangitis or jaundice, evidence of dilatation of the biliary tree, or connection with the cyst). Indirect hemagglutination tests (IHT) and ELISA tests were done as serological tests and were positive in all patients.
The patients who had evidence of biliary rupture, a history of recurrence, cysts deep or difficult to access in liver (central or posterior localizations), multiple cysts (more than two with unfavorable localizations), large cysts (>15 cm in diameter), and cysts with thick, calcified walls were not considered candidates for laparoscopy.
Operative Technique
All patients received general anesthesia. The urinary bladder was catheterized, a nasogastric tube was placed, and antibiotics were administered half an hour prior to the operation. The operation was performed with the patient in the supine position.
Pneumoperitoneum was provided by Veress needle insufflation. The first trocar was inserted at the umbilicus and a 30° laparoscope was used to visualize the peritoneal cavity. The operating surgeon stood at the patient's left side; the camera assistant managed the laparoscope from the left for right-sided cysts and from the right for left-sided cysts. Two additional 5-mm trocars were inserted from the optimum points chosen during exploration. The patient was placed in deep Trendelenburg position and the subdiaphragmatic area was filled with 200 to 300 cc of 10% povidone-iodine for right-sided cysts. The cyst then was punctured with a Veress needle and the cyst's fluid was aspirated as much as possible. The cyst was refilled with 20% hypertonic saline, which is a potent scolocidal agent and left for 5 minutes. During this procedure, a 5-mm aspirator was placed beside the puncture point to prevent any fluid spillage into the peritoneal cavity.
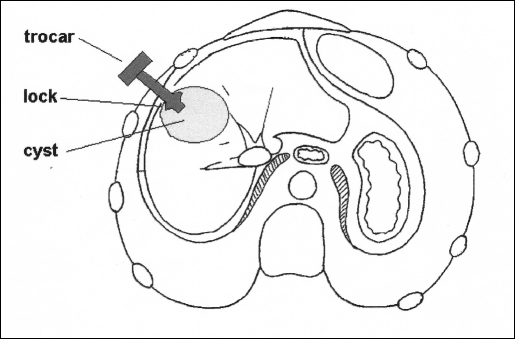
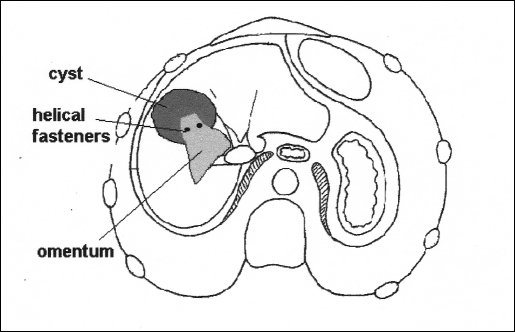
The cyst's content was reaspirated. Thereafter, a 10-mm locking trocar (Dexide Inc., Ft. Worth, Texas, USA) was inserted from a point nearest to the cyst that was immobilized with a grasper. Then this trocar, which was primarily designed to avoid inward and outward movement through the abdominal wall, was inserted into the cyst, and the umbrella-like lock was opened immediately. The cyst was pulled upwards and pinched between the abdominal wall and the umbrella lock of the trocar (Figure 1). A 10-mm aspirator was inserted through the trocar and the cyst's contents, including germinative membrane and daughter cysts, were aspirated. Irrigation with 20% saline was again performed. The superficial and visible part of the cystic wall was excised with an electrosurgical hook or shears, and the specimen was removed from the abdominal cavity within an Endobag. The cystic cavity was then explored with a laparoscope to check whether any remnants of the cyst, biliary rupture, or hemorrhage were present. An adequate portion of greater omentum was pulled and inserted into the cyst's cavity. The omentum was fixed to the cut edges of the cyst wall with a helical fastener (Pro Tack, Auto Suture, Norwalk, Connecticut, USA), an instrument designed to fix mesh patches in endoscopic hernia surgery (Figure 2). The abdominal cavity was irrigated and aspirated with saline solution. A single drain was placed into the cyst's cavity. A clear diet was allowed the next day. The drain was removed and the patient was discharged if no bile or ascites drainage were present. Albendazole was administered, 10 mg/kg/day, for 6 months postoperatively, and an intermittent therapy regimen was planned as a 4-week course of drug therapy and 2 weeks of no treatment. Radiological controls with CT and US were performed in the sixth month, and then annually.
Figure 1.
The insertion of the locking trocar into the cavity to minimize the contamination by the cyst's fluid.
Figure 2.
Schematic presentation of omentoplasty technique. Omentum is fixed at the edges of the unroofed cyst.
RESULTS
In all patients, laparoscopic cystotomy, partial cystectomy, and omentoplasty were performed. No conversion to laparotomy was necessary, and the procedures were accomplished uneventfully. The average operation time was 80 minutes (range 40 to 105 min). No perioperative complications such as bleeding occurred during application of the helical fasteners.
In 1 case, with a single cyst in the right lobe, bile leakage was observed postoperatively, whereas no evidence of biliary rupture had been found during exploration. The biliary drainage gradually tapered off and ceased spontaneously on postoperative day 9 without any further intervention. Except for this case, no early or late complications occurred.
The average hospital stay was 5 days (range 2 to 11 days). No radiological recurrence was observed in an average length of follow-up of 17 months (range 4 to 36 months).
DISCUSSION
In the last decade, laparoscopic treatment of hydatid disease of the liver has been carried out in many centers. A variety of techniques have been suggested for the surgical treatment of hydatid disease, all to sterilize the cysts, but the most commonly performed ones, both conventional or laparoscopic, are pericystectomy, simple drainage, or unroofing with omentoplasty. However, regardless of the method, the surgical principles are sterilization of the cyst cavity, careful evacuation of the cyst's content without intraperitoneal spread, investigation of the biliary rupture, and obliteration of the cyst's cavity. To succeed in laparoscopic hydatid disease surgery, these objectives are best reached with the meticulous selection of patients. As for current opinion, most laparoscopic surgeons prefer simple drainage procedures with or without partial cystectomy.3–5
Obliteration of the cyst's cavity with greater omentum has been reported to provide further benefits concerning prevention of postoperative abdominal complications.6 For this purpose, some authors have defined original omentoplasty techniques for laparoscopic hydatid disease surgery. Ertem et al5 reported an omentoplasty technique with staples. We modified it by securing an omental flap to the edges of the excised cavity with helical fasteners that are designed to fix mesh patches in video endoscopic hernia surgery. This allows a better and faster fixation of greater omentum that may easily drop into the peritoneal cavity. A critical point while applying this method is to apply fasteners only to the edges of the remnant of the cyst wall and to avoid injury to the liver. We observed no complications in our experience.
On the other hand, spread of cystic fluid into the peritoneal cavity may result in peritoneal hydatidosis. We have used a locking (or umbrella) trocar, as previously described by Seven et al,3 and a 10-mm rigid aspirator to evacuate the cyst's contents. This technique is safe and easy to apply. When approaching right-sided cysts, we filled the subdiaphragmatic space with 10% povidone-iodine (Betadine), to take measures against intraperitoneal spread, and 20% hypertonic saline solution was used to sterilize the cystic cavity. The scolocidal effect of povidone-iodine has been demonstrated in several experimental studies.7, 8 Although the use of 20% hypertonic saline solution to sterilize the cavity is now widely accepted because of it's safety and ease of application, we preferred povidone-iodine for filling the pericystic area.
In our series, except for 1 patient with 2 cysts that allowed easy access, we excluded patients with multiple cysts. Although not contraindicated, multiple cysts are not suitable for laparoscopy. In such cases, maneuver of laparoscopic devices becomes exceptionally difficult unless the surgeon uses an excessive number of ports. Also, cysts deep into the liver have increased surgical risks, such as difficult identification, bleeding, or the inability to check for biliary rupture. Khoury et al9 reported on a patient who developed anaphylaxis on laparoscopic evacuation of a hydatid cyst, localized deep into the liver. It should be kept in mind that even minimal contact of cystic fluid with blood or with the peritoneal surface may lead to anaphylactic shock, and this contact is not preventable in deep cysts. Therefore, an open surgical technique must have priority in deep cysts because the surgeon's ability to prevent cyst fluid from contact with blood is significantly more difficult.
Another question concerning difficult cases for laparoscopy is biliary rupture. In a series of 328 patients, Erguney et al10 reported a biliary rupture rate of 10.3%. In the preoperative evaluation, evidence of jaundice, right upper quadrant abdominal pain, cholangitis, or dilated biliary tract must warn the surgeon of a possible biliary rupture and a decision in favor of laparoscopic surgery should be reconsidered. One patient was overlooked on preoperative assessment in our series and presented with biliary fistula during the postoperative course. Nevertheless, biliary drainage ceased with conservative management. Spiliadis et al11 performed endoscopic sphincterotomy for complicated hydatid disease of the liver and 80% of patients suffering from postoperative biliary fistulas were successfully treated.11 Endoscopic sphincterotomy by ERCP (endoscopic retrograde cholangiopancreatography) is the treatment of choice for persistent biliary fistulas.
CONCLUSIONS
With growing experience, laparoscopy seems to be quite feasible in hydatid disease of the liver. However, laparoscopy should not limit the surgeon's performance in every surgical step of hydatid disease surgery. In many instances, omentoplasty with helical fasteners provides an easy and effective obliteration of the cyst's cavity during laparoscopic access.
References:
- 1. Ammann RW, Eckert J. Cestodes. Echinococcus. Gastroenterol Clin North Am. 1996;25:655–689 [DOI] [PubMed] [Google Scholar]
- 2. King CH. Cestodes. In: Mandell GL, Benett JE, Dolin R. eds. Principles and Practice of Infectious Diseases. 5th ed. Philadelphia, Pa: Churchill Livingstone Inc; 2000:2957–2963 [Google Scholar]
- 3. Seven R, Berber E, Mercan S, Eminoglu L, Budak D. Laparoscopic treatment of hepatic hydatid cysts. Surgery. 2000;128:36–40 [DOI] [PubMed] [Google Scholar]
- 4. Alper A, Emre A, Acarli K, Bilge O, Ozden I, Ariogul O. Laparoscopic treatment of hepatic hydatid disease. J Laparoendosc Surg. 1996;6:29–33 [DOI] [PubMed] [Google Scholar]
- 5. Ertem M, Uras C, Karahasanoglu T, Erguney S, Alemdaroglu K. Laparoscopic approach to hepatic hydatid disease. Dig Surg. 1998;15:333–336 [DOI] [PubMed] [Google Scholar]
- 6. Dziri C, Paquet JC, Hay JM, et al. Omentoplasty in the prevention of deep abdominal complications after surgery for hydatid disease of the liver: a multicenter, prospective randomized trial. French Associations for Surgical Research. J Am Coll Surg. 1999;188:281–289 [DOI] [PubMed] [Google Scholar]
- 7. Gokce O, Yilmaz M, Huseyinoglu K, Gunel S. Povidone-iodine in experimental peritoneal hydatidosis. Br J Surg. 1991;78:495–496 [DOI] [PubMed] [Google Scholar]
- 8. Besim H, Karayalcin K, Hamamci O, Gungor C, Korkmaz A. Scolecoidal agents in hydatid cyst surgery. HPB Surg. 1998;10:347–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khoury G, Jabbour-Khoury S, Soueidi A, Nabbout G, Baraka A. Anaphylactic shock complicating laparoscopic treatment of hydatid cysts of the liver. Surg Endosc. 1998;12:452–454 [DOI] [PubMed] [Google Scholar]
- 10. Erguney S, Tortum O, Taspinar AH, Ertem M, Gazioglu E. Complicated hydatid cysts of the liver. Ann Chir. 1991;45:584–589 [PubMed] [Google Scholar]
- 11. Spiliadis C, Georgopoulos S, Dailianas A, Konstantinidis A, Rimikis M, Skandalis N. The use of ERCP in the study of patients with hepatic echinococcosis before and after surgical intervention. Gastrointest Endosc. 1996;43:575–579 [DOI] [PubMed] [Google Scholar]