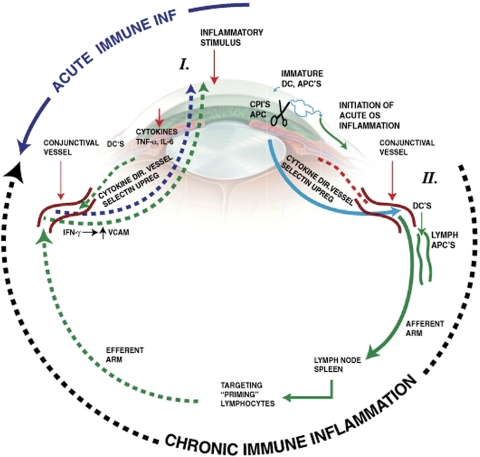
Figure 4.
Diagram of acute and chronic ocular immune inflammation. Acute inflammation is initiated by associated tissue damage and by a naïve cellular immune response through immature antigen presenting cells in the eye. This results in the subsequent recruitment of acute-phase inflammation cells from the conjunctival and episcleral blood vessels. In contrast, chronic immune inflammation involves procurement and processing of antigens by mature antigen presenting cells in the eye that migrate to the local afferent arm of the lymph drainage system in the conjunctiva, where antigen-APCs drain into regional lymph nodes and the spleen. This then results in a primed T-cell response that migrates out of the lymph system back into the eye via the blood vessels in the eye, including conjunctival and episcleral blood vessels. The cells adhere to vascular endothelium and enter the tissue through diapedesis. APCs indicate antigen presenting cells; CPIs, corneal proteases; DC, dendritic cells; TNF-α, tumor necrosis factor alpha; IL-6, interleukin 6; IFN-γ, interferon gamma. Reprinted with permission from McDermott AM, Perez V, Huang AJW, et al. Pathways of corneal and ocular surface inflammation: a perspective from the Cullen symposium. Ocul Surf. 2005;3:S131–S138. Artist: Elaine Kurie.