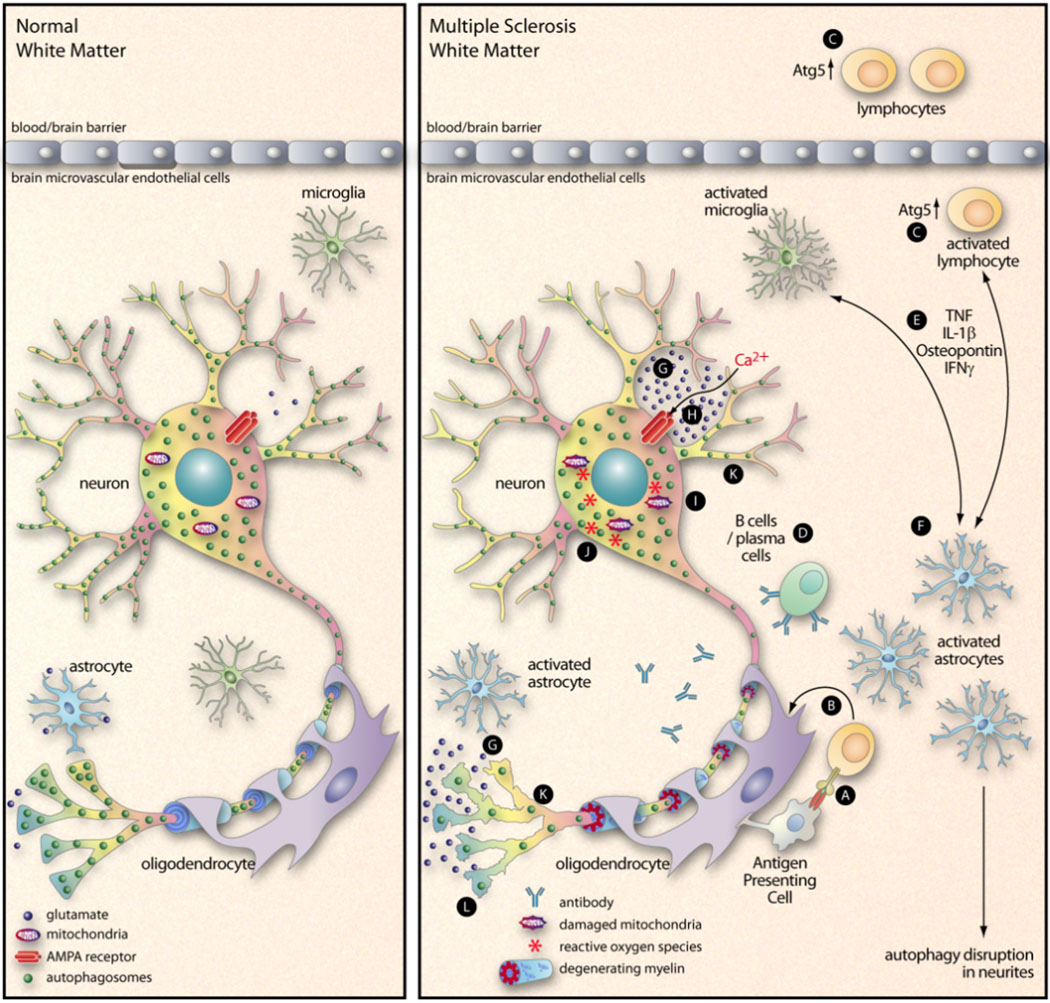
Figure 2. Proposed interactions between inflammation, Ca2+ excitotoxicity, and autophagy in a non-infectious neurodegenerative disease.
During MS, lymphocytes infiltrate into the brain and recognize their antigen, usually myelin-derived antigen presented by an APC (A). These activated T cells then release pro-inflammatory cytokines that act on oligodendrocytes (B), leading to the demyelination that is a hallmark of the disease. This diagram focuses mainly on other events that may be involved in MS neurodegeneration. Atg5 is an important component of the autophagy pathway, and its cleavage can switch a cell’s fate from autophagy (and survival) to apoptosis (and death) (Yousefi et al., 2006). In our recent paper (Alirezaei et al., 2009) we showed that peripheral blood CD4+ T cells of some MS patients contained an elevated level of Atg5, leading us to speculate that these potentially-pathogenic cells may have prolonged lifespans (C). B cells and plasma cells, too, have been implicated in MS (D). The pro-inflammatory mediators that are released by activated lymphocytes and / or microglia (E) can activate astrocytes (F), reducing their capacity of resorb glutamate (G). The resulting increase in extracellular glutamate triggers AMPA receptors (H) which leads to an influx of Ca2+ into the neurons (Williams et al., 2008). This initiates a cascade of events including damage to mitochondria (I), an increase in ROS (J), activation of caspases and calpain, and a decrease in number of neurite autophagosomes (K). The ultimate outcome is neurodegeneration (L).