Abstract
PURPOSE Current office blood pressure measurement (OBPM) is often not executed according to guidelines and cannot prevent the white-coat effect. Serial, automated, oscillometric OBPM has the potential to overcome both these problems. We therefore developed a 30-minute OBPM method that we compared with daytime ambulatory blood pressure.
METHODS Patients referred to a primary care diagnostic center for 24-hour ambulatory blood pressure monitoring (ABPM) had their blood pressure measured using the same validated ABPM device for both ABPM and 30-minute OBPMs. During 30-minute OBPM, blood pressure was measured automatically every 5 minutes with the patient sitting alone in a quiet room. The mean 30-minute OBPM (based on t = 5 to t = 30 minutes) was compared with mean daytime ABPM using paired t tests and the approach described by Bland and Altman on method comparison.
RESULTS We analyzed data from 84 patients (mean age 57 years; 61% female). Systolic and diastolic blood pressures differed from 0 to 2 mm Hg (95% confidence interval, −2 to 2 mm Hg and from 0 to 3 mm Hg) between mean 30-minute OBPM and daytime ABPM, respectively. The limits of agreement were between −19 and 19 mm Hg for systolic and −10 and 13 mm Hg for diastolic blood pressures. Both 30-minute OBPM and daytime ABPM classified normotension, white-coat hypertension, masked hypertension, and sustained hypertension equally.
CONCLUSIONS The 30-minute OBPM appears to agree well with daytime ABPM and has the potential to detect white-coat and masked hypertension. This finding makes 30-minute OBPM a promising new method to determine blood pressure during diagnosis and follow-up of patients with elevated blood pressures.
Keywords: Blood pressure, family practice, diagnosis
INTRODUCTION
The Framingham and the SCORE (systematic coronary risk evaluation) risk functions, both developed to assess the risk of cardiovascular disease, are based on standardized office blood pressure measurements (OBPMs).1,2 Despite guidelines that advocate the relevance of well-executed, standardized OBPM to prevent several forms of bias,3,4 it is well known that most caregivers do not execute OBPM strictly according to these guidelines.5,6 In addition, up to one-quarter of patients is prone to the white-coat effect (in which patients exhibit elevated blood pressure in a clinical setting but not in other settings), which influences cardiovascular risk profiling as well.7,8 This white-coat effect cannot be overcome by standardized OBPM. As a consequence, the determined cardiovascular risk will be incorrect in an estimated 25% of patients and may lead to under- or overtreatment.
To enable a more precise determination of cardiovascular risk, OBPM should be free from (observer) bias and the white-coat effect. The measurement should be uniform, easy to execute correctly for all types of health care personnel (doctors, practice assistants, practice nurses, research assistants, etc), and straightforward to implement in daily practice.
Fortunately, since the introduction of automated, oscillometric blood pressure measurement devices, this ideal can be met. Oscillometric devices are readily available in primary care and are used for 24-hour ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring.1,3 Guidelines have started to recommend the use of 24-hour ABPM and home blood pressure monitoring primarily for the detection of the white-coat effect.1,4
Although both these types of monitoring eliminate most types of observer bias and the white-coat effect, 24-hour ABPM is costly and not suitable for all types of patients; up to 50% of patients report it is a nuisance or results in disturbed sleep.9 With home blood pressure monitoring, patients are reported to be noncompliant with measurements or self-report of blood pressures.10
There is a small but growing body of evidence to support a new method of office measurements in which a series of automated measurements is taken with the patient sitting alone in a quiet room (serial automated OBPM). The scarce, available research comes predominantly from one research group that used a validated oscillometric office blood pressure device able to be set at measurement intervals of 1 minute or more for a duration of 5 to 10 minutes. With this protocol the white-coat effect was practically eliminated.11,12
Meanwhile we developed a protocol that enables practices or primary care diagnostic centers to use a 24-hour ABPM device for serial automated OBPM. To our knowledge no previous research has studied using this protocol.
A growing number of practices and diagnostic centers already possess 1 or more 24-hour ABPM devices. Using a 24-hour ABPM device for serial automated OBPM can be cost saving, and the device is user friendly, as clinic staff are already familiar with it. Validating our protocol may contribute to further acceptance of serial automated OBPM.
As a first step in the process of validation, using a study sample of patients drawn from a family medicine population, we compared blood pressures determined using a protocol of serial measurements while patients were sitting for a mean of 30 minutes (30-minute OBPM) with their mean daytime ABPMs.
METHODS
Design, Setting, and Participants
We invited all patients aged 18 years or older who were referred by their family physician from October 2008 until February 2009 for a 24-hour ABPM to a diagnostic center that primarily supports family practices to participate in this comparative study. Reasons for referral were obtained from routinely used referral forms.
Known atrial fibrillation, irregular pulse, pregnancy, and night shift work were exclusion criteria. After informed consent a 30-minute OBPM took place directly before a 24-hour ABPM.
Ethics approval was not required, as declared by the local Medical Ethics Committee of the RUNMC (Central Committee on Research involving Human Subjects, Arnhem-Nijmegen, the Netherlands).
Blood Pressure Monitors and Measurements
A Welch Allyn Cardioperfect 6100 oscillometric blood measurement device (Welch Allyn Protocols, Inc, New York, New York) was used for both the 30-minute OBPM and the 24-hour ABPM. This device is equivalent to the validated SunTech Medical Oscar 2 device (SunTech Medical, Inc, Morrisville, North Carolina, and Eynshm, Oxfordshire, England; declaration of equivalence form13 available upon request).14 For each patient, the same device was used for both measurements. The devices are calibrated annually.
All 30-minute measurements took place between 11 am and 3 pm in a quiet room at the diagnostic center. The patient was sitting still 5 minutes before and during the 30-minute OBPM. The patient sat in a chair with a supported back, arm at heart level, and both feet resting flat on the floor. Blood pressure was measured on the nondominant arm at 5-minute intervals for a total of 8 measurements. The first measurement was a test measurement during the installation of the patient. The second measurement was the start of the 30-minute period; the researcher (I.E.B.) left the room after this measurement proved to be successful (no error reading).
Previous research has shown that in serial measurements blood pressure can decline substantially in the first 10 minutes before it stabilizes.15,16 We therefore chose to exclude the first 2 measurements for the determination of the mean 30-minute OBPM. Thus we define 30-minute OBPM to be the mean blood pressure calculated from the 6 measurements taken at 5-minute intervals from t = 5 to t = 30 minutes. If more than 1 of these 6 measurements was erroneous (defined as an “error” reading given by the device), the entire case was excluded for analysis.
To underpin our choice for a 30-minute period of measurements, we compared the mean 30-minute OBPM with the means of several shorter time periods, using the acquired data on 30-minute OBPM and recalculated these data to means based on 2 to 5 measurements. We then compared these means with the mean 30-minute OBPM using paired t tests.
The 24-hour ABPM was set at 20-minute intervals from 7 am to 11 pm and at 1-hour intervals from 11 pm to 7 am. Blood pressure was monitored on the same arm as during the 30-minute OBPM. Patients were instructed to perform their usual daily activities but to stop moving and be silent during measurements. The mean daytime ABPM was calculated from the readings of 9 am to 9 pm.3 Only patients with 15 or more successful daytime readings were included.
Patient instructions and application of the monitors were performed by the same experienced researcher (I.E.B.), trained in the procedures of blood pressure measurement, using a standardized protocol based on the American Heart Association guidelines.4
Classification of Hypertension Subtype
As an indication for the diagnostic value, we compared the 30-minute OBPM with the daytime ABPM in classifying 4 groups of blood pressure subtypes: normotension (office blood pressure <140/90 mm Hg and daytime ABPM or 30-minute OBPM <135/85 mm Hg); white-coat hypertension (office blood pressure ≥140/90 mm Hg and daytime ABPM or 30-minute OBPM <135/85 mm Hg); masked hypertension (office blood pressure <140/90 mm Hg and daytime ABPM or 30-minute OBPM ≥135/85 mm Hg), and sustained hypertension (office blood pressure ≥140/90 mm Hg and daytime ABPM or 30-minute OBPM ≥135/85 mm Hg). In the absence of usual care office blood pressure measurements, we defined office blood pressure as the mean of the first 2 measurements of the 30-minute OBPM.
Sample Size
In the absence of international consensus criteria, we deemed a mean difference of 5 or more mm Hg between both types of measurements in the same patient to be of clinical relevance. Detection of blood pressure differences smaller than 5 mm Hg is seriously hampered by the biologic variation of blood pressure.17,18 With a 2-sided α of .05, a power of 90%, and a standard deviation of the difference of 15 mm Hg, a sample size of 81 would allow detection of a difference of 5 mm Hg or more.
Statistical Analysis
We calculated the difference between the mean daytime ABPM and the mean 30-minute blood pressure, as well as the standard deviation of the difference. Results are presented for systolic and diastolic blood pressure and for mean arterial pressure. Although mean arterial pressure is not a measure commonly used in primary care, we present it because it is measured by oscillometric devices to calculate the values of the systolic and diastolic blood pressure. The means of the daytime ABPM and the 30-minute blood pressures were compared using a paired t test. Bland-Altman plots were constructed to further evaluate agreement of both means.
The limits of agreement in these plots were derived from the standard deviation of the mean difference between both measurements using the following formula: mean difference ± 1.96 × standard deviation of the mean difference.19
Pearson’s correlation was determined to study whether a difference between the means would relate to the magnitude of the blood pressure. Log transformation would be applied in case of dependence.20
We applied McNemar-Bowker test to determine whether the same patients who were categorized by 30-minute OBPM into 1 of the 4 subgroups of the hypertension classification were similarly categorized by the mean daytime ABPM.
We used the SPSS version 14.0 software package (SPSS Inc, Chicago, Illinois) for all analyses.
RESULTS
Of 117 patients asked to participate, 18 patients declined, and 3 patients were excluded (2 with known atrial fibrillation, and 1 with irregular pulse at examination). Of 96 patients included, 6 measurements exceeded the predefined number of erroneous readings; in 5 patients a problem occurred with cuff fitting during the 24-hour ABPM, and 1 patient was disturbed during the 30-minute OBPM, leaving 84 patients for the final analysis. The characteristics of these patients are shown in Table 1▶.
Table 1.
Characteristics of Study Population
| Variable | Value |
|---|---|
| Population studied, No. | 84 |
| Age, mean (SD), y | 57 (13.9) |
| Sex, % | |
| Female | 61 |
| Male | 39 |
| Body mass index, mean (SD) | 26.5 (4.3) |
| Smoker, % | 17 |
| Antihypertensive medication, % | |
| Yes | 51 |
| No | 49 |
| Reason of referral for 24-hr ABPM, % | |
| Suspected white-coat hypertension | 45 |
| Diagnosis of hypertension | 38 |
| Treatment evaluation | 12 |
| Other | 5 |
ABPM = 24-hour ambulatory blood pressure monitoring.
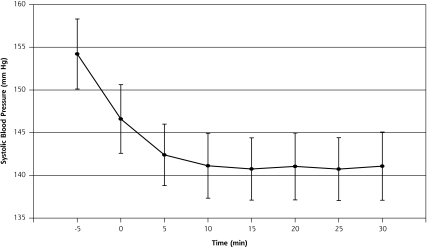
Figure 1▶ shows that systolic blood pressure declines substantially in the first 15 minutes before reaching a plateau phase. We observed exactly the same course for diastolic blood pressure (data not shown). The mean 10-minute OBPM (mean of third and fourth measurements) is modestly but not significantly higher than the mean 30-minute OBPM (142/84 mm Hg vs 141/84 mm Hg; P = .1 and .7, respectively). No differences were found for mean 15-, 20-, and 25-minute OBPMs compared with the mean 30-minute OBPM.
Figure 1.
Course of mean systolic blood pressure during 30 minutes of measurement.
Note: Error bars represent 95% confidence intervals of the standard error of the mean.
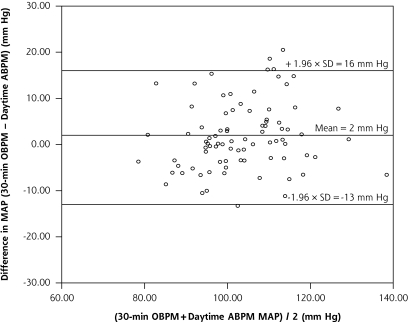
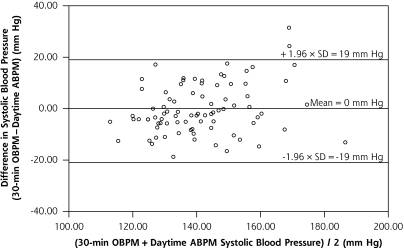
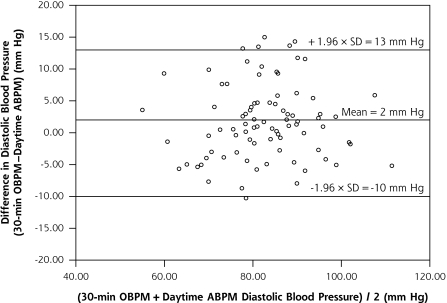
The mean blood pressure levels, the difference between the means, and the standard deviation of the difference of the daytime ABPM and the 30-minute blood pressure levels are depicted in Table 2▶. The limits of agreement were between −19 and 19 mm Hg for systolic blood pressure, between −10 and 13 mm Hg for diastolic blood pressure, and between −13 and 16 mm Hg for mean arterial pressure.
Table 2.
Blood Pressure Levels for Daytime ABPM and 30-Minute OBPM
| Measurement | 30-min OBPM (SD) | Daytime ABPM (SD) | Δ 30-min OBPM–ABPM (95% CI) | SDD |
|---|---|---|---|---|
| Mean arterial pressure, mm Hg | 104 (12) | 103 (11) | 2 (0 to 3)a | 7 |
| Systolic blood pressure, mm Hg | 141 (17) | 141 (14) | 0 (−2 to 2) | 10 |
| Diastolic blood pressure, mm Hg | 84 (11) | 82 (11) | 2 (0 to 3)b | 6 |
ABPM = ambulatory blood pressure monitoring; CI = confidence interval; OBPM = office blood pressure measurement; SDD = standard deviation of the difference of the mean.
Note: Because of rounding, figures may not add up correctly.
aP=.03.
bP=.008.
Figures 2a▶, 2b▶, and 2c▶ plot the difference between the 30-minute OBPM and the daytime ABPM against mean blood pressure. The difference proved to be related to the magnitude of the mean blood pressure for systolic blood pressure, but not for mean arterial pressure and diastolic blood pressure (Pearson correlation coefficient r = 0.27, P = .01; r = 0.17, P = .13; and r = 0.05, P = .64, respectively).
Figure 2a.
Bland-Altman plot of difference in mean arterial pressure between 30-minute OBPM and daytime ABPM against mean mean arterial pressure.
ABPM = 24-hour ambulatory blood pressure monitoring; MAP = mean arterial pressure; OBPM = office blood pressure measurement.
Figure 2b.
Bland-Altman plot of difference in systolic blood pressure between 30-minute OBPM and daytime ABPM against mean systolic blood pressure.
ABPM = 24-hour ambulatory blood pressure monitoring; OBPM = office blood pressure measurement.
Figure 2c.
Bland-Altman plot of difference in diastolic blood pressure between 30-minute OBPM and daytime ABPM against mean diastolic blood pressure.
ABPM = 24-hour ambulatory blood pressure monitoring; OBPM = office blood pressure measurement.
As shown in Table 3▶, the 30-minute OBPM classified patients into the 4 subgroups of hypertension (as mentioned in the method section) similarly to daytime ABPM. There was no significant difference in classification of patients between both measurements (P = .22); 87% of patients were classified similarly.
Table 3.
Comparison of Patients Classified by Hypertension Subtypes Between 30-Minute OBPM and Daytime ABPM
| Subtype | 30-min OBPM No. | Daytime ABPM No. |
|---|---|---|
| Normotensive | 18 | 15 |
| White-coat hypertension | 13 | 13 |
| Masked hypertension | 1 | 4 |
| Sustained hypertension | 52 | 52 |
ABPM = ambulatory blood pressure monitoring; OBPM = office blood pressure measurement.
Note: There were 87% of patients similarly classified by both 30-minute OBPM and daytime ABPM.
DISCUSSION
We have reported a difference of less than 2 mm Hg, with a standard deviation of the difference of less than 10 mm Hg for mean arterial pressure and systolic and diastolic blood pressure of the mean 30-minute OBPM compared with the mean daytime ABPM using the same blood pressure monitoring device for both types of measurement. The limits of agreement were comparable to other blood pressure method comparison studies. In addition, 30-minute OBPM seems to be able to detect white-coat hypertension as well as daytime ABPM does.
Our Results in Perspective of Previous Research
Although in our study no clinical relevant systematic difference was detected between 30-minute OBPM and daytime ABPM, the limits of agreement show that at the individual level, substantial, clinical relevant differences can occur (Figures 2a▶-c▶). Ideally in comparative studies the reference measurement has an excellent reproducibility.20 In blood pressure measurement, however, this reproducibility is always limited by the relatively large intrapersonal biologic variation of blood pressure. Consequently, any comparative study on blood pressure measurements will result in relatively wide limits of agreement. The limits of agreement in our study did not exceed even those of well-executed reproducibility studies (eg, with 24-hour ABPM).18,21
Accordingly, 30-minute blood pressure readings are preferred to other types of office-based blood pressure measurements.22 Although it is known that conventional OBPMs executed in complete accordance with guidelines may reach results similar to those of ABPMs,23 daily practice over the last decades has proved that one can be skeptical about ever bridging the gap between theory and daily practice.
No previous studies have aimed at comparing mean 30-minute blood pressures with mean daytime ambulatory blood pressure in a primary care setting using the same measurement device for both types of measurement. There has been some research showing that mean 4- to 10-hour blood pressure was comparable to mean daytime ambulatory blood pressure.24,25 In a recent study, Culleton et al reported on the use of a mean 25-minute (4-minute interval) oscillometric blood pressure measurement to reduce white-coat effect.26 Mean 25-minute blood pressure appeared to be 10 mm Hg lower than daytime ABPM. Differences, however, in the primary objective of the study, the study population, and the period of rest before start of measurement obstruct reasonable comparison with our results.
Our results are in agreement with data from Myers et al, where the automated office measurement proved to be 2 mm Hg lower than daytime ABPM.12 Their study population was almost similar to ours, but their blood pressure measurement protocol differed considerably (5 or 10 minutes, apparently without a prior rest period). In contrast to Myers et al, we used 1 device for both the office and the ambulatory measurement. In this way, we excluded a potential source of bias when comparing the 2 measurement methods. We purposely chose to validate a protocol with the use of an ABPM device because we anticipate that in most industrialized countries these devices will soon become standard equipment in family physicians’ offices. With the 30-minute protocol, practices can than use 1 type of device (and 1 type of software) for both office and ambulatory measurements. The 5-minute measurement interval in our protocol was chosen because the minimum measurement interval of most, if not all, ambulatory devices can be set at least at 5 minutes. As a consequence, with the same number of measurements, this minimum interval results in a longer measurement period than the 10 minutes studied by Myers et al. Our results showed, however, that serial measurements for 10 minutes after a 5- to 10-minute rest period may be sufficient; future research is needed to underline this possibility.
Strengths and Limitations
Our study has several strengths. It was performed in a primary care setting—the setting where high blood pressure is most often diagnosed and managed. Blood pressure measurements were executed according to clear and well-described protocols that can be easily implemented in daily practice using existing blood pressure measurement devices.
For logistic reasons we were unable to randomize the order in which 30-minute OBPM and ABPM took place. As a consequence, a regression to the mean could have influenced the results of our study. The 30-minute OBPM, however, was not used as a selection criterion to undergo 24-hour ABPM, and the mean 30-minute measurement was determined excluding the first measurement.
Our definition of a successful daytime ABPM was more lenient than the consensus-based definitions of most guidelines. To understand whether this discrepancy would influence results, we reanalyzed our data from 64 patients using the cutoff as defined by O’Brien et al3 and found the results to be consistent with those reported here (data not shown).
The study population consisted of hypertensive patients in usual care family practice, some of whom were taking antihypertensive medications. Although in theory treatment for hypertension may have had an effect on the study outcome, in their method comparison study, Little et al found that, in a family practice–based population, treatment does not bias results.22
The mean difference between 30-minute OBPM and daytime ABPM was related to the magnitude of the blood pressure. This relation is common in blood pressure research, and if this relation is strong, it seems reasonable to report conclusions separately for both hypertensive and normotensive patients. In our study, however, the observed correlations were very small and do not affect our conclusions.
We realize that the outcome of our study depends in part on the population under study, its sample size, and the setting. For instance, that our 30-minute OBPM was executed in a single primary care diagnostic center rather than in actual family practices may have affected the results, because of a potential difference in white-coat effect between settings. Recently, however, Ogedegbe et al showed that although setting can be a factor, the role of the physician is most relevant.27
Future Perspectives
Currently, detection of the white-coat effect is the main and most evidence-based indication for the use of 24-hour ABPM or home blood pressure monitoring, and guidelines formulate with caution about other possible indications.1,3–4 We believe that automated OBPM—such as the 30-minute OBPM—is a valid, useful, office-based alternative to daytime ABPM or home blood pressure monitoring for this indication. Moreover and contrary to the more laborious home blood pressure monitoring and 24-hour ABPM, 30-minute OBPM could be a convenient way to follow up high blood pressure findings.
Although 30-minute OBPM and home blood pressure monitoring are theoretically interchangeable with regard to indication and interpretation, the same cannot be said for 24-hour ABPM. Twenty-four hour monitoring gives unique information about the diurnal blood pressure pattern (dipping or nondipping), blood pressure variability, and mean night blood pressure. It is unclear, however, whether these data can be used to improve cardiovascular risk management, and if so, how these variables should be used and interpreted in family medicine.
Improvement of office measurement techniques can already benefit patients substantially, particularly in family medicine. Very recently an algorithm has been proposed for diagnosing hypertension using serial automated OBPM.24
The 30-minute OBPM agrees well with daytime ABPM and has limits of agreement comparable to other method comparison studies of blood pressure. It appears to classify blood pressure status of patients as well as daytime ABPM. Accordingly, this new method of office blood pressure measurement can potentially enable family physicians to overcome well-known problems when measuring usual blood pressure, such as observer bias and the white-coat effect. Additional research is needed to determine the reproducibility of the 30-minute OBPM and its agreement with usual office and home-based blood pressure measurements.
Acknowledgments
We would like to thank the primary care based diagnostic center Stichting Huisartsenlaboratorium Oost (location Velp) for their help in data acquisition.
Conflicts of interest: Carel Bakx and Mark van der Wel collaborate in a research project aiming at improvement of hypertension management (NAMI-study, http://www.clinicaltrials.gov: NCT00457483) with an unconditional grant by Novartis to cover the material costs of the study. As head of the Department of Primary and Community Care, Chris van Weel supervises research projects some of which (in part) are funded as unconditional research grants by Bayer, NovoNordisk, Astra-Zeneca, Boehringer Ingelheim, GlaxoSmithKline, or Novartis. Iris Buunk and Theo Thien report no conflicts of interest.
Funding support: This study was funded by the Department of Primary and Community Care, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands.
REFERENCES
- 1.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. [DOI] [PubMed] [Google Scholar]
- 2.Conroy RM, Pyörälä K, Fitzgerald AP, et al.; SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003. [DOI] [PubMed] [Google Scholar]
- 3.O’Brien E, Asmar R, Beilin L, et al.; European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21(5):821–848. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. [DOI] [PubMed] [Google Scholar]
- 5.Graves JW, Sheps SG. Does evidence-based medicine suggest that physicians should not be measuring blood pressure in the hypertensive patient? Am J Hypertens. 2004;17(4):354–360. [DOI] [PubMed] [Google Scholar]
- 6.Campbell NR, Culleton BW, McKay DW. Misclassification of blood pressure by usual measurement in ambulatory physician practices. Am J Hypertens. 2005;18(12 Pt 1):1522–1527. [DOI] [PubMed] [Google Scholar]
- 7.Myers MG, Oh PI, Reeves RA, Joyner CD. Prevalence of white coat effect in treated hypertensive patients in the community. Am J Hypertens. 1995;8(6):591–597. [DOI] [PubMed] [Google Scholar]
- 8.Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988;259(2): 225–228. [PubMed] [Google Scholar]
- 9.Verdecchia P, Angeli F, Borgioni C, Gattobigio R, Reboldi G. Ambulatory blood pressure and cardiovascular outcome in relation to perceived sleep deprivation. Hypertension. 2007;49(4):777–783. [DOI] [PubMed] [Google Scholar]
- 10.van der Hoeven NV, van den Born B-JH, Cammenga M, van Montfrans GA. Poor adherence to home blood pressure measurement schedule. J Hypertens. 2009;27(2):275–279. [DOI] [PubMed] [Google Scholar]
- 11.Myers MG, Valdivieso M, Kiss A. Optimum frequency of office blood pressure measurement using an automated sphygmomanometer. Blood Press Monit. 2008;13(6):333–338. [DOI] [PubMed] [Google Scholar]
- 12.Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009;27(2):280–286. [DOI] [PubMed] [Google Scholar]
- 13.Atkins N, O’Brien E. The dabl Educational Trust device equivalence procedure. Blood Press Monit. 2007;12(4):246–249. [DOI] [PubMed] [Google Scholar]
- 14.Goodwin J, Bilous M, Winship S, Finn P, Jones SC. Validation of the Oscar 2 oscillometric 24-h ambulatory blood pressure monitor according to the British Hypertension Society protocol. Blood Press Monit. 2007;12(2):113–117. [DOI] [PubMed] [Google Scholar]
- 15.Sala C, Santin E, Rescaldani M, Magrini F. How long shall the patient rest before clinic blood pressure measurement? Am J Hypertens. 2006;19(7):713–717. [DOI] [PubMed] [Google Scholar]
- 16.Netea RT, Thien T. Blood pressure measurement: we should all do it better! Neth J Med. 2004;62(8):297–303. [PubMed] [Google Scholar]
- 17.Mancia G, Ferrari A, Gregorini L, et al. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ Res. 1983;53(1):96–104. [DOI] [PubMed] [Google Scholar]
- 18.Stergiou GS, Baibas NM, Gantzarou AP, et al. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002;15(2 Pt 1):101–104. [DOI] [PubMed] [Google Scholar]
- 19.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1(8476):307–310. [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. [DOI] [PubMed] [Google Scholar]
- 21.Palatini P, Mormino P, Canali C, et al. Factors affecting ambulatory blood pressure reproducibility. Results of the HARVEST Trial. Hypertension and Ambulatory Recording Venetia Study. Hypertension. 1994;23(2):211–216. [DOI] [PubMed] [Google Scholar]
- 22.Little P, Barnett J, Barnsley L, Marjoram J, Fitzgerald-Barron A, Mant D. Comparison of agreement between different measures of blood pressure in primary care and daytime ambulatory blood pressure. BMJ. 2002;325(7358):254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jula A, Puukka P, Karanko H. Multiple clinic and home blood pressure measurements versus ambulatory blood pressure monitoring. Hypertension. 1999;34(2):261–266. [DOI] [PubMed] [Google Scholar]
- 24.Sheps SG, Bailey KR, Zachariah PK. Short-term (six hour), ambulatory blood pressure monitoring. J Hum Hypertens. 1994;8(12):873–878. [PubMed] [Google Scholar]
- 25.Wong RC, Yeo TC. ‘Office-hour’ ambulatory blood pressure monitoring is sufficient for blood pressure diagnosis. J Hum Hypertens. 2006;20(6):440–443. [DOI] [PubMed] [Google Scholar]
- 26.Culleton BF, McKay DW, Campbell NR. Performance of the automated BpTRU measurement device in the assessment of white-coat hypertension and white-coat effect. Blood Press Monit. 2006;11(1): 37–42. [DOI] [PubMed] [Google Scholar]
- 27.Ogedegbe G, Pickering TG, Clemow L, et al. The misdiagnosis of hypertension: the role of patient anxiety. Arch Intern Med. 2008; 168(22):2459–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myers MG. A proposed algorithm for diagnosing hypertension using automated office blood pressure measurement. J Hypertens. 2010;28(4):703–708. [DOI] [PubMed] [Google Scholar]