Figure 4. Adjusted association between ultrafiltration rate (UFR) and (1) cardiovascular (CV) hospitalization and all-cause mortality, (2) CV hospitalization and CV-related mortality, and (3) CV hospitalization.
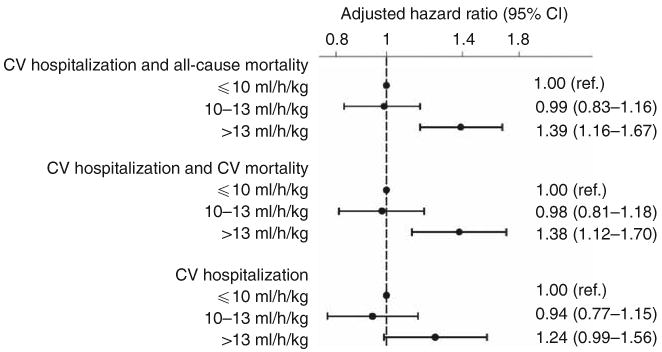
Based on Cox regression models adjusted for age, sex, interdialytic weight gain, race (black, non-black), smoking status (never, past, current), vintage (< 1, 1–2, 2–4, ≥ 4 years), access type (graft, fistula, catheter), systolic blood pressure (< 120, 120–140, 140–160, 160–180, ≥ 180 mm Hg), residual urine output (≤ versus > 200 ml/day), diabetes, congestive heart failure, peripheral vascular disease, ischemic heart disease, cerebrovascular disease, serum albumin, creatinine, hematocrit (< 30, 30–33, 33–36, ≥ 36%), and phosphorus, and use of α-adrenergic blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, β-blocker, calcium channel blocker, nitrates, and other antihypertensives. Unadjusted estimates (not shown) for the relationship between UFR (10–13 and > 13 ml/h/kg, respectively) and outcomes were: 0.88 (0.76–1.03; P = 0.13) and 1.21 (1.05–1.40; P = 0.01) for CV hospitalization and all-cause mortality; 0.90 (0.76–1.08; P = 0.26) and 1.23 (1.05–1.45; P = 0.01) for CV hospitalization and CV-related mortality; and 0.88 (0.73–1.06; P = 0.18) and 1.14 (0.96–1.36; P = 0.13) for CV hospitalization. Abbreviations: ref., reference; CI, confidence interval.
