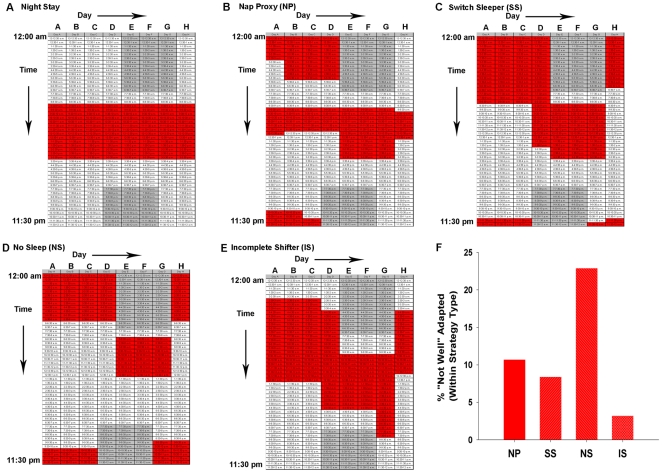
Figure 2. Representative sleep schedules for typical night-shift schedules.
Nurses were instructed to shade the time boxes for any time in which they would sleep, including any naps for only the schedules they had actually experienced. Some nurses had experienced both night-shift or day-shift and they completed both work-week schedules, but most nurses completed only one of the schedules. Each column is one 24-h period beginning at 12:00am, and each box represents 30-min. Gray shaded area refers to the night-shift work schedule (7:00pm to 7:00am for the typical night-shift schedule at Vanderbilt Hospital). Red shaded areas represent typical responses for sleep time in the surveys. These responses were categorized into five strategy types: A) Night Stay: Continued to sleep regularly in the daytime on or off shift; B) Nap Proxy (NP): On days off, they nap (longer than one hour) on at least four out of the five days off during the time in which they would normally be asleep when working night-shift; C) Switch Sleepers (SS): Switch from nights to days by using a strictly enforced schedule, but they do not give up any sleep in order to do so (i.e., they sleep late on the day they will start night-shift work); D) No Sleep (NS): Switch from days to nights and vice versa by choosing a>24-hr period to stay awake entirely; E) Incomplete Switcher (IS): Switched half-way between days and nights; F) Post hoc analysis of significant MANOVA for strategy type [F(12, 558) = 1.8, Pillai's Trace = 0.11, p<0.05] of nurses who were currently working night shift and did not choose the Night Stay strategy. Significant univariate analysis revealed a significantly greater percentage of nurses (within Strategy Type) falling into the “Not Well” Adapted category (G(3) = 8.7, p<0.05). Frequencies of nurses who reported being “Not Well” Adapted (for each group from left to right): 3/27, 8/92, 10/46, and 1/31.