Abstract
We review the records of 79 tetanus patients in two hospitals (one tertiary and one secondary level) in Owo, Ondo state, Nigeria from 1997 to 2006. The male: female ratio was 3:1. Ages were 14–70 years (mean 33.25 years, SD ±16.76). The overall case fatality rate (CFR), 32.91%, did was not significantly different in the two hospitals. CFR for men was 32.10% and for women 35.29%. The main factor indicative of bad prognosis was a short hospitalization period. It was observed that 30.38% of our patients were discharged against medical advice (DAMA), that financial constraint was the underlying problem in 50% of cases, and that the trend of DAMA occurred at the two study sites. This DAMA phenomenon could pose a great danger to the eradication of this vaccine preventable disease in rural areas.
Keywords: Tetanus, Rural hospital, Discharge against medical advice, Nigeria
Introduction
Though tetanus has become uncommon in most developed countries, it remains a major health problem in developing countries [1]. Nigeria is not exempt from this scourge. Tetanus in developing countries is associated with high mortality. Tetanus admissions in Nigeria have recently decreased [2], but reports of discharge against medical advice among even in urban settings [3] shows that the disease may be far from being under control. In addition, there are only a few reports from the rural parts of the country. This study looks at the pattern of presentation and mortality, and at factors that influence them. It also looks at discharge against medical advice and the outcome of tetanus infections among adult patients admitted to a secondary and to a tertiary level health care centre in Owo. These two centres serve as referral centres to many primary health centres in the community.
Patients and materials
A review of the medical records of patients aged 14 years and above who had been admitted and treated in the adult wards of the Federal Medical Centre Owo and St Louis Catholic Hospital Owo, from January 1997 to December 2006 was undertaken. The diagnosis of tetanus was wholly clinical and based on the presence of one or more of the following:
Trismus
Rigidity of the neck and or abdomen
Reflex spasms
Patients with rigidity and/ or spasm limited to the wound bearing area of the body were classified as having localized tetanus, whereas those with trismus and generalized rigidity with or without generalized spasms were classified as having generalized tetanus.
Details of age, sex, outcome of treatment and whether they were discharged against medical advice were obtained. The case fatality rate (CFR) was calculated by dividing the number of deaths from tetanus by the number of admissions for tetanus and multiplied by 100.
Data analysis: The data was analysed using SPSS Version 11 and CPEA. Summary statistics such as means and percentages were used to summarize the data. Differences between mean values were tested using Student's t-test. Chi-square test and where appropriate Fishers exact test was employed to test relationships between categorical variables. The level of significance was set at P < 0.05
Results
Seventy-nine patients were seen in the two hospitals between January 1997 and December 2006: 64 in one hospital (81.01 %) and 15 in the other (18.99 %). Ages ranged between 14 and 70 years with a mean of 33.25 (SD +16.76) years. There were 62 males and 17 females, giving a male: female ratio of 3:1. Mean age of the males was 31.71 (+15.77 SD) years. Mean age of the females was 38.88 (+19.46 SD) years (t= 1.58, df =77, p = 0.12). Only one patient had localized tetanus (1.27%) while the other 78 patients had generalized tetanus (98.73%).
Twenty of the 62 males and six of the 17 females died, giving CFR of 32.25% and 35.29%, respectively (X2 = 0.03, p = 0.87). The mean age of the patients who died was 34.73 (+15.15 SD) years, while the mean age of patients who survived was 34.79 (+20.09 SD) years (t = 0.01, p = 0.99). CFR seemed to increase with age until the age of 50 years, after which it dropped (Table 1). Overall CFR was 33% in each of the two hospitals.
Table 1.
Outcome of the infection in different age groups of patients admitted in the two health facilities
| Age group (yrs) | Outcome | CFR % | |||
|---|---|---|---|---|---|
| DAMA | Survived | Died | Total | ||
| ≤20 | 6 | 8 | 5 | 19 | 26.32 |
| 21–30 | 11 | 10 | 8 | 29 | 27.59 |
| 31–40 | 4 | 3 | 5 | 12 | 41.67 |
| 41–50 | 2 | 0 | 5 | 7 | 71.43 |
| ≥51 | 1 | 8 | 3 | 12 | 25.00 |
| Total | 24 | 29 | 26 | 79 | 32.91 |
The number of tetanus admissions declined from 7 to 5 per year during 1997–1999 and was stable at six per year during 2004–2006. However, during the intervening period (2000–2003) it was about twice as high, averaging almost 11 admissions per year. The highest CFR was in 1999.
CFR for the first five-year period and the second period was the same (33.0%). A factor indicative of bad prognosis was a short period of hospitalisation; mean duration of stay for those that died was 4.5 + 2.2 days while for those that survived was 19.0 + 7.2 days, t = 9.8 df =53, p = < 0.001. Prognosis was not affected by incubation period, pulse rate, socio-economic status, or site of injury.
Twenty four out of the 79 patients (30.38%) were discharged against medical advice (DAMA). There were no incidents of DAMA in 1999 and 2000. Mean age of patients DAMA was 29.79 + 13.94 years while the mean age of those who were not DAMA was 34.76 + 17.77 years (t =1.22, df= 77, p = 0.23).
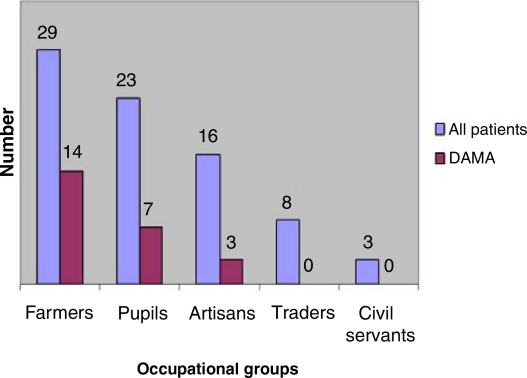
Farmers were more likely than other categories of patients to be DAMA. Twenty three of the patients who were DAMA (95.83%) were males while only 1 (4.17%) was a female. X2= 4.81; p = 0.03. Percent frequency of DAMA in the two hospitals was not significantly different (X2 = 0.033%, p = 0.82).
The most frequent routes of entry for the infection were the lower limbs (31 cases, 39.24%) and the upper limbs (15 cases, 18.99%). Other sites recorded in this study were chronic otitis media in 4 cases (5.06%), road traffic accidents with open wounds in 8 cases (10.13%). Head and neck wounds occurred in 4 cases (5.06%). One case of tetanus was secondary to a local surgery performed for enlarged tonsils (1.27%). In 6 cases (7.60%) the portal of entry was not seen, while in 10 cases (12.66%) there was no record of the portal of entry.
Discussion
Tetanus in Nigeria is a disease of the young [2, 4, 5]. In this study, 75% of the patients were 40 years and below. This is similar to other studies in other regions of Nigeria [2–4] but contrasts sharply with those from Europe, America and Asia, where tetanus has become rare and, when it occurs, is more frequent in the elderly and those above 40 years of age whose tetanus antibodies had declined with time [6–9]. The high frequency of tetanus cases in our environment is a result of inadequate and irregular tetanus immunization programmes [2].
Recent reports from Nigeria have indicated the reduction in hospital admissions for tetanus [2, 4, 10]. The reduction in admissions observed initially from 1997 to 1999 and after 2003 might be consistent with this general observation. The peak in admissions recorded during 2000–2003 might have been due to the harsh economic conditions prevalent in the country at that time.
The CFR for adult tetanus in Nigeria ranges from 0% to 64% [2–4, 10–13], from various studies in the country. The finding in this study of 33% is within this range but higher than that reported in developed countries of Europe and America [8, 9].
This study did not group tetanus patients into different categories of severity because we did not have sufficient data. In this study, the only case of localized tetanus survived CFR among females (35%) was similar to that among males (32%). A study from the same region of this country however recorded a statistically significant higher CFR in females than in males because of post abortal and post partum tetanus, which usually present with the severe form of the disease and are associated with high mortality. Also in another study, higher but statistically insignificant mortality among females than males was recorded within the first seven days of admission due to complicated induced septic abortion but there was no overall increase mortality among them [4]. Our female patients, however, did not present with any of these two conditions.
The relationship between age and CFR observed in this study is similar to those of other studies [2], though this study did not look at tetanus admissions below the age of 14 years or tetanus admissions into the intensive care unit as the two health facilities did not have such facilities at the time of this study.
Many of the patients were discharged against medical advice. DAMA rate reported among tetanus patients from the University of Port Harcourt teaching hospital in an urban city of the oil rich Niger Delta part of Nigeria was only 1.1% [3]. DAMA is a worldwide phenomenon [15] and has been reported where there are financial constraints during admission or where the admission is unplanned for. Furthermore, the nature of the illness, especially if it is terminal, and lack of proper counselling can make patients DAMA. Customs and beliefs, as well as patients' preference for alternative care givers, are other reasons why they DAMA. The DAMA rate of 30.38% in this study is indeed very high. Both Alebiosu et al 16 and Odu et al [14] in separate studies on DAMA in this same region of the country observed that financial constraint was the single most important reason why patients DAMA. In our study, 50% of those who were DAMA had clear documentation of financial difficulties in procuring drugs and other materials needed during admission. This further strengthens the finding that financial difficulty is an important reason why patients seek DAMA in this part of Nigeria. Furthermore, the majority of our patients were peasant farmers, artisans, and school children; these were the sub- set of patients that sought DAMA in the study by Odu et al [14]. It is also possible that some of our patients DAMA to seek alternative care givers. Maden et al [17] observed that many patients believe in the supernatural, traditional and faith healers, and that any delay in finding an immediate solution to their health problem by orthodox medicine will be met with DAMA. It is possible that this practice is more common among the rural dwellers than those living in urban cities of Nigeria.
The portal of entry commonly recorded in our study was the lower limbs. This agrees with separate studies by other workers where the lower limbs [7, 10] or the extremities [5] were the common portals of entry in these other tertiary institutions in Nigeria.
Limitations of the study
The patients who were DAMA were not followed up. Depending on the CFR among those who were DAMA, the CFR we report here could have been higher or lower.
Some subtle cases of tetanus might have been missed if the clinician was not sufficiently practiced in diagnosing such cases.
Conclusion
Tetanus is still a major public health problem in Nigeria, it is generally associated with high mortality, and DAMA is frequent in rural areas. Attention should be focused on the rural populace to educate the people about the disease, and effective, extended immunization programmes should be implemented to eradicate this vaccine preventable disease. Pre-school children should also receive booster doses of tetanus toxoid.
Figure 1.
Total number of patients and those who DAMA in different occupational groups.
Table 2.
Annual rates of tetanus admission, CFR, and DAMA in the two health facilities between 1997 and 2006
| Year of admission | No admitted | DAMA | Died | CFR (%) |
|---|---|---|---|---|
| 1997 | 7 | 3 | 0 | 0 |
| 1998 | 6 | 4 | 1 | 16.67 |
| 1999 | 5 | 0 | 4 | 80.00 |
| 2000 | 11 | 4 | 2 | 18.18 |
| 2001 | 12 | 2 | 7 | 58.33 |
| 2002 | 8 | 0 | 3 | 37.50 |
| 2003 | 12 | 4 | 3 | 25.00 |
| 2004 | 6 | 5 | 1 | 16.67 |
| 2005 | 6 | 1 | 3 | 50.00 |
| 2006 | 6 | 1 | 2 | 33.33 |
| Total | 79 | 24 | 26 | 32.91 |
Acknowledgements
We acknowledge the assistance of the staff of the medical records of both hospitals in retrieving the case records of these patients. We also thank Dr. Sunday Sajo of St. Louis Catholic Hospital for his assistance.
References
- 1.Campbell J. Tetanus: a major killer still at large. Afri Health. 2000;22(4):8–10. [Google Scholar]
- 2.Ojini FI, Danesi MA. Mortality of tetanus at the Lagos University Teaching Hospital, Nigeria. Trop Doct. 2005;35(3):178–81. doi: 10.1258/0049475054620806. [DOI] [PubMed] [Google Scholar]
- 3.Chapp-Jumbo EN. Neurologic admissions in the Niger Delta area of Nigeria: a ten year review. A J N S. 2004;24(1):1–15. [Google Scholar]
- 4.Sanya EO, Taiwo SS, Olarinoye JK, et al. A 12-year review of adult tetanus managed at the University College Hospital, Ibadan, Nigeria. Trop Doct. 2007;37:170–72. doi: 10.1258/004947507781524601. [DOI] [PubMed] [Google Scholar]
- 5.George AO, Ogunbiyi AO, Amanor-Boadu S, et al. Tetanus in Nigeria: the economic burden. Trop Doct. 2005;35:126–27. doi: 10.1258/0049475054036878. [DOI] [PubMed] [Google Scholar]
- 6.Thwaites CL. Tetanus. Pract Neurol. 2002;2:130–37. [Google Scholar]
- 7.Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. Br J Anaesth. 2001;87(3):477–87. doi: 10.1093/bja/87.3.477. [DOI] [PubMed] [Google Scholar]
- 8.Prospero E, Appignanesi R, D' Errico MM, et al. Epidemiology of tetanus in the marches Region of Italy. Bull W H O. 1998;76(1):47–54. [PMC free article] [PubMed] [Google Scholar]
- 9.Lau LG, Kong KO, Chew PH. A ten year retrospective study of Tetanus at a General hospital in Malaysia. Singapore Med J. 2001;42(8):342–50. [PubMed] [Google Scholar]
- 10.Onwuekwe IO, Onyedum CC, Nwabueze AC. Experience with tetanus in a tertiary hospital in South East Nigeria. Niger J Med. 2008;17(1):50–52. doi: 10.4314/njm.v17i1.37355. [DOI] [PubMed] [Google Scholar]
- 11.Bandele EO, Akinyanju OO, Bojuwoye BJ. An analysis of tetanus deaths in Lagos. J Natl Med Assoc. 1991;83:55–58. [PMC free article] [PubMed] [Google Scholar]
- 12.Arogunade FA, Bello IS, Kuteyi EA, et al. Pattern of presentation and mortality in tetanus a 10years retrospective review. Niger Postgrad Med J. 2004;11(3):198–02. [PubMed] [Google Scholar]
- 13.Ogunrin OA, Unuigbe EI. Tetanus: an analysis of the prognosticating factors of cases seen in a tertiary hospital in a developing African country between 1990 and 2000. Trop Doct. 2004;34(4):240–41. doi: 10.1177/004947550403400422. [DOI] [PubMed] [Google Scholar]
- 14.Odu OO., Bello TO, Fadiora SO. Discharge against medical advice from a tertiary hospital in Nigeria-a cause for concern. Nig Clin Rev. 2005;9:15–19. [Google Scholar]
- 15.Akiode O, Musa AA, Shonubi AM, et al. Trends of discharge against medical advice in a suburban surgical practice in Nigeria. Trop Doct. 2005;35(1):51–52. [PubMed] [Google Scholar]
- 16.Alebiosu CO, Raimi TH. Discharge against medical advice. Trop Doct. 2003;3393:191–92. doi: 10.1177/004947550303300331. [DOI] [PubMed] [Google Scholar]
- 17.Maden C, Mckendrick S, Robert G. Alternative Medicine at Vila Central hospital Vanuatu. A survey of the use of custom medicine in patients and staff. Trop Doct. 2003;3391:22–24. doi: 10.1177/004947550303300111. [DOI] [PubMed] [Google Scholar]