Figure 5. Conceptual model showing the contribution of optimal individual behaviour and the risk of premature death or disability from any cause and the contribution of genetics to this increased risk.
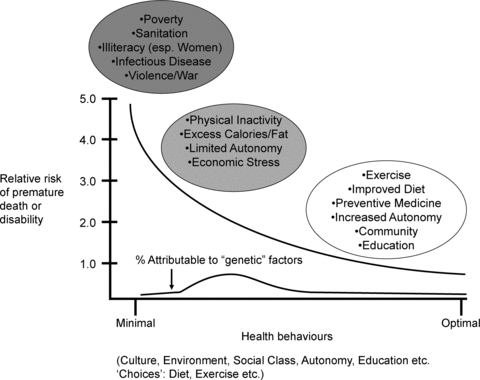
Individual behaviour is influenced by complex interactions among culture, environment, social class, education, and ‘choices’ about things like diet, exercise and seat belt use. In chaotic societies with uncertain food supplies, poor sanitation, no social safety net and warfare or other forms of social displacement, premature death and disability is vastly greater than in more stable environments. Additionally, under these desperate conditions we speculate that genetic variation in individual humans contributes minimally to the pattern of death and disability. At the other end of the spectrum are educated, well-off individuals of high social status who typically engage positive health behaviours. We speculate that these individuals are largely buffered from potentially adverse genetic variants. By contrast are the inactive, obese citizens of many industrialized nations who have limited social autonomy and consistently engage in negative health behaviours. These behaviours and social factors may then interact with certain genetic variants to facilitate the emergence of many diseases such as diabetes, hypertension, cancer and vascular disease. Thus, we speculate that for a given individual a low physical activity, high calorie, high social stress lifestyle determines the extent that various ‘risk’ gene variants for metabolic, cardiovascular and other diseases become expressed or activated. This concept is also demonstrated in Fig. 3. As these interactions are likely to be complex and involve a large number of genetic variants, as shown in Fig. 1, the utility of predictive models based on genetic information is likely to be limited.
