Abstract
Objectives:
The objective of this study was to determine the vitamin D status of pregnant Omanis by measurement of their circulating 25 hydroxy vitamin D levels.
Methods:
Blood samples were obtained from a cohort of 103 consecutive healthy pregnant Omanis at the Armed Forces Hospital, Muscat, on their first antenatal visit. The study took place in May, June and July 2010.
Results:
Vitamin D deficiency was present in 34 (33%) of patients (25OHD3 <25 nmol/L), ‘at risk’ levels were found in 67 (65%) patients (25OHD3 25–50 nmol/L); two patients (1.9%) had values between 50 and 75 nmol/L, and no patients in the optimal range >75 nmol/L.
Conclusion:
If confirmed, these findings indicate the need for vitamin D replacement during pregnancy and lactation. Although not evidence based we recommend at least 1000 IU of cholecalciferol, (vitamin D3) daily.
Keywords: Pregnancy, Oman, 25 hydroxyvitamin D3 (25OHD3), Vitamin D deficiency
Advances in Knowledge
This article is the first to draw attention to the possibility of widespread vitamin D deficiency among pregnant women in Oman.
Application to Patient Care
Until more is known about the vitamin D status in Omanis, we recommend that all pregnant women and lactating mothers should receive vitamin D supplements with at least 1000 IU vitamin D3 daily.
Deficiency of vitamin D is common worldwide1 including the Gulf states.2,3 The latter is surprising as sunlight is abundant in the Middle East. More than 90% of our vitamin D is provided by sunlight4 and it is therefore obvious that those persons affected in Arabian countries have little sunlight exposure and a diet deficient in vitamin D.
The role of vitamin D in normal physiology is complex and wide ranging. It has important immune modulating effects protecting against infection,4,5,6 autoimmune disorders7 and certain cancers, in addition to its well documented effects on the prevention of osteoporosis, fractures, falls in the elderly4,5 and impaired cognitive function.8
As we continually see patients with vitamin D deficiency in our clinics, it became important to establish whether or not vitamin stores (25OHD) are normal in a healthy Omani population. For this reason, we chose patients in their first and second trimester of pregnancy as pregnancy and lactation are associated with profound alterations in calcium absorption and skeletal remodelling necessitating increased utilisation of vitamin D. Our findings are reported below.
Methods
Blood samples were obtained from a cohort of 103 consecutive healthy Omani patients at their first antenatal visit, usually in the first, but sometimes the second trimester. They were then assayed for serum calcium (Ca), phosphate (Phos), and serum alkaline phosphatase (ALP), which were measured by spectrophotometry, (COBAS Integra 800, Roche Diagnostics, Indianapolis, USA) on the same day. Serum samples for parathyroid hormone (PTH) were measured by immunochemiluminesence (Access 2, Beckman Coulter, Inc., CA, USA), and 25(OH)D3 by the LB211 gamma counter (Berthold GmBH & Co. KG, Bad Wilbad, Germany), having been centrifuged and deep frozen at −40º C. PTH and 25(OH)D3 were then measured on the same day at the end of the study.
Statistical analysis was performed to determine the relationship between the level of serum Ca, Phos, ALP and PTH versus the level of serum 25(OH)D. We used a correlation test to calculate the significance of these relationships. As this showed no significant linear correlation, a polynomial trend curve was employed. The calculations were made for all groups of patients.
Fully informed consent was obtained from each patient to extract the blood needed for the above procedures in addition to that required for routine antenatal screening. The study was approved by the Armed Forces Hospital authorities.
Results
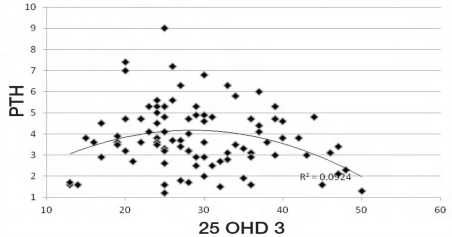
Serum 25OHD3 levels were deficient (<25 nmol/L) in 34 patients, between 25 and 50 nmol/L in 67 patients (at risk) and two patients had values between 50 and 75 nmol/L. There was no significant linear correlation between 25(OH) D3 and serum Ca, Phos or ALP levels or parity. However, a significant relationship between PTH and 25(OH)D3 was observed which differed between the ‘deficient’ and the ‘at risk’ groups. This was confirmed using a polynomial curve, which had a significant correlation value of 0.55 [Figure 1].
Figure 1:
Relationship between PTH (normal range 1.6–9.3 pmol/L) and 25(OH)D3 levels. There was no linear correlation between PTH and 25OHD3 levels, but using a polynomial curve, the correlation coefficient was significant at 0.55.
Legend: PTH = parathyroid hormone; 25(OH)D3 = vitamin D3.
Discussion
This is the first study to report vitamin D status in normal pregnant Omanis. The results are alarming: 34% of these apparently healthy women were vitamin D deficient and a further 64% ‘at risk’ at a time when there is a critical need for calcium metabolism to be normal. A pregnant woman must provide 25 to 30 gm of calcium to support the developing foetal skeleton. Much of this demand occurs in the third trimester when the foetal skeleton undergoes mineralisation. This demand is compensated for by an increased absorption of calcium from the gut induced by rising levels of PTH and the active metabolite of vitamin D, 1,25 dihydroxy vitamin D (1,25(OH)2D).9 At this point 25(OH)D will be utilised to make more 1,25(OH)2D and those patients with low stores will be at considerable risk for the development of vitamin D deficiency and osteoporosis in old age.10
To compound this problem, many Omani women have 6 or more children and breast feed for up to 2 years. During lactation, hyperabsorption of calcium does not occur and remineralisation of the maternal skeleton only starts after weaning when PTH, and 1,25(OH)2D levels rise, calcium absorption increases and urinary calcium levels fall, a process that may persist for months.11 Obviously, adequate stores of 25(OH)D are vital during this period, otherwise skeleton remineralisation will be seriously impaired and possibly result in the development of osteoporosis in old age.4,5
Interestingly, none of the patients in the 25(OH)D3 deficiency group were symptomatic and serum PTH and ALP levels were still within the normal range. However there was a significant increase of the percentage rise in PTH in the face of a declining 25(OH)D level suggesting the early stages of a biological response to vitamin D deficiency in the “at risk” group. In the deficiency group the reverse response was seen. Our 25(OH) D3 immunoassay results have been carefully checked and are correct. It is possible therefore that an overt rise of PTH and ALP levels has been suppressed by an oral intake of calcium in excess of 1 gm daily as this will delay the development of secondary hyperparathyroidism.12,13 Other factors such as body mass index may also be relevant14 but this was not examined here.
In addition to its musculo-skeletal actions, vitamin D deficiency is reportedly associated with the development of certain cancers, the metabolic syndromes and infections, as well as type 1 and type 2 diabetes,4,5 disorders which are common in Oman.
Our results confirm that vitamin D3 stores are low even in Omanis of reproductive age. These findings are similar to those reported in Saudi Arabians more than 25 years ago2 and more recently in the UAE and Qatar.3,12 It therefore seems sensible to advocate vitamin D supplementation for all pregnant women in the Middle East. At the present time, there are no clear cut recommendations as to the dose, but we recommend at least 1000 IU of vitamin D3 a day which should be continued throughout lactation. Until more is known about the daily calcium intake of Omanis, it would be prudent to advocate calcium supplementation as well.15
Conclusion
This study shows that vitamin D3 scores are low in pregnant Omanis. Further studies are required to confirm these findings. Until then, we recommend supplementation with vitamin D3 (cholecalciferol) for all pregnant and lactating mothers.
Footnotes
CONFLICT OF INTEREST
The authors reported no conflict of interest.
References
- 1.Thacher TD, Fisher PR, Strand MA, Pettifor JM. Nutritional rickets around the world: causes and future directions. Ann Tropical Paediatr. 2006;26:1–16. doi: 10.1179/146532806X90556. [DOI] [PubMed] [Google Scholar]
- 2.Woodhouse NY, Norton W. Low vitamin d levels in Saudi Arabians. King Faisal Spec Hosp Med J. 1982;2:127–31. [Google Scholar]
- 3.Saadi HF, Dawodu A, Afandi BO, Zayed R, Benedict S, Nagelkerke N. Efficacy of daily and monthly high dose calciferol in vitamin D deficient nulliparous and lactating women. Am J Clin Nutr. 2007;85:1565–71. doi: 10.1093/ajcn/85.6.1565. [DOI] [PubMed] [Google Scholar]
- 4.Holick MF. Vitamin D: A delightful health perspective. Nutrition Rev. 2008;66:5182–94. doi: 10.1111/j.1753-4887.2008.00104.x. [DOI] [PubMed] [Google Scholar]
- 5.Pearce SHS, Cheetham TD. Diagnosis and management of vitamin D deficiency. BMJ. 2010;340:b5664. doi: 10.1136/bmj.b5664. [DOI] [PubMed] [Google Scholar]
- 6.Holick MF. Vitamin D deficiency. Review article. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 7.Hyponen E, Laara E, Reunanen A, Jarvelin M-R, Vertanen SM. Intake of vitamin D and risk of type 1 diabetes. A birth cohort study. Lancet. 2001;358:1500–03. doi: 10.1016/S0140-6736(01)06580-1. [DOI] [PubMed] [Google Scholar]
- 8.Llewellyn DJ, Lang IA, Langa KM, Muniz-Terrera G, Phillips CL, Cherubini A, et al. Vitamin D and risk of cognitive decline in elderly persons. Arch Intern Med. 2010;170:1099–100. doi: 10.1001/archinternmed.2010.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Affinito P, Tommaselli GA, di Carlo C, Guida F, Nappi C. Changes in bone mineral density and calcium metabolism in breastfeeding women: A one-year follow-up study. J Clin Endocrinol Metab. 1996;81:2314–18. doi: 10.1210/jcem.81.6.8964870. [DOI] [PubMed] [Google Scholar]
- 10.Javaid MK, Crozier SR, Harvey NC, Gale CR, Dennison EM, Boucher BJ. Maternal vitamin D status during pregnancy and childhood mass at age 9 years: a longitudinal study. Lancet. 2006;367:36–43. doi: 10.1016/S0140-6736(06)67922-1. [DOI] [PubMed] [Google Scholar]
- 11.Kalkwarf HJ, Specker BL, Heubi JE, Viera NE, Yergey AL. Intestinal calcium absorption of women during lactation andafterweaning. AM J Clin Nutr. 1996;63:526–31. doi: 10.1093/ajcn/63.4.526. [DOI] [PubMed] [Google Scholar]
- 12.Saadi HF, Nagelkerke N, Benedict S, Qazaq HS, Zilahi E, Mohamadiyeh MK, et al. Predictors and relationships of serum 25 hydroxyvitamin D concentration with bone turnover markers, bone mineral density and vitamin D receptor genotype in Emirati women. Bone. 2006;39:1136–43. doi: 10.1016/j.bone.2006.05.010. Epub 2006 June 30. [DOI] [PubMed] [Google Scholar]
- 13.Steingrimsdottir L, Gumarsson O, Indridason OS, Franzson L, Sigurdsson G. Relationship between serum parathyroid hormone levels, vitamin D sufficiency and calcium intake. JAMA. 2005;294:2336–41. doi: 10.1001/jama.294.18.2336. [DOI] [PubMed] [Google Scholar]
- 14.Paik J, Curhan G, Forman J, Taylor E. Determinant of plasma parathyroid hormone levels in young women. Calcified Tissue Int. 2010;87:211–17. doi: 10.1007/s00223-010-9397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abrahamsen B. Patient level pooled analysis of 68,500 patients from seven major vitamin D fracture trials in US and Europe. (The DIPART group) BMJ. 2010;340:b5463. doi: 10.1136/bmj.b5463. [DOI] [PMC free article] [PubMed] [Google Scholar]