Abstract
We report a case of lingual ischemia and swelling in an elderly stroke patient from prolonged insertion of a FastrachTM Laryngeal Mask Airway ® following a failed Emergency Department intubation. Simple suggestions to mitigate such injury are provided.
CASE REPORT
A 75-year-old woman (71 kg, 165 cm) was brought to a small, rural, emergency department (ED) with a two-day history of headache and confusion. Computerized tomography of the head demonstrated an acute intracerebral hemorrhage without signs of midline shift. One hour into her ED course the patient had a brief generalized tonic-clonic seizure followed by a second seizure 20 minutes later. The patient then developed a prolonged postictal phase and appeared unable to protect her airway, prompting endotracheal intubation. After three unsuccessful intubation attempts by direct laryngoscopy (DL) performed by a single ED physician, a size 5 Fastrach™ Intubating Laryngeal Mask Airway® (FT-LMA) [Laryngeal Mask Company, Jersey, UK] was successfully inserted as a rescue airway device. It is unknown why a FT-LMA was selected, what volume of air was used to inflate the FT-LMA cuff, or why intubation via the FT-LMA was not attempted. The patient was placed on a ventilator, appropriate medical management was instituted, and she was transported to our facility for definitive neurosurgical care.
The patient arrived in the intensive care unit at our facility approximately five hours after placement of the FT-LMA. The anesthesia team was consulted for endotracheal intubation and removal of the FT-LMA. An initial oral exam revealed edema and marked purple-black discoloration of the tongue. Fiberoptic bronchoscope (FOB) exam through the FT-LMA demonstrated marked edema of all glottic structures. After unsuccessful attempts to intubate the patient with FOB-assistance through the FT-LMA, a bedside tracheostomy was performed by the surgical service. The FT-LMA was then removed and the oropharnyx inspected, revealing the entire length of tongue (from tip to base) to be swollen, markedly purple-black in coloration, and free of lacerations. Pictures taken two days later with the patient awake and following commands demonstrated residual discoloration of the tongue (Figure 1). The patient denied any sensory deficits to the tongue, dysarthria, dysphagia, or stridor. The patient did not experience any necrosis or sloughing of her lingual mucosal surfaces and did not appear to have any lasting sequela from the prolonged FT-LMA insertion. She was ultimately discharged home in good condition.
Figure 1.
Discoloration of the patient’s tongue
DISCUSSION
A number of different extraglottic devices are available for use in the ED. The FT-LMA is an intubating laryngeal airway intended to provide both ventilation and the consistent ability to pass an endotracheal tube (ETT) blindly into the trachea. It has been in use for over 12 years with an overall low complication rate.1 Reported complications include: esophageal intubation, esophageal perforation, sore throat, dysphagia, dental damage and aspiration.2–7 Because the FT-LMA is used primarily to facilitate intubation in the operating room and then removed, there is little information on complications from prolonged insertion. The FT-LMA is more likely to be left in place when used in the ED and emergency medical service settings either because providers are not trained to intubate through it (used strictly as a rescue device), have less experience and therefore less success at intubation, and/or because of recommendations not to attempt removal in these settings.1
Kihara et al5 showed that the pharyngolaryngeal morbidity of sore throat and mouth was more common with the FT-LMA compared to the Classic™ laryngeal mask airway (C-LMA) following anesthesia lasting one to two hours. However, the degree of morbidity of their complications was significantly less than our current case. It is possible that our patient’s lingual ischemia was exacerbated by the three intubation attempts or by trauma secondary to a seizure activity; however, an oropharyngeal exam revealed no evidence of oropharyngeal injury or lacerations. Moreover, she did not have history of coagulopathy or conditions predisposing her to lingual ischemia (i.e. vascular disease, diabetes). The dearth of traumatic evidence in combination with Keller et al8 pharyngeal pressure data point to the FT-LMA as the likely culprit.
Using strain gauge microchip sensors attached to a size 5 FT-LMA, Keller et al8 demonstrated that the FT-LMA generates pharyngeal mucosal pressures that exceed estimated mucosal capillary perfusion pressures at the manufacturer’s recommended intracuff volumes. They suggest that the device be left in situ the shortest possible time to reduce the chance of pharyngeal mucosal ischemia and injury.8 A literature search revealed no case reports of clinically significant injuries related to prolonged FT-LMA insertion times. There are two cases of significant lingual edema in an infant and an adult after the use of a C-LMA.9–10 However, we are reporting the first serious complication due to the prolonged FT-LMA use in an elderly female stroke patient in which significant lingual ischemia resulted after an insertion time of less than five hours.
Keller et al8 demonstrated that the FT-LMA provides a more effective seal than the C-LMA, but pharyngeal mucosal pressures are significantly higher and always exceed capillary perfusion pressure when typical cuff volumes are used. The major difference between the FT-LMA and other laryngeal masks (i.e. the C- LMA, Unique™, ProSeal™ [P-LMA]) is its rigid metal airway tube. This airway tube is pressed against the anterior cervical vertebrae in the distal hypopharynx generating an area of maximal pharyngeal pressure.8
In a more recent cadaveric study, Ulrich-Pur et al11 used microchip sensors to examine mucosal pressure exerted by the cuffs of various airway devices including the FT-LMA, C-LMA and the P-LMA. They too found that the FT-LMA exerted the greatest pharyngeal pressure at all recommended cuff volumes and concluded “cuff pressures do not suggest a clinically relevant danger, because the investigated devices…are not intended for prolonged use.”11 We would suggest the ultimate duration of use for a particular device may be unpredictably prolonged; hence, an understanding of its hazards is in order.
Other extraglottic airway devices have also been implicated as the cause of various oropharyngeal trauma issues. The literature is replete with oropharyngeal nerve (hypoglossal, lingual, recurrent laryngeal) injuries associated with the use of the C-LMA.12–18 Two prior reports describe significant lingual edema with the use of the C-LMA. In the first of these, an oversized C-LMA (use of size 2.5 when 2 is recommended) was placed in a 10.6 kg one-year-old for a five-hour case.9 The other case involved a correctly sized C-LMA placed in an adult that led to marked lingual edema and cyanosis after a 90-minute procedure .10 Both cases were exemplary for noticeable tongue protrusion out of the mouth after initial inflation of the C-LMA’s cuff. The authors postulate tongue protrusion may indicate a potential size mismatch between the device and the patient’s oropharynx, which may contribute to venous or arterial obstruction.
The P-LMA has also been implicated as causing injury to the lingual, hypoglossal and recurrent laryngeal nerves.19–21 A recent case involved the uncuffed i-Gel (Intersurgical, Wokingham, Berkshire, UK) in which a patient had an atraumatic device placement for a two-hour case and awoke with a sore and partially numb tongue that also had decreased taste; these symptoms persisted for three weeks.22 Though our patient did not have any sensory deficits, it is likely that a similar traumatic mechanism due to prolonged placement or malposition may have led to either impaired tongue arterial perfusion or venous drainage resulting in a compromised airway.
Various factors should be employed to insure that cuff pressure is minimized when using the FT-LMA – whether for brief or prolonged use. Clinicians should insure that cuff volumes are kept to the manufacturers’ recommendations and that cuff pressure is monitored if the FT-LMA is used beyond a brief placement for intubation. If it is necessary to use the FT-LMA as the primary airway device, the cuff volumes should be minimized. For example, an adequate seal may be achieved with far less than the recommended maximum of 40 ml for the size 5 FT-LMA, especially if a patient is being vigorously resuscitated with the predictable resultant airway edema. Additionally, multiple authors and the manufacturer all suggest that the device be removed immediately after successful intubation.1,8,11,23 If FT-LMA removal is not possible but an ETT is able to be placed via the FT-LMA, it is imperative that the FT-LMA cuff be deflated once endotracheal intubation is confirmed.
Finally, two additional issues need to be addressed. Firstly, it was not documented as to why the initial attempts at DL were unsuccessful. The cause of the difficult DL would possibly have helped elucidate the putative factors generating her lingual ischemia. Secondly, it is unclear why a size 5 FT-LMA was selected for the case patient. By size characteristics, a size 4 FT-LMA would have been more appropriate in a 71-kg 165-cm-tall woman. Though the size 5 FT-LMA allowed for adequate ventilation, the inability to perform FOB-assisted intubation indicates it was not seated appropriately in the laryngeal inlet and likely contributed to the lingual ischemia. In the authors’ experience, when using the FT-LMA, the inability to adequately visualize the glottis via a FOB with minimal device manipulations is a strong indicator that the incorrect size FT-LMA has been chosen. In this case, the size 5 FT-LMA was likely too large and led to possible lingual injury.
While the FT-LMA remains an outstanding extraglottic airway device, this case demonstrates that caution is necessary when leaving the FT-LMA in place for periods of several hours or more. Suggested techniques to limit harm include removing the device as soon as feasible, using minimum cuff volumes, and deflating the cuff entirely if intubation is achieved but the device cannot be safely removed.
RECOMMENDATIONS TO MINIMIZE RISK OF OROPHARYNGEAL, LARYNGEAL, AND LINGUAL INJURY
Appropriate training
Before using the FT-LMA, the clinician should fully read the manufacturer’s instruction guide (http://www.lmana.com/docs/IFU(US)-Fastrach.pdf).23 Ideally, clinicians should gain experience in placement, intubation and removal in an elective setting in patients with non-difficult airways. Also, experience with the FT-LMA should also be obtained by using the device in a simulator/mannequin setting.
Appropriate size selection
Size 3 - 30–50 kg
Size 4 - 50–70 kg
Size 5 - 70–100 kg
It is important to note that the weight ranges have some overlap and clinical judgment may lead one to place a certain size FT-LMA in a patient that falls outside the respective devices’ weight range (i.e. placing a size 4 in a 90 kg obese short-statured patient).
Minimize cuff pressure / volume
If the FT-LMA is used without an ETT, insure no more than the maximum volume of air is used in the cuff (20cc - size 3; 30cc - size 4; 40cc - size 5). The recommended maximum cuff pressure is 60 cm H2O if the device is only being used as a conduit to intubation; if it is being left in situ, a pressure of 20–30 cm H2O is recommended.23 Moreover, it is very common to have an adequate seal and appropriate ventilatory parameters with cuff volumes that are as low as half the recommended inflation volume.
If one is unable to directly measure cuff pressure, an alternative to insuring minimal cuff pressures is to pressurize the breathing circuit and observe airway pressures while listening for a cuff leak. One can then minimize the cuff volume while insuring the cuff leak is achieved at 20 cm H2O of airway pressure.
If an ETT is placed via the FT-LMA, but the device is unable to be removed, leave the FT-LMA cuff fully deflated and have it removed at the earliest possible point.
Additionally, if the FT-LMA is left in situ, the head and neck of the patient should be kept midline and in the neutral position in order to minimize device pressure.
Minimize duration of time device remains in-situ
Because of the above discussed issues with its prolonged use, the FT-LMA should be removed as soon as possible, regardless of whether it has been used as a conduit for intubation or as a stand-alone device. There are no formal guidelines or published recommendations on the maximum duration the FT-LMA can safely be left in situ.
Intubation via the FT-LMA
Blind intubation and assisted-methods (i.e. FOB) have high (>90%) first attempt success rates with the FT-LMA.
Blind intubation recommendations:
Insure ventilation is optimal via FT-LMA initially (insures glottis and device aperture aligned)
Consider adjunctive drugs (low muscle relaxant, opioids)
Raise device in vertical / sagittal plane
Use well-lubricated (water based) reinforced ETT or reverse-oriented standard ETT (to minimize angle of exit from FT-LMA aperture)
Indirect / adjunctive intubation recommendations:
FOB guidance is the author’s preferred technique because of the likely minimal airway trauma generated and the assurance of confirming the definitive tracheal placement of the ETT. Two recommendations from our significant experience with the FOB include: a) insure the liberal application of a water-based lubricant to the FOB and the airway tube of the FT-LMA and b) insure that the FOB is advanced at least halfway to the carina to insure the FOB does not slip out during ETT advancement.
Airway exchange catheter can be inserted through FT-LMA and tracheal placement confirmed with capnography followed by ETT insertion.
Gum elastic bougie was used in emergency airway situations when a FOB was unavailable. Once the FT-LMA is in place, the bougie is inserted through the airway tube, tracheal rings can be detected by feel, and an ETT can be advanced over the bougie.
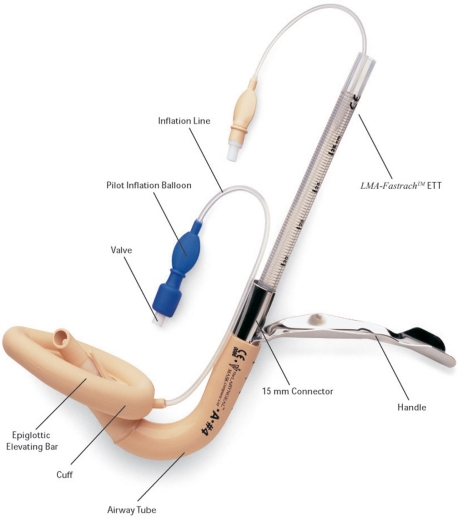
Figure 2.
Fastrach™ Intubating Laryngeal Mask Airway®
Footnotes
Reprints available through open access at http://scholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias.
REFERENCES
- 1.Gerstein NS, Braude DA, Hung O, et al. The Fastrach™ Intubating Laryngeal Mask Airway®: an overview and update. Canadian Journal of Anaesthesia. 2010;57:588–601. doi: 10.1007/s12630-010-9272-x. [DOI] [PubMed] [Google Scholar]
- 2.Pandit JJ, MacLachlan K, Dravid RM, et al. Comparison of times to achieve tracheal intubation with three techniques using the laryngeal or intubating laryngeal mask airway. Anaesthesia. 2002;57:128–32. doi: 10.1046/j.0003-2409.2001.02401.x. [DOI] [PubMed] [Google Scholar]
- 3.Dimitriou V, Voyagis GS. The intubating laryngeal mask airway (ILMA): disadvantage of being a blind technique. European Journal of Anesthesiology. 1999;16:418–9. doi: 10.1046/j.1365-2346.1999.00491.x. [DOI] [PubMed] [Google Scholar]
- 4.Branthwaite MA. An unexpected complication of the intubating laryngeal mask. Anaesthesia. 1999;54:166–7. doi: 10.1046/j.1365-2044.1999.00635.x. [DOI] [PubMed] [Google Scholar]
- 5.Kihara S, Yaguchi Y, Brimacombe J, et al. Routine use of the intubating laryngeal mask airway results in increased upper airway morbidity. Canadian Journal of Anaesthesia. 2001;48:604–8. doi: 10.1007/BF03016840. [DOI] [PubMed] [Google Scholar]
- 6.Asai T. Dental damage caused by the intubating laryngeal mask airway. Anesthesia and Analgesia. 2006;103:785. doi: 10.1213/01.ANE.0000227159.94345.3A. [DOI] [PubMed] [Google Scholar]
- 7.Keller C, Brimacombe J, Bittersohl J, et al. Aspiration and the laryngeal mask airway: three cases and a review of the literature. British Journal of Anaesthesia. 2004;93:579–82. doi: 10.1093/bja/aeh228. [DOI] [PubMed] [Google Scholar]
- 8.Keller C, Brimacombe J. Pharyngeal mucosal pressures, airway sealing pressures, and fiberoptic position with the intubating versus the standard laryngeal mask airway. Anesthesiology. 1999;90:1001–6. doi: 10.1097/00000542-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Stillman PC. Lingual oedema associated with the prolonged use of an inappropriately large laryngeal mask airway (LMA™) in an infant. Paediatric Anaesthesia. 2003;13:637–9. doi: 10.1046/j.1460-9592.2003.01050.x. [DOI] [PubMed] [Google Scholar]
- 10.Twigg S, Brown JM, Williams R. Swelling and cyanosis of the tongue associated with the use of a laryngeal mask airway. Anaesthesia and Intensive Care. 2000;28:449–450. doi: 10.1177/0310057X0002800417. [DOI] [PubMed] [Google Scholar]
- 11.Ulrich-Pur H, Hrska F, Krafft P, et al. Comparison of mucosal pressures induced by cuffs of different airway devices. Anesthesiology. 2006;104:933–8. doi: 10.1097/00000542-200605000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Umapathy N, Eliathamby TG, Timms MS. Paralysis of the hypoglossal and pharyngeal branches of the vagus nerve after use of a LMA and ETT. British Journal of Anaesthesia. 2001;87:322. [PubMed] [Google Scholar]
- 13.Sommer M, Schuldt M, Runge U, et al. Bilateral hypoglossal nerve injury following the use of the laryngeal mask without the use of nitrous oxide. Acta Anaesthesiologica Scandinavica. 2004;48:377–8. doi: 10.1111/j.0001-5172.2004.0332.x. [DOI] [PubMed] [Google Scholar]
- 14.Majumder S, Hopkins PM. Bilateral lingual nerve injure following the use of the laryngeal mask airway. Anaesthesia. 1998;53:184–6. doi: 10.1046/j.1365-2044.1998.00313.x. [DOI] [PubMed] [Google Scholar]
- 15.Gaylard D. Lingual nerve injury following the use of the laryngeal mask airway. Anaesthesia and Intensive Care. 1999;27:668. [PubMed] [Google Scholar]
- 16.Lloyd Jones FR, Hegab A. Recurrent laryngeal nerve palsy after laryngeal mask airway insertion. Anaesthesia. 1996;51:171–2. doi: 10.1111/j.1365-2044.1996.tb07707.x. [DOI] [PubMed] [Google Scholar]
- 17.Daya H, Fawcett W, Weir N. Vocal cord palsy after use of the laryngeal mask airway. Journal of Laryngology & Otology. 1996;110:383–4. doi: 10.1017/s0022215100133699. [DOI] [PubMed] [Google Scholar]
- 18.Cros AM, Pitti R, Conil C, et al. Severe dysphonia after use of a laryngeal mask airway. Anesthesiology. 1997;86:498–500. doi: 10.1097/00000542-199702000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Brimacombe J, Clarke G, Keller C. Lingual nerve injury associated with the ProSeal laryngeal mask airway: a case report and review of the literature. British Journal of Anaesthesia. 2005;95:420–3. doi: 10.1093/bja/aei187. [DOI] [PubMed] [Google Scholar]
- 20.Trumpelmann P, Cook T. Unilateral hypoglossal nerve injury following use of a ProSeal laryngeal mask. Anaesthesia. 2005;60:101. doi: 10.1111/j.1365-2044.2004.04056.x. [DOI] [PubMed] [Google Scholar]
- 21.Kawauchi Y, Nakazawa K, Ishibashi S, et al. Unilateral recurrent laryngeal nerve neuropraxia following placement of a ProSeal laryngeal mask airway in a patient with CREST syndrome. Acta Anaesthesiologica Scandinavica. 2005;49:576–8. doi: 10.1111/j.1399-6576.2005.00616.x. [DOI] [PubMed] [Google Scholar]
- 22.Michalek P, Donaldson WJ, Hinds JD. Tongue trauma associated with the i-gel supraglottic airway. Anaesthesia. 2009;64:692–3. doi: 10.1111/j.1365-2044.2009.05954_1.x. [DOI] [PubMed] [Google Scholar]
- 23.LMA North America Inc LMA Fastrach™ Reusable and LMA Fastrach™ Single Use Instruction Manual, 2006 edition. Available at www.lmana.com/docs/LMAFastrach_manual.pdf. Accessed December 2009.
- 24.Timmermann A, Russo SG, Crozier TA, et al. Intubating laryngeal mask airway for difficult out-of-hospital airway management: a prospective evaluation. British Journal of Anaesthesia. 2007;99:286–291. doi: 10.1093/bja/aem136. [DOI] [PubMed] [Google Scholar]