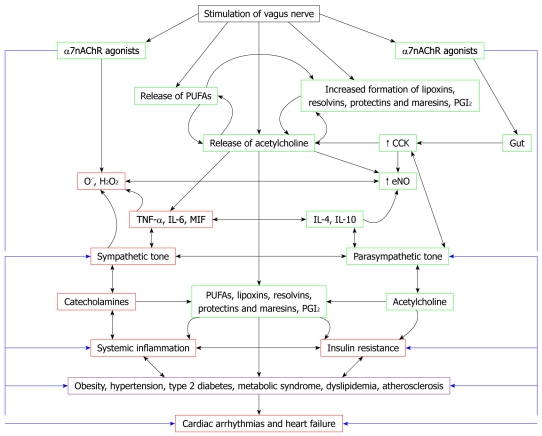
Figure 1.
Scheme showing relationship between vagal nerve stimulation, autonomic nervous system, inflammation, insulin resistance, metabolic syndrome and cardiac arrhythmias and cardiac failure. Inflammation plays a significant role in coronary heart disease (CHD) and cardiac arrhythmias and conditions that predispose to its development such as atherosclerosis. In contrast, vagal nerve stimulation (VNS) has anti-inflammatory activity, an antifibrillatory effect, and is beneficial in heart failure. Cardiac arrhythmias are due to local inflammation, oxidative injury, altered myocyte metabolism, extracellular matrix remodeling, and fibrosis. Myeloperoxidase (MPO)-deficient mice show reduced activity of matrix metalloproteinases (MMPs), blunted myocardial fibrosis, and markedly reduced incidence of arrhythmias. Patients with cardiac arrhythmias have higher plasma and myocardial concentrations of MPO compared to controls. Activation of leukocytes occurs in cardiac arrhythmias and congestive heart failure (CHF) that leads to excess production of MPO. Increased production of leukocyte MPO could be secondary to a deficiency of lipoxin A4 (LXA4) and prostacyclin (PGI2), which are potent anti-inflammatory, organ-protective, antifibrotic, and antiarrhythmic molecules. Thus, under normal physiological conditions, a delicate balance exists between proinflammatory molecules such as interleukin (IL)-6, tumor necrosis factor (TNF)-α, macrophage migration inhibitory factor (MIF), MPO and anti-inflammatory molecules such as IL-4, IL-10, NO, lipoxins, resolvins, protectins and maresins. Similarly, a balance exists between sympathetic tone and parasympathetic tone. Catecholamines (the neurotransmitters of the sympathetic nervous system) have proinflammatory actions, whereas acetylcholine (the principal neurotransmitter of the vagus nerve) has anti-inflammatory actions. Acetylcholine and VNS might augment the production of anti-inflammatory molecules lipoxins, resolvins, protectins and maresins. Thus, VNS is beneficial in cardiac arrhythmias, CHF and in other low-grade systemic inflammatory conditions such as obesity, hypertension, type 2 diabetes, metabolic syndrome, dyslipidemia, atherosclerosis and insulin resistance. Hence, measurement of plasma/leukocyte content of acetylcholine, catecholamines, IL-6, TNF-α, MIF, IL-4, IL-10, various PUFAs, lipoxins, resolvins, protectins, maresins and vagal tone could be used for prediction of disease progression, and assessing prognosis and response to treatment of CHF and cardiac arrhythmias.