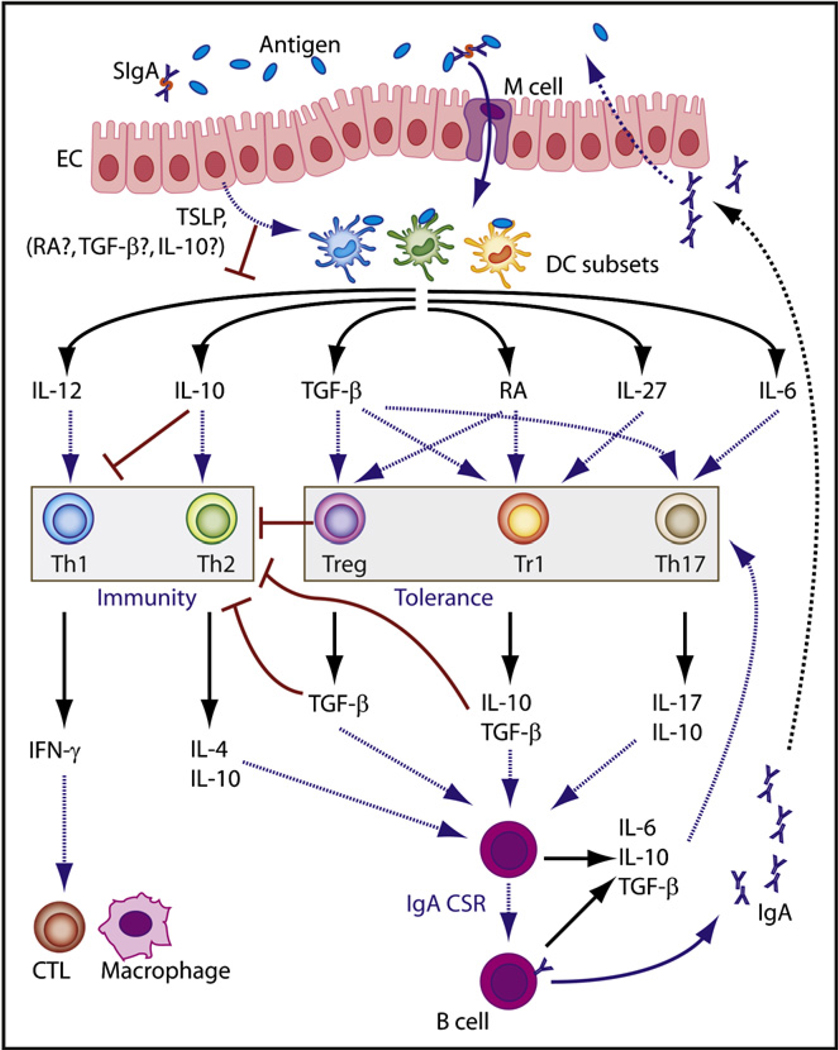
Figure 2. Putative Role of IgA in Intestinal Tolerance and Homeostasis.
Intestinal M cells transfer IgA-bound antigen from the lumen to DCs. In the presence of TSLP and other epithelial cell (EC) products, possibly including retinoic acid (RA), TGF-β, and IL-10, multiple subsets of Peyer’s patch DCs initiate noninflammatory CD4+ T cell responses. By blocking DC production of IL-12 and inducing DC production of IL-10, TSLP prevents intestinal DCs from initiating proinflammatory Th1 responses, including IFN-γ-dependent activation of macrophages and cytotoxic T lymphocytes (CTLs). The resulting Th2 response triggers IgA (and IgG) class switching and production by activating B cells via CD40L (not shown) as well as IL-4 and IL-10. By upregulating DC release of TGF-β, IL-6, IL-27, and RA, TSLP alone or combined with other epithelial factors might also initiate Treg, Tr1, and Th17 cell responses. Treg cells dampen Th1-Th2 immunity through contact-dependent mechanisms and TGF-β, whereas Tr1 cells and regulatory-stage Th17 cells attenuate Th1-Th2 immunity via IL-10. Treg, Tr1, and Th17 cells might also trigger IgA (but not IgG) class switching and production by activating B cells via CD40L (not shown) as well as TGF-β and IL-10. Intestinal Treg, Tr1, and Th17 cell responses might be further amplified by TGF-β, IL-10, IL-6, and IgA derived from B cells.