Fig. 1. Mechanisms of oral tolerance induction.
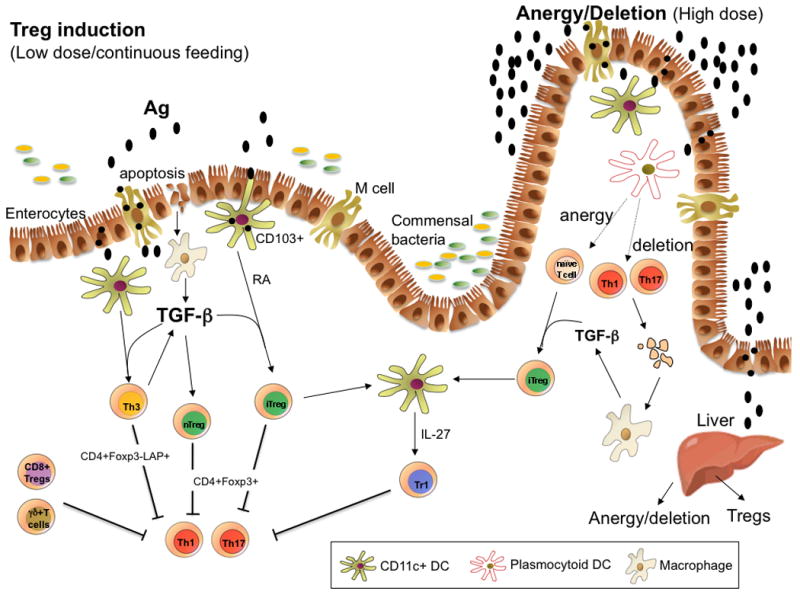
Oral antigen crosses from the intestine into the gut associated lymphoid tissue in a number of ways. It can enter via M cells, be sampled by DC processes that penetrate the lumen, or be taken up by intestinal epithelial cells. DCs in the gut are unique in that they can drive Treg differentiation from Foxp3− cells. These properties of DCs relate to their being conditioned by commensal bacteria, TGFβ and IL-10 from gut epithelial cells, and their expression of retinoic acid, which is provided in the form of vitamin A in the diet and appears to be constitutively expressed by gut DCs. CD11b monocytes may also play a role in the induction of Tregs, and the induction of Tregs occurs in the MLNs and involves both CCR7 and CCR9. Costimulation by PDL1-PDL are also important for the induction of Tregs. Macrophages are stimulated to produce TGF-β after uptaking apoptotic epithelial cells or apoptotic T cells following high dose tolerance. Lower doses of antigen favor the induction of Tregs, whereas higher doses of antigen favor anergy/deletion as a mechanism of tolerance induction. The liver may also play a role in oral tolerance induction and antigen (high dose) may be rapidly taken up by the liver, where it is processed by plasmacytoid DCs that induce anergy and deletion. A number of different types of Tregs may be induced or expanded in the gut including CD4+CD25+Foxp3+ iTregs, nTregs, Tr1 cells, LAP+ Tregs (Th3 cells), CD8+ Tregs, and γδ T cells.
