Abstract
The goal of a fusion of the lumbar spine is to obtain a primary solid arthrodesis thus to alleviate pain. Different circumferential fusion techniques have been described such as combined anterior–posterior fusion (APF), instrumented posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). The TLIF procedure has rapidly gained popularity; because of its posterolateral extracanalar discectomy and fusion, it has been reported as a safe technique, without the potential complications described when using combined APF and PLIF techniques. A retrospective clinical and radiographic study was performed. The database of our Center was interrogated in a retrospective way to extract data from patients that underwent a one or two level lumbar fusion with TLIF approach. All patients had symptomatic disc degeneration of the lumbar spine. One hundred and fourteen levels fused from 2003 to 2008. All patients were operated in the same center. All the patients were operated by the same surgical team. Patients were evaluated preoperatively and postoperatively at 1 and 3 months and 1 and 2 years follow-up. The spine was approached through a classic posterior midline incision and subperiosteal muscular detachment. The side of facetectomy was chosen according to the subject’s symptoms of leg pain if present. A posterolateral annulotomy was made and subtotal discectomy was performed and the hyaline cartilage of endplates was removed. Once the surgeon was satisfied with endplate preparation, a banana shaped allograft spacer was inserted through the annulotomy and placed anteriorly. Additional autograft locally harvested from decompression was packed behind the allograft spacer in all cases. Laminae and the remaining contralateral facet joint were decorticated, and packed with bone graft (local autologous and allograft chips in some cases). The posterior fusion was instrumented with pedicle screws and titanium rods. The TLIF procedure had led to shortened surgical times, less neurologic injury, and improved overall outcomes. The introduction of the TLIF procedure has allowed surgeons to achieve successful fusion without the risk of nerve root tethering that is seen so frequently with standard PLIF techniques.
Keywords: TLIF, Minimal invasive fusion, Degenerative disc disease, Interbody fusion
Introduction
Methods of spinal arthrodesis continue to evolve, in efforts to treat back pain. The latest techniques include approaching from anterior, posterior, lateral and posterolateral.
Interbody fusion techniques have been developed to provide solid fixation of spinal segments while maintaining load-bearing capacity and proper disc height [1]. The ability to reconstruct the anterior column after disc removal is important because, as well know, 80% of the compressive, torsion, and shear forces are transmitted through the anterior column [2, 3]. Reconstruction of the anterior column can be performed via the anterior approach, with direct transperitoneal or retroperitoneal access to the lumbar spine. Posterior fusion and instrumentation can be added to obtain a 360° fusion. This technique involves two surgical approaches, with increased operating time (compared to posterolateral fusion) as well as potential complications related to anterior approaches to the lumbar spine.
An alternative method of reconstructing the anterior column is via posterior lumbar interbody fusion. The transforaminal lumbar interbody fusion (TLIF) developed by Harms [4] is a modification of the posterior lumbar interbody fusion (PLIF). The TLIF has been shown to be valuable alternative to the traditional PLIF [5–7]. Advantages of the TLIF over PLIF are fewer complications, elimination of epidural scarring, less intraoperative bleeding [5], and avoidance of dura and nerve roots. Further, given its unilateral approach, better preservation of the lumbar spine musculoligamentous complex is obtained.
Materials and methods
A retrospective clinical and radiographic study was performed.
The database of our Center was analyzed in a retrospective way to extract data from patients that underwent a one or two level lumbar fusion with TLIF procedure. All patients founded (n = 100) in this series had variable component of degenerative disc disease. Secondary associated diagnoses such as recurrent herniated nucleus pulposus (HNP) or other degenerative stenosis were accepted for inclusion.
Twenty patients in this series had prior spinal surgeries with the most common being decompression surgeries such as discectomies and laminectomies at one or more of the operated levels.
Patients with scoliosis, severe spondylolisthesis (more than grade I–II Meyerding), infection, or tumor were excluded.
From December 2003 until December 2008, 100 patients (62 males and 38 females) with a mean age of 54.2 ± 10.2 years (range 34–69 years) underwent the TLIF procedure for a variety of lumbar pathologies: revision surgery after failed discectomy and decompression by open posterior midline approach (n = 20); spondylolisthesis grade I–II (n = 38) severe degenerative disc disease (n = 56).
The distribution of levels fused is the sequent: in one level fixation cases the level fused was L3–L4 (n = 3), L4–L5 (n = 36); L5–S1 (n = 40); in two level fixation cases the level fused with TLIF was L3–L4–L5/TLIF L4–L5 (n = 8); L4–L5–S1/TLIF L5–S1 (n = 13).
The cage material was not always the same: Peek (n = 56), Carbon fiber (n = 58).
All of the patients in this series had low back pain as their predominant symptom, with varying degrees of radicular pain and neurologic symptoms. All patients underwent at least 6 months of nonoperative care before coming to surgery.
Clinical and radiological evaluation
The data collected retrospectively for analysis were age, gender, previous diagnoses, revision diagnosis, duration of symptoms, levels of fusion, operating time, intraoperative blood loss, clinical and radiographic results after surgery, and complications. Back and leg pain was quantified by visual analog scores (VAS) collected from the patients preoperatively, postoperatively, and in last follow-up.
The SF-36 was used both before and after surgery to give surgeon information about the patient’s satisfaction. Clinical outcome was assessed at a minimum of 1 year follow-up and compared to a pre-operative baseline value using Short Form 36 (SF-36) and VAS.
Preoperative radiological evaluation included anteroposterior, lateral, and flexion–extension plain radiograph, magnetic resonance imaging (MRI) (Fig. 1). Fusion rates were assessed by the same surgical orthopedic team using static and dynamic plain X-rays at 3 and 12 months after surgery (Fig. 2). In ten cases, we have performed a CT scan to confirm the fusion rate (Fig. 3). Definitive fusion was identified by the formation of trabecular bony bridges between contiguous vertebral bodies at the instrumented levels, intact hardware, and less than 3 degree segmental movement according to the fusion criteria.
Fig. 1.

MRI preop. show recurrent disc herniation at L4L5
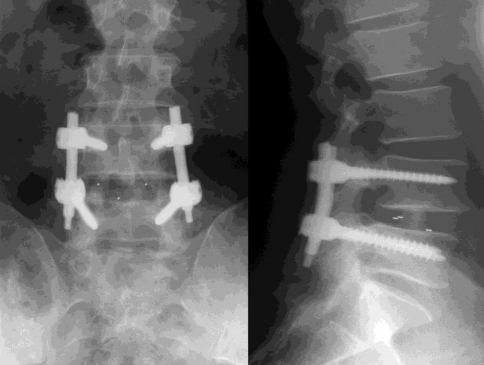
Fig. 2.
Rx 1 year F.U. after TLIF L4L5
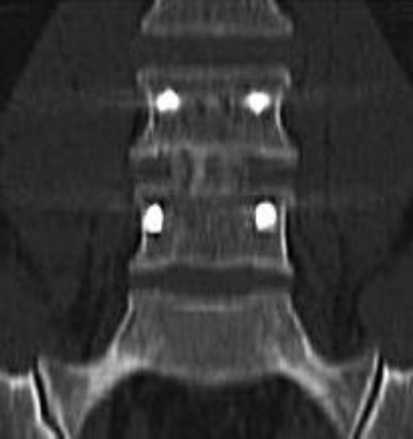
Fig. 3.
CT scan 1 year F.U. after TLIF L4L5
Statistical analyses were performed using SPSS 11.0 for Mac OS X. Student’s t test was used for the comparison of continuous variables. P values below 0.05 were accepted for significance.
Results
We identified 100 subjects who underwent a one or two level stabilization with TLIF.
The mean blood loss was 320 ± 120.2 mL and the mean postoperative length of stay was 4.1 ± 2.2 days.
No major surgical complication was observed. There were no complications related to internal fixation breakage, loosening or displacement.
In five cases, we found a L5 nerve root irritation with weakness due to pedicle screw malplacement that was also noticed immediately postoperatively and reoperated in few days.
All patients achieved spinal fusion in the last X-rays control. There were three cases of cage anterior migration in patients affected by obesity. There were three cases of loss of disk space height and foramen height between the initial and final postoperative X-rays suggestive of cage subsidence over time.
In our experience, the different material of the cage does not influence the rate of fusion without statistical relevance of difference into the two groups of materials: carbon fiber or peek.
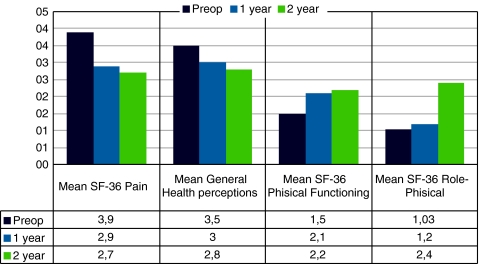
The SF-36 outcomes instrument was automatically administered before surgery in all patients but only in 90% of patients we have the SF-36 Questionnaire available for 12 months after surgery and 24 months after surgery. The preoperative, 12-month and 24-month postoperative scores were compared and analyzed in this study.
SF-36 outcomes analysis demonstrated a statistically significant improvement in the 12- and 24-month mean pain scores and 24-month mean role physical scores compared with the preoperative scores on the same scales (Fig. 4).
Fig. 4.
Clinical results
Discussion
Amongst all the lumbar spinal fusion techniques, combined APF offers the highest mechanical stability and the best chances of bony fusion [8]. However, it is well recognized that the anterior approach may result in severe, sometimes life threatening intraoperative complications, because the surgeon has to work in proximity of major anatomical structures [9, 10].
TLIF is a variant of the PLIF technique described by Cloward in the 1950s [11]. PLIF has been associated with the high incidences of neurological complications, up to 13.6% permanent neurologic lesions in Barnes’ et al. study, in particular of the traversing nerve root [12, 13]. This is due to the fact that a great amount of traction on the dural sac is required to implant the interbody fusion devices.
The TLIF technique was described by Harms and Jeszenszky [4] as a modification of the well-established PLIF procedure. The TLIF uses a posterior approach to the spine that runs through the far lateral portion of the vertebral foramen accesses the disc space, which provides the surgeon with a fusion procedure that may reduce many of the risks and limitations associated with PLIF [14], yet produces similar stability in the spine. This has been shown to reduce the incidence of postoperative radiculitis [15]. TLIF usually is performed by unilateral approach preserving the interlaminar surface on the contralateral side, which can be used as a site for additional fusion. Like PLIF, TLIF is easily enhanced when combined with posterolateral fusion and instrumentation. Both procedures can provide circumferential spinal stabilization through a single posterior approach, but the more lateral access to the disk space in the TLIF technique requires less retraction of the thecal sac and neural elements than with the PLIF technique.
The angle of approach normally obtained during TLIF allows a unilateral approach to the disc space, thus reducing operative time and blood loss.
Conclusion
This study evaluated the clinical and radiographic results in 100 patients from one center who underwent instrumented TLIF. According to the international concerns, in our experience, the TLIF procedure had led to shortened surgical times, less neurologic injury, and improved overall outcomes. The introduction of the TLIF procedure has allowed surgeons to achieve successful fusion without the risk of nerve root tethering that is seen so frequently with standard PLIF techniques.
Conflict of interest
None.
References
- 1.Stonecipher T, Wright S. Posterior lumbar interbody fusion with facet-screw fixation. Spine. 1989;14:468–471. doi: 10.1097/00007632-198904000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Harms J. Screw-threaded rod system in spinal fusion surgery. Spine. 1992;6:541–575. [Google Scholar]
- 3.Yang SW, Langrana NA, Lee CK. Biomechanics of lumbosacral spinal fusion in combined compression–torsion loads. Spine. 1986;11:937–941. doi: 10.1097/00007632-198611000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Harms J, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998;6:88–99. [Google Scholar]
- 5.Humphreys SC, Hodges SD, Patwardhan AG, et al. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001;26:567–571. doi: 10.1097/00007632-200103010-00023. [DOI] [PubMed] [Google Scholar]
- 6.Lowe TG, Tahernia AD, O’Brien MF, et al. Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech. 2002;15:31–38. doi: 10.1097/00024720-200202000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Whitecloud TS, III, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior–posterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord. 2001;14:100–103. doi: 10.1097/00002517-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Oxland TR, Lund T. Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J. 2000;9(suppl 1):S95–S101. doi: 10.1007/PL00010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brau SA, Delamarter RB, Schiffman ML, Williams LA, Watkins RG. Vascular injury during anterior lumbar surgery. Spine J. 2004;4:409–412. doi: 10.1016/j.spinee.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Herkowitz HN, Sidhu KS. Lumbar spine fusion in the treatment of degenerative conditions: current indications and recommendations. J Am Acad Orthop Surg. 1995;3:123–135. doi: 10.5435/00124635-199505000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg. 1953;10:154–168. doi: 10.3171/jns.1953.10.2.0154. [DOI] [PubMed] [Google Scholar]
- 12.Fraser RD. Interbody, posterior, and combined lumbar fusions. Spine. 1995;20:167S–177S. doi: 10.1097/00007632-199512151-00016. [DOI] [PubMed] [Google Scholar]
- 13.Hee HT, Castro FP, Jr, Majd ME, Holt RT, Myers L. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord. 2001;14:533–540. doi: 10.1097/00002517-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Posterior lumbar interbody fusion: a retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999;70:329–334. doi: 10.3109/17453679908997819. [DOI] [PubMed] [Google Scholar]
- 15.Harms J. Screw-threaded rod system in spinal fusion surgery. Spine. 1992;6:541–575. [Google Scholar]