Abstract
Purpose
As the population in developed countries continues to age, the incidence of osteoporotic distal radius fractures (DRFs) will increase as well. Treatment of DRF in the elderly population is controversial. We systematically reviewed the existing literature for the management of DRFs in patients 60 and over with five common techniques: volar locking plate system (VLPS), non-bridging external fixation (non-BrEF), bridging external fixation (BrEF), percutaneous Kirschner-wire fixation (PKF), and cast immobilization (CI).
Methods
Articles retrieved from MEDLINE, Embase and CINAHL Plus that met predetermined inclusion and exclusion criteria were reviewed in two literature reviews. Outcomes of interest included wrist arc of motion, grip strength, functional outcome measurements, radiographic parameters, and the number and type of complications. The data were statistically analyzed using weighted means and proportions based on the sample size in each study.
Results
2,039 papers were identified, and 21 papers fitting the inclusion criteria were selected in the primary review of articles with mean patient age of 60 and over. Statistically significant differences were detected for wrist arc of motion, grip strength, and DASH score, although these findings may not be clinically meaningful. Volar tilt and ulnar variance revealed significant differences amongst the groups, with CI resulting in the worst radiographic outcomes. The complications were significantly different, with CI having the lowest rate of complications, whereas VLPS had significantly more major complications requiring additional surgical intervention.
Conclusions
This systematic review suggests that despite worse radiographic outcomes associated with CI, functional outcomes were no different than surgically treated groups for patients 60 and over. Prospective comparative outcomes studies are necessary to evaluate the rate of functional recovery, cost, and outcomes associated with these 5 treatment methods.
Level of Evidence
Therapeutic, Level III
Keywords: distal radius fracture, elderly, systematic review, outcomes
Distal radius fractures (DRFs) are the most common fractures seen by physicians.1–4 In the younger population, these fractures are most often the result of high-energy trauma such as motor vehicle accidents or falls from heights. In the elderly population, however, these fractures frequently result from falls from a standing height and other low-energy trauma. DRFs are the second most common fracture suffered by the elderly, after hip fractures.5 Approximately 10% of 65-year-old white women will suffer a DRF during their remaining lifetime.5 The annual incidence of DRF in the US population over the age of 65 has been reported as 57 to 100 per 10,000.4–6 There are over 37 million individuals 65 years of age and older in the US.7 Thus, we can extrapolate that as many as 372,000 individuals 65 years of age and over sustain this type of fracture every year. This number will only rise in the future because the Baby-Boomers are beginning to age and elderly individuals are living longer and lead healthier, more active lives than any previous generation.
The optimal treatment for osteoporotic DRFs is controversial. These fractures may be comminuted and associated with several fracture fragments.8 DRFs in older patients have traditionally been treated with closed reduction and cast immobilization (CI).9, 10 This method of treatment fails to maintain reduction and results in malunion in over 50% of cases.11, 12 However, malunion often does not affect functional outcomes, and many elderly patients have satisfactory functional results despite imperfect anatomical healing.11–16 Other conventional treatments such as percutaneous fixation with Kirschner-wires (PKF), direct skeletal external fixation with bridging fixators (BrEF) and external fixation with non-bridging fixators (non-BrEF) result in fewer malunions and also have satisfactory functional results.17–23 The increasing popularity of the volar locking plating system (VLPS) has been shown to give equivalent outcomes for young and elderly patients.24
In the face of uncertainty in considering competing treatment choices, a systematic review is helpful to synthesize the best evidence from the literature when randomized controlled trial data are not available.25 In this study, we systematically reviewed outcome and complication data for five common treatment options for DRF: CI, PKF, BrEF, non-BrEF, and VLPS. The population of interest in this systematic review are those 60 years or older.
Materials and Methods
Literature search
A search of the English language literature published from January 1980 to July 2009 was performed using MEDLINE and CINAHL Plus to identify citations related to DRF. The following search MeSH terms were used: radius fractures OR wrist injuries OR distal radius (radial) fractures OR wrist fractures OR Colles fractures OR Smith fractures.26 A secondary search was performed within the results of the primary search with MeSH terms, fracture fixation OR orthopedic fixation devices. A title and abstract search then was conducted to identify appropriate articles using criteria developed a priori (Table 1). A manual reference check of the retrieved articles was performed to identify additional references not captured by the original search.
Table 1.
Inclusion Criteria for Systematic Literature Review on Unstable DRFs.
|
Our primary literature search was deliberately broad so that we could capture the most information available. However, studies with a mean age of 60 or older may be confounded by younger patients. Thus, a separate secondary literature search was performed with more stringent search criteria as an internal test of validity. This search was performed in MEDLINE, Embase, and CINAHL Plus in the same date range with the following MeSH terms: radius fractures OR distal radius fractures OR wrist fractures OR Colles fractures OR Smith fractures. A secondary search was performed within this separate group of abstract results using: (fracture fixation OR orthopedic fixation OR fracture management) AND (elderly OR elder OR geriatric OR osteoporotic).
Inclusion and Exclusion Criteria
Because we were examining outcomes following unstable fractures, citations were only included if fractures fit at least one of the criteria indicated in Table 1.24, 27 We excluded articles from review if they met any of the following criteria: (1) fewer than 10 patients, (2) no information provided about the number of patients lost to follow-up, (3) complications not reported, (4) studies including a surgical technique that combined the use of an external fixator and plate fixation in the same patient, (5) studies including non-standard procedures such as functional casting or intramedullary wire fixation, or (6) studies of fractures associated with either fractures of the distal ulna (not including isolated fractures of the styloid process), fractures of carpal bones, dislocation of the distal radioulnar joint, fractures with vascular injury, or open fractures.28 In our second literature search, we added the additional criterion excluding studies that included any patients under the age of 60 to eliminate possible confounding effect of younger patients.
Data Extraction and Analysis
The data extracted from the studies included patient demographic information, fracture-type classifications, treatment technique, time period of wrist immobilization, type of supplemental wrist immobilization (i.e. splinting after VLPS or casting in addition to PKF), functional outcomes, radiographic parameters, and the number and type of complications and their treatments. Functional outcomes data included wrist and forearm motion and grip strength. We also extracted the results of objective or self-assessment scoring systems for the function of the hand, wrist or upper extremity, activities of daily living (ADLs) or other outcomes. Radiographic parameters included volar tilt, radial inclination, radial height, radial shortening and ulnar variance. We categorized complications into three groups; minor, major not requiring surgery, and major requiring surgery. Minor complications consisted of superficial infection, blistering, and loosening of pins. Persistent nerve lesions, complex regional pain syndrome and early removal of pins were assigned to major complications not requiring surgery. Major complications requiring surgery included tendon rupture, deep infection, continuous carpal tunnel syndrome, and any complication requiring a secondary surgical procedure to correct.29
Statistical Analysis
Heterogeneity is a concern in any review of this type, which is influenced by the underlying differences in patient samples, study design, or data analysis that can result in variations in outcomes among studies. Variations caused by heterogeneity can obscure the differences that we attribute to the particular treatment type. In studies of DRF treatment, outcome heterogeneity may be caused by differences in patient selection, patient age, fracture severity, variations in surgical technique, postoperative rehabilitation, outcome measurement methods, length of follow-up period, and the number of patients loss to follow-up.27 For this systematic review, we considered the number of fractures, the rate of intra-articular fractures, mean patient age, and the length of the follow-up time as potential sources of heterogeneity and analyzed these factors using analysis of variance (ANOVA) and the chi-square test.
The weighted means of continuous outcome measures were calculated across available studies for each treatment option.30 Wrist motion, grip strength, radiographic parameters, and DASH scores from available articles were pooled together by generating the weighted means for all factors. Significance level was set at p=0.05. If significant differences were detected, multiple comparisons of the five treatment options were performed using Tukey Style Multiple Comparisons test.
Quality assessment of the literature
Each article was evaluated using both the Structured Effectiveness Quality Evaluation Scale (SEQES) and Sackett’s Level of Evidence.(Appendices 1 and 2, respectively)58–60 The SEQES appraises the overall quality of a study based on study design, subject accrual, intervention, outcomes, analysis, and recommendations. Each category is further broken down into individual criteria, with each criterion scored 0–2. A score of 0 indicates that the criterion has not been met, a score of 1 indicates that it has been partially met, and a score of 2 indicates that the criterion has been fully met. A total score of 33 or above indicates a high quality study.59 The authors reviewed each of the studies, assigning scores to each criterion and a level of evidence (LOE) rank.
Appendix 1.
Structured Effectiveness Quality Evaluation Scale (SEQES)
Score each question 0–2 (Higher score indicated higher quality)
| Study question |
| 1. Was the relevant background work cited to establish a foundation for the research question? |
| Study design |
| 2. Was a comparison group used? |
| 3. Was patient status at more than one time point considered? |
| 4. Was data collection performed prospectively? |
| 5. Were patients randomized to groups? |
| 6. Were patients blinded to the extent possible? |
| 7. Were treatment providers blinded to the extent possible? |
| 8. Was an independent evaluator used to administer outcome measures? |
| Subjects |
| 9. Did sampling procedures minimize sample/selection bias? |
| 10. Were inclusion/exclusion criteria defined? |
| 11. Was an appropriate enrollment contained? |
| 12. Was an appropriate retention/follow-up obtained? |
| Intervention |
| 13. Was the intervention applied according to established principles? |
| 14. Were biases due to the treatment provider minimized (i.e. attention, training, etc)? |
| 15. Was the intervention compared to appropriate comparator? |
| Outcomes |
| 16. Was an appropriate primary outcome defined? |
| 17. Were appropriate secondary outcomes considered? |
| 18. Was an appropriate follow-up period incorporated? |
| Analysis |
| 19. Was an appropriate statistical test(s) performed to indicate differences related to the intervention? |
| 20. Was it established that the study had significant power to identify treatment effects? |
| 21. Was the size and significance of the effects reported? |
| 22. Were missing data accounted for and considered in the analyses? |
| 23. Were the cliwenical and practical significance considered in interpreting results? |
| Recommendations |
| 24. Were the conclusions/clinical recommendations supported by the study objectives, analysis and results? |
| Total quality score = |
Appendix 2.
Sackett’s Levels of Evidence
| Level of Evidence | General criteria for LOE |
|---|---|
| I | Single high-quality randomized, controlled trial (RCT) or systematic review of homogenous RCTs |
| II | Single cohort study, low-quality RCT (i.e. less than 80% follow-up), or systematic review of cohort studies |
| III | Case-control studies |
| IV | Case series, low-quality cohort and case-control studies |
| V | Expert opinion without critical appraisal |
Results
Study Retrieval and Characteristics
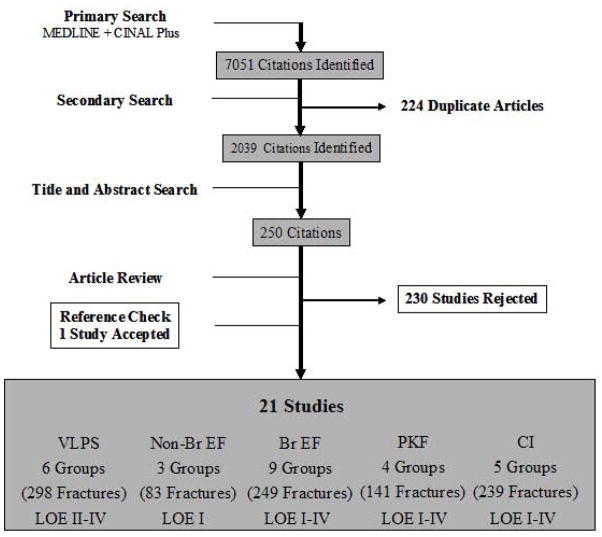
After eliminating non-relevant and duplicate articles, our extensive primary literature search identified 2,039 citations. After a title and abstract search, 250 citations remained. Ultimately, 21 articles, comprising 27 groups of patients, met the inclusion and exclusion criteria (Figure 1). Selected articles and study characteristics are listed in Table 2. Of the included studies, 8 were randomized controlled trials,18, 41, 48, 50, 51, 53–55 3 were prospective cohort studies,24, 44, 49 and 10 were retrospective case series.13, 15, 29, 42, 43, 45–47, 52, 56, 57 Fifteen of the 21 studies were single institution studies. In eight studies, the operations were performed by or under the supervision of a single surgeon. Our secondary literature search was more specific in its search terms, so it identified only 504 citations. The final result of the secondary literature search was comprised of 8 articles with 12 groups of patients. Three of those articles were Level I randomized controlled trials (RCTs), 1 was a Level II prospective cohort studies (PCSs) and the remaining 4 were case series. Seven of those 8 articles were captured in our first literature search.
Figure 1.
Identification of studies in the primary literature search
Footnote - VLPS: Patient groups are derived from studies with Levels of Evidence ranging from Level II to Level IV; Non-Br EF: Patient groups are derived from studies with Level of Evidence Level I; Br EF, PKF, CI: Patient groups are derived from studies with Levels of Evidence ranging from Level I to Level IV
Table 2.
Study Characteristics
| First Author | Year | Procedure* | N | Study design | Level of Evidence | SEQES^ Score (0–48) | Institutional setting | Surgeons |
|---|---|---|---|---|---|---|---|---|
| Atroshi18 a, b | 2006 | Non-BrEF, BrEF | 38 | RCT | I | 38 | Single site | Unknown |
| Azzopardi41a, b | 2005 | PKF, CI | 57 | RCT | I | 38 | Single site | Single |
| Krukhaug48a | 2009 | Non-BrEF, BrEF | 75 | RCT | I | 41 | Multicenter | Multiple |
| McQueen51a | 1996 | BrEF, CI | 90 | RCT | I | 37 | Single site | Multiple |
| McQueen50 a | 1998 | Non-BrEF, BrEF | 60 | RCT | I | 39 | Single site | Single |
| Sanchez-Sotelo54 a, b | 2000 | CI | 55 | RCT | I | 31 | Single site | Single |
| Schmalholz55a | 1990 | BrEF | 25 | RCT | I | 30 | Single site | Single |
| Chung24 a, b | 2008 | VLPS | 25 | PCS | II | 34 | Single site | Single |
| Gerald44 a | 2008 | VLPS | 55 | PCS | II | 24 | Single site | Single |
| Lattmann49 a | 2009 | VLPS | 91 | PCS | II | 34 | Single site | Unknown |
| Pritchett53 a | 1995 | BrEF | 50 | RCT | II | 21 | Single site | Single |
| Arora13 a, b | 2009 | VLPS, CI | 114 | Case series | IV | 28 | Single site | Multiple |
| Cannegieter42a | 1997 | BrEF | 32 | Case series | IV | 15 | Single site | Unknown |
| Drobetz43 a | 2003 | VLPS | 50 | Case series | IV | 13 | Single site | Unknown |
| Fujii45 b | 2002 | PKF | 22 | Case series | IV | 17 | Single site | Unknown |
| Hede46 a | 2000 | PKF | 42 | Case series | IV | 17 | Single site | Unknown |
| Hegeman47 a, b | 2005 | BrEF | 16 | Case series | IV | 17 | Single site | Unknown |
| Orbay52 a, b | 2004 | VLPS | 24 | Case series | IV | 21 | Multicenter | Multiple |
| Shiota56 a | 2003 | PKF | 37 | Case series | IV | 18 | Single site | Unknown |
| van Aaken29a | 2008 | PKF | 34 | Case series | IV | 21 | Unknown | Unknown |
| Young15 a, b | 2003 | CI | 25 | Case series | IV | 18 | Multicenter | Multiple |
| Ziran57 a | 2000 | BrEF | 10 | Case series | IV | 14 | Single site | Single |
VLPS: volar locking plate system, non-BrEF: non-bridging external fixation, BrEF: bridging external fixation, PKF: percutaneous Kirschner-wire fixation, CI: cast immobilization
SEQES: Structured Effectiveness Quality Evaluation Scale; low quality (<16), moderate quality (17–32), high quality (33–48).
Primary Literature Search
Secondary Literature Search
Table 2 displays the breakdown of the levels of evidence of the available literature in our review. Of all the papers that met our inclusion criteria in our primary literature review, 7 were LOE I, 4 were LOE II, and the remaining articles were level IV case series. The SEQES scores varied from 13–41, with a mean of 25.6, out of 40. Appendix 1 illustrates the distribution of SEQES criteria met by all of the included articles, ranging from 0% in regards to blinded patients or treatment providers to 100% in regards to appropriate follow-up. Only 9% established that the study had significant power to identify treatment effects.
Patient and Fracture Characteristics
Patient, fracture and treatment characteristics are indicated in Table 3. The number of patients (p=0.86), mean patient age (p=0.71), and mean follow-up period (p=0.48) were comparable amongst the five treatment methods. There was a significant difference amongst the 5 groups with regard to the proportions of intra-articular fractures (p<0.001); the VLPS group was comprised of 64% intra-articular fracture, whereas the PKF group had only 24% intra-articular fractures. In the Non-BrEF and BrEF groups, the fixation devices were commonly applied for 6 weeks. Below-elbow casts were also applied for 6 weeks in the majority of patients treated with CI. In 92% of patients treated with VLPS, an additional splint or short arm cast was used for 2 to 4 weeks. For PKF, an additional splint was used for 3 to 6 weeks.
Table 3.
Patient and Fracture Characteristics
| Procedure | First Author | No. of Patients | No. of Fractures | Female (%) | Intraarticular Fracture (%) | Mean Age (yr) | Mean Follow-Up (mo) | Period of Wrist Immobilization | Type of Supplemental Wrist Immobilization |
|---|---|---|---|---|---|---|---|---|---|
| VLPS | Arora13 | 53 | 53 | 36 (68%) | 25 (47%) | 76 | 52 | 2wks | Splint |
| Chung24 | 25 | 25 | 19 (76%) | 12 (48%) | 69 | 12 | 6wks | Splint | |
| Drobetz43 | 49 | 50 | 40 (82%) | 34 (68%) | 62 | 26 | 2wks* | Splint* | |
| Gerald44 | 55 | 55 | 37 (67%) | 55 (100%) | 60 | 29 | 4wks | Cast | |
| Lattmann49 | 91 | 91 | 73 (80%) | 57 (63%) | 64 | 12 | 1–4wks | Cast | |
| Orbay52 | 23 | 24 | 17 (74%) | 8 (33%) | 79 | 15 | - | - | |
|
|
|||||||||
| Total | 296 | 298 | 222 (75%) | 191 (64%) | 67 | 25 | - | - | |
|
|
|||||||||
| Non-BrEF | Atroshi18 | 18 | 18 | 16 (89%) | 8 (44%) | 70 | 12 | 6wks | - |
| Krukhaug48 | 35 | 35 | - | 0 | 62 | 12 | 6wks | - | |
| McQueen50 | 28 | 30 | 27 (96%) | 9 (30%) | 62 | 12 | 6wks | - | |
|
|
|||||||||
| Total | 84 | 83 | - | 17 (20%) | 64 | 12 | - | - | |
|
|
|||||||||
| BrEF | Atroshi18 | 18 | 19 | 15 (83%) | 11 (58%) | 71 | 12 | 6wks | - |
| Cannegieter42 | 32 | 32 | 27 (84%) | 19 (59%) | 68 | 36 | 5wks | - | |
| Hegeman47 | 16 | 16 | 16 (100%) | 16 (100%) | 67 | 48 | 6wks | - | |
| Krukhaug48 | 37 | 37 | - | 0 | 62 | 12 | 6wks | - | |
| McQueen50 | 28 | 30 | 28 (100%) | 5 (17%) | 61 | 12 | 6wks | - | |
| McQueen51 | 28 | 30 | 25 (89%) | 16 (53%) | 63 | 12 | 5wks | - | |
| Pritchett53 | 50 | 50 | 26 (52%) | 50 (100%) | 65 | 24 | 6wks | - | |
| Schmalholz55 | 25 | 25 | 24 (96%) | 0 | 66 | 12 | 5wks | - | |
| Ziran57 | 10 | 10 | - | 10 (100%) | 62 | 29 | 8wks | - | |
|
|
|||||||||
| Total | 244 | 249 | - | 127 (51%) | 65 | 20 | - | - | |
|
|
|||||||||
| PKF | Azzopardi41 | 27 | 27 | 23 (85%) | 0 | 72 | 12 | unknown | Cast |
| Fujii45 | 22 | 22 | 21(95%) | 14(64%) | 69 | 24 | 5wks | Unknown | |
| Hede46 | 42 | 43 | 31(74%) | 0 | 61 | 33 | 5wks | Splint | |
| van Aaken29 | 34 | 34 | 26 (76%) | 19 (56%) | 63 | 30 | 6wks | Splint | |
| Shiota56 | 37 | 37 | 11 (30%) | 15 (41%) | 66 | 28 | 3wks | Splint | |
|
|
|||||||||
| Total | 162 | 163 | 112 (69%) | 48 (29%) | 66 | 25 | - | - | |
|
|
|||||||||
| CI | Arora13 | 61 | 61 | 42 (69%) | 30 (49%) | 81 | 62 | 6wk | - |
| Azzopardi41 | 27 | 27 | 25 (93%) | 0 | 71 | 12 | 5wk | - | |
| McQueen51 | 30 | 30 | 28 (93%) | 19 (63%) | 64 | 12 | 6wk | - | |
| Sanchez-Sotelo54 | 55 | 55 | 49 (89%) | 20 (36%) | 67 | 12 | 6wk | - | |
| Young15 | 66 | 66 | 58 (89%) | 9 (14%) | 60 | 84 | 6wk | - | |
|
| |||||||||
| Total | 239 | 239 | 203 (85%) | 78 (33%) | 69 | 45 | - | - | |
Immobilization for AO type C fractures only
Functional Outcomes
Wrist and forearm motions were inconsistently presented and were expressed as degrees, percentage of the contralateral hand or difference from the contralateral hand. We used the 11 citations from our primary literature review that listed motion at final follow-up in degrees to calculate the weighted mean (Table 4). There were statistically significant differences in flexion/extension of the wrist (p<0.001) and rotation of the forearm (p<0.001) amongst the 5 methods. There was insufficient data in the secondary literature review to analyze weighted means on active motion. Grip strength at final follow-up was reported in 13 studies (Table 5). Grip strength at final follow-up was not significantly different (p=0.71) amongst the five methods in our primary literature search. However, there was a significant difference (p<0.001) between VLPS/PKF and VLPS/CI in our secondary literature search.
Table 4.
Active Arc of Motion of the Wrist and Forearm at Final Follow-up (Weighted Mean)
| VLPS (n=218) | Non-BrEF (n=18) | BrEF (n=28) | PKF (n=68) | CI (n=137) | p value | |
|---|---|---|---|---|---|---|
| Wrist flexion/extension arc (degrees) | 118 | 118 | 116 | 112 | 130 | 0.68a |
| Forearm rotation arc (degrees) | 168 | 168 | 153 | 140 | 175 | 0.15a |
Note: p values were calculated using ANOVA
Primary Literature Review
Table 5.
Grip Strength at Final Follow-up (Weighted Mean)
| Grip strength (% compared with contralateral ) | VLPS (n=235) | Non-BrEF (n=28) | BrEF (n=138) | PKF (n=95) | CI (n=220) | p value |
|---|---|---|---|---|---|---|
| Primary literature review | 81 | 69 | 84 | 74 | 85 | 0.707 |
| Secondary literature review | 76 | - | - | 83 | 84 | <0.001 |
Note: p value was calculated using ANOVA.
The Non-BrEF and BrEF could not be compared via ANOVA to the other groups because only 1 paper at most was present for analysis.
Significant difference (95% confidential level using Tukey Style Multiple Comparisons test) were found between the following treatment groups: VLPS/PKF, VLPS/CI.
Various objective and subjective scoring systems were also used (Table 6). The Disability of Arm, Shoulder and Hand (DASH) was used as an outcomes measure in 5 studies. There was a significant difference (p<0.001) when the weighted mean DASH score was compared amongst VLPS, non-BrEF, BrEF, and CI in our primary literature search. Similar analysis was not possible in our secondary search.
Table 6.
Final Number of Patients and Fracture, and Result of Scoring System
| Procedure | First Author | No. of Patients at final follow-up | No. of Fractures at final follow-up | Scoring system (name: % of patients receiving excellent and good scores or mean points scored) |
|---|---|---|---|---|
| VLPS | Arora13 | 53 | 53 | Green and O’Brien: 74%; DASH: 11.1/100*; PRWE: 9.3/100* |
| Chung24 | 17 | 17 | MHQ: 85/100 | |
| Drobetz43 | 49 | 50 | Cooney: 68%; Sarmiento: 92% | |
| Gerald44 | 55 | 55 | Gartland and Werley: 80%; DASH: 7.1/100* | |
| Lattmann49 | 86 | 86 | ||
| Orbay52 | 23 | 24 | DASH: 8.2/100* | |
| Non-BrEF | Atroshi18 | 18 | 18 | DASH: 11/100*; SF-12: 49/100 |
| Krukhaug48 | 35 | 35 | DASH: 9/100* | |
| McQueen50 | 28 | 28 | ||
| BrEF | Atroshi18 | 18 | 18 | DASH: 7/100*; SF-12: 48/100 |
| Cannegieter42 | 32 | 32 | Sarmiento: 100% | |
| Hegeman47 | 16 | 16 | Gartland and Werley: 63% | |
| Krukhaug48 | 37 | 37 | DASH: 13/100* | |
| McQueen50 | 28 | 28 | ||
| McQueen51 | 28 | 28 | ||
| Pritchett53 | 50 | 50 | Lindstrom: 84% | |
| Schmalholz55 | 25 | 25 | Lindstrom: 84% | |
| Ziran57 | 10 | 10 | PRWE: pain - 11/100*, disability - 9.8/100* | |
| PKF | Azzopardi41 | 27 | 27 | Sheehan’s ADL: unilateral – 7.6/8, bilateral - 9.7/12 |
| Fujii45 | 22 | 22 | Saito: 91% | |
| Hede46 | 42 | 43 | Luca: 93% | |
| Shiota56 | 37 | 37 | ||
| van Aaken29 | 25 | 25 | Gartland and Werley: 85% | |
| CI | Arora13 | 61 | 61 | Green and O’Brien: 85%; DASH: 11.6/100*; PRWE: 16.9/100* |
| Azzopardi41 | 27 | 27 | Sheehan’s ADL: unilateral – 7.4/8, bilateral - 9.4/12 | |
| McQueen51 | 28 | 28 | ||
| Sanchez-Sotelo54 | 55 | 55 | Cooney: 55% | |
| Young15 | 49 | 49 | Gartland and Werley: 96% |
DASH: Disability of Arm, Shoulder and Hand; PRWE: Patient-Related Wrist Evaluation; MHQ: Michigan Hand Outcomes Questionnaire
Higher score equals greater disability
Radiographic Outcome
Volar tilt was evaluated in 22 of the 27 patient groups in the primary literature search and all patient groups in the secondary search. Radial inclination and ulnar variance were reported less frequently. Amongst radial height, radial shortening, and ulnar variance to evaluate shortening of the distal radius, only ulnar variance was evaluated in all five treatment options. Volar tilt, radial inclination, and ulnar variance at final follow-up are shown in Table 7 for both literature searches. Treatment with CI resulted in the most severe dorsal angulation and shortening of the distal radius in both literature searches (volar tilt = −11°; ulnar variance = +3.6mm). VLPS, non-BrEF and PKF indicated positive values for volar tilt: 4°, 7° and 4° respectively. Three treatment options also resulted in ulnar variance under +2mm (VLPS = +1.5mm; non-BrEF = +1.0; BrEF = +1.0mm). There were significant differences in volar tilt (p<0.001), radial inclination (p<0.001), and ulnar variance (p<0.001) amongst the 5 treatment groups. Multiple comparison analysis demonstrated there were significant differences in volar tilt between CI and all other treatment groups (p<0.001). Ulnar variance was significantly different between PKF and other options and between CI and others (p<0.001). Similar results were obtained between the analyses of the radiographic outcomes of our two literature searches with the exception of two key points (Table 7). First, we were unable to analyze the non-bridging external fixator group in our secondary literature search because of insufficient data Second, radial inclination measurements showed significant differences between the groups in our secondary literature search, with the VLPS mean at 23° and the CI mean at 18° (p < 0.001) as the maximum and minimum values, respectively.
Table 7.
Radiographic Parameters at Final Follow-up (Weighted Mean)
| VLPS | Non-BrEF | BrEF | PKF | CI | p value | ||
|---|---|---|---|---|---|---|---|
| Volar Tilt (degrees) | Primary literature review | 3.9 (n=235) | 6.5 (n=81) | −0.8 (n=169) | 3.7 (n=52) | −11 (n=220) | 0.018 |
| Secondary literature review | 3.1 (n=94) | - | 0.3 (n=35) | 0.5 (n=49) | −11 (n=168) | <0.001 | |
| Radial Inclination (degrees) | Primary literature review | 13.4 (n=149) | 13.7 (n=53) | 13.9 (n=113) | 21 (n=52) | 14.8 (n=137) | 0.182 |
| Secondary literature review | 22.8 (n=94) | - | 19.5 (n=35) | 21 (n=49) | 18.0 (n=168) | <0.001 | |
| Ulnar Variance (mm) | Primary literature review | 1.5 (n=53) | 1.0 (n=53) | 1.1 (n=81) | 3.0 (n=27) | 3.6 (n=143) | <0.001 |
| Secondary literature review | 1.5 (n=53) | - | 2.4 (n=35) | 3.0 (n=49) | 3.6 (n=143) | <0.001 |
Note: p values were calculated using ANOVA.
Significant difference (95% confidential level using Tukey Style Multiple Comparisons test) were found between the following treatment groups for the following variables in the primary literature review: Volar Tilt – VLPS/CI, Non-BrEF/CI; Ulnar Variance – VLPS/BrEF, VLPS/CI, Non-BrEF/CI
Significant difference (95% confidential level using Tukey Style Multiple Comparisons test) were found between the following treatment groups for the following variables in the secondary literature review: Volar Tilt – VLPS/CI, BrEF/CI, PKF/CI; Radial Inclination – all groups were significantly different; Ulnar Variance – All groups significantly different except for BrEF/CI.
The Non-BrEF could not be compared via ANOVA in the secondary literature review to the other groups because only 1 paper was present for analysis.
Complications
Complications are listed in Table 8. The most common minor complication was superficial pin-track infection in patients treated with non-BrEF, BrEF, and PKF. Sixty-three of the 77 major complications not requiring surgery were complex regional pain syndrome and nerve lesions. Injured nerves included the superficial branch of the radial nerve, ulnar nerve, the median nerve, and its palmar cutaneous branch. The most common major complication requiring surgery was rupture or adhesion of the flexor pollicis longus tendon and/or the extensor pollicis longus tendon. Four patients experienced carpal tunnel syndrome requiring surgical intervention. In 8 cases in the VLPS group, hardware removal was performed as an additional operation due to loosening, failure or patient request.
Table 8.
Summary of Complications
| VLPS | Non-BrEF | BrEF | PKF | CI | p value | ||
|---|---|---|---|---|---|---|---|
| Minor | Superficial infection | 0 | 25 | 39 | 2 | 0 | |
| Others | 2 | 0 | 0 | 9 | 0 | ||
| Total (%) | 2 (1%) | 25 (31%) | 39 (16%) | 11 (8%) | 0 | <0.001 | |
| Major not requiring Surgery | Nerve lesion | 6 | 1 | 10 | 4 | 4 | |
| CRPS | 9 | 0 | 16 | 2 | 11 | ||
| Early hardware removal | 0 | 0 | 6 | 3 | 0 | ||
| Others | 3 | 0 | 2 | 0 | 0 | ||
| Total (%) | 18 (6%) | 1 (1%) | 34 (14%) | 9 (7%) | 15 (7%) | <0.001 | |
| Major requiring Surgery | Tendon rupture/adhesion | 18 | 2 | 0 | 3 | 3 | |
| Nerve lesion | 2 | 0 | 2 | 0 | 0 | ||
| Infection | 2 | 0 | 1 | 0 | 0 | ||
| Hardware loosening, failure or removal | 8 | 0 | 0 | 0 | 0 | ||
| Others | 2 | 0 | 2 | 0 | 0 | ||
| Total (%) | 32 (11%) | 2 (3%) | 5 (2%) | 3 (2%) | 3 (1%) | <0.001 |
Note: p values were calculated using the chi-square test. Significant differences were found between the all treatment groups except the following pairs: major, not requiring surgery –PKF/CI; major, requiring surgery – Non-BrEF/PKF, BrEF/PKF.
There were significant differences in the rates of all types of complications among the 5 treatment options, with BrEF resulting in the highest proportion of minor and major complications not requiring surgery, whereas VLPS resulted in the highest proportion of major complications requiring surgery. Non-invasive CI resulted in the lowest proportion of complications in all categories.
Discussion
In the present study, we reviewed over 2,000 citations from three large databases in order to evaluate the functional outcomes, radiographic parameters, and complications of the five most common treatment methods for unstable DRFs in the elderly. Our systematic review revealed that motion after each treatment option was statistically different, when measured at least 12 months following injury. Functional range of wrist flexion and extension for ADLs, however, were 54° and 60° respectively. 31 Therefore, wrist motion was clinically comparable because the final motions (regardless of the treatment method) were between 116° and 133°. DASH scores were also significantly different among the four treatment groups except PKF, but not clinically different because the difference was only 2.5 or less out of 100 points. There were significant differences in some radiographic parameters, namely volar tilt and ulnar variance. Specifically, treatment with VLPS or Non-BrEF resulted in significantly better volar tilt and ulnar variance when compared to treatment with CI. This was not unexpected, because it is well known that fractures treated conservatively are prone to collapse.11, 12 VLPS prevents this by using fixed-angle screws to hold the fragment in place, whereas Non-BrEF can directly support the distal fragments through pins, which are secured to the device. It is also well known that wrist function is not related to wrist deformity in elderly patients, lending credence to our finding that there were no clinically significant functional differences amongst the 5 treatment methods, as measured by the DASH and motion despite the significant differences in radiographic parameters.15, 16, 32
Recent randomized controlled studies of unstable DRFs, not restricted to the elderly, demonstrated that both wrist function and DASH scores in groups treated with VLPS were comparable with those treated with BrEF, radial column plate, and PKF one year after surgery.33, 34 VLPS, however, leads to better wrist motion and DASH score in the first 6 to 12 weeks after surgery. We found that the period of immobilization, which allowed patients limited or no wrist movement, and the types and rates of complications were also different amongst the five strategies in the present review. The rate of recovery and limitations of ADL during treatment affect the quality of life of patients with DRFs. Compared to younger patients, the elderly already experience a delay of approximate 6-month in gaining functional improvement.24 These findings imply that rate of recovery of ADL performance and the possibility of major complications during recovery may be more important factors than the final functional outcome when deciding which treatment strategy is best for elderly patients with DRFs. A decision analysis, which compares the utility of, or preference for, each treatment option from the perspective of elderly individuals themselves, may serve as a reference for decision-making based on risk-benefit ratio that the elderly population places on each intervention.
Our results were limited by the strength of available evidence. Heterogeneity exists amongst the five groups in many characteristics, including indications of surgery, manipulation of redisplaced fractures and fracture type. Most notably, there are significant differences in the proportions of intra-articular fractures amongst the groups, although we were unable to determine the influence of these confounding factors on outcomes at final follow-up because of insufficient information on patients’ loss to follow-up. On the other hand, it remains controversial whether experiencing an intra-articular fracture, or the subsequent osteoarthritis of the radiocarpal joint that frequently occurs following this type of fracture, greatly affects long-term function of the wrist.13, 35–37 In future research, it would be prudent to distinguish between outcomes of extra-articular and intra-articular fractures, including coronal split fracture or Barton’s fracture, which generally require management with open reduction and internal fixation.32, 38
Another limitation of our primary data analysis is that the primary literature search inclusion criteria required only a mean age of 60 for each study’s patient sample, not that all the patients in each series be over the age of 60. We did this because we also included a minimum follow-up period of 12 months, limiting our results to only 21 citations. However, to serve as an internal test of validly, we redid our literature search and analysis with more stringent criteria to isolate journal articles with study populations comprised completely of elderly patients. Even with the addition of a third database, this reduced the number of citations in our secondary literature search to 8. This greatly impacted our ability to analyze and compare important aspects of DRF outcomes such as motion, standardized functional scores and complications. In comparing radiographic outcomes, the results between the analyses of the primary and secondary literature searches were similar (Table 7) in showing that operative management is superior to CI in maintaining volar tilt and preventing radial shortening. We feel that this similarity between the analyses of our two literature searches adds validity to the assumptions we made in broadening our search to studies with a mean age of 60 or older in our original inclusion/exclusion criteria. Thus, we are confident in using our primary literature search analysis in the description of the variability between the 5 treatment options in regards to motion, DASH score and complications.
Another limitation is that 10 retrospective case series were included in this systematic review. A systematic review of randomized controlled trials or cohort study is ranked as a higher level of evidence. However, the importance of systematic review relies on the methodological search for the underlying causes of heterogeneity, which allows the authors to make evidence-based recommendations for future investigations. 39 Therefore, the present analysis uses all available evidence in the literature to yield the pooled data for comparative purposes to propose necessary follow-up studies.
Even with the inclusion of these retrospective case series, the mean SEQES score was 25.6, out of 48, reflecting our stringent inclusion criteria for 12-month follow-up, complications, and functional and radiologic assessments. Although the SEQES is a subjective measure of quality, it does lend some merit to the studies included and also draws attention to some flaws in our literature. Blinding treatment providers and patients remains a difficult issue to address in the field of surgical outcomes research, but others seem much easier to improve. Only 9% of studies had established that they had sufficient power to detect treatment effects, and 41% had independent evaluators assess function or radiologic outcomes. This study reflects inadequacies in our current literature that can only be attended to if they are acknowledged going forward.
There remains no consensus regarding the appropriate treatment for unstable DRFs in elderly patients. Consequently, indications for surgical intervention are judged individually based on the balance of risk and benefit. If there is no great difference between functional outcomes and ADL one year after injury, factors that affect quality of life during recovery such as pain, the rate of recovery, limitation of ADLs, and potential complications will be more critical in deciding the treatment strategy. Quality of life depends on individuals’ activities, lifestyles and preferences, rather than age. Nevertheless, it seems age, as well as geography, influence the selection of treatment methods for DRF.9, 40 The use of internal fixation is on the rise, yet there have been no large-scale randomized controlled trials to compare VLPS to other treatments in elderly patients. Although there is some evidence that outcomes of VLPS are as good in elderly patients as those in young patients,24 there is no proof that these outcomes justify this more invasive, and likely more expensive, procedure. The definite answer regarding the optimal management of the growing incidence of DRFs in the elderly demands the conduct of multicenter clinical trials to better define the best practice in treating this prevalent injury.
Figure 2.
Summation of Quality of Evidence—Percent of studies meeting each SEQES criteria
Acknowledgments
We would like to thank Philip J. Clapham for his help organizing this manuscript, and Heidi Reichert and Soo Young Kwak for their help with the statistical analysis. Supported in part by a Clinical Trial Planning Grant (R34 AR055992-01), an Exploratory/Developmental Research Grant Award (R21 AR056988) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (To Dr. Kevin C. Chung)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Solgaard S, Petersen VS. Epidemiology of distal radius fractures. Acta Orthop Scand. 1985;56:391–393. doi: 10.3109/17453678508994354. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill TW, Cooper C, Finn JD. Incidence of distal forearm fracture in British men and women. Osteoporos Int. 2001;12:555–558. doi: 10.1007/s001980170076. [DOI] [PubMed] [Google Scholar]
- 3.Owen RA, Melton LJI. Incidence of Colles’ fracture in a North American community. Am J Public Health. 1982;72:605–607. doi: 10.2105/ajph.72.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg. 1998;80B:243–248. doi: 10.1302/0301-620x.80b2.7762. [DOI] [PubMed] [Google Scholar]
- 5.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. [PubMed] [Google Scholar]
- 6.Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal radius fractures in older women: A 10-year follow-up study of descriptive characteristics and risk factors: The study of osteoporotic fractures. J Am Geriatrics Society. 2001;50:97–103. doi: 10.1046/j.1532-5415.2002.50014.x. [DOI] [PubMed] [Google Scholar]
- 7.US Census Bureau PD. [Accessed September 16, 2009.];American Community Survey. 2005–2007 http://factfinder.census.gov/servlet/ADPTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2007_3YR_G00_DP3YR5&-ds_name=&-_lang=en&-redoLog=false:1-5.
- 8.Clayton RA, Gaston MS, Ralston SH, Court-Brown CM, McQueen MM. Association between decreased bone mineral density and severity of distal radial fractures. J Bone Joint Surg Am. 2009;91:613–619. doi: 10.2106/JBJS.H.00486. [DOI] [PubMed] [Google Scholar]
- 9.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004;18:680–686. doi: 10.1097/00005131-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]
- 12.Strange-Vognsen HH. Intraarticular fractures of the distal end of the radius in young adults. A 16 (2–26) year follow-up of 42 patients. Acta Orthop Scand. 1991;62:527–530. doi: 10.3109/17453679108994488. [DOI] [PubMed] [Google Scholar]
- 13.Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23:237–242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 14.Synn AJ, Makhni EC, Makhni MC, Rozental TD, Day CS. Distal radius fractures in older patients: is anatomic reduction necessary? Clin Orthop Relat Res. 2009;467:1612–1620. doi: 10.1007/s11999-008-0660-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg. 2000;25A:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 16.Anzarut A, Johnson JA, Rowe BH, Lambert RGW, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated fractures. J Hand Surg. 2004;29A:1121–1127. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Fu YC, Chien SH, Huang PJ. Use of an external fixation combined with the buttress-maintain pinning method in treating comminuted distal radius fractures in osteoporotic patients. J Trauma. 2006;60:330–333. doi: 10.1097/01.ta.0000203538.29179.5b. [DOI] [PubMed] [Google Scholar]
- 18.Atroshi I, Brogren E, Larsson GU, Kloow J, Hofer M, Berggren AM. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445–453. doi: 10.1080/17453670610046389. [DOI] [PubMed] [Google Scholar]
- 19.Herrera M, Chapman CB, Roh M, Strauch RJ, Rosenwasser MP. Treatment of unstable distal radius fractures with cancellous allograft and external fixation. J Hand Surg Am. 1999;24:1269–1278. doi: 10.1053/jhsu.1999.1269. [DOI] [PubMed] [Google Scholar]
- 20.Hutchinson DT, Strenz GO, Cautilli RA. Pins and plaster vs external fixation in the treatment of unstable distal radial fractures. A randomized prospective study. J Hand Surg Br. 1995;20:365–372. doi: 10.1016/s0266-7681(05)80095-6. [DOI] [PubMed] [Google Scholar]
- 21.Kwasny O, Fuchs M, Hertz H, Quaicoe S. Skeletal transfixation in treatment of comminuted fractures of the distal end of the radius in the elderly. J Trauma. 1990;30:1278–1284. doi: 10.1097/00005373-199010000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Ochman S, Frerichmann U, Armsen N, Raschke MJ, Meffert RH. Is use of the fixateur externe no longer indicated for the treatment of unstable radial fracture in the elderly? Unfallchirurg. 2006;109:1050–1057. doi: 10.1007/s00113-006-1166-6. [DOI] [PubMed] [Google Scholar]
- 23.Strohm PC, Muller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures. A randomized trial. J Bone Joint Surg Am. 2004;86-A:2621–2628. doi: 10.2106/00004623-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Chung KC, Squitiere L, Kim HM. A comparative outcomes study of using the volar locking plating system for distal radius fractures in both young and elderly adults. J Hand Surg. 2008;33A:809–819. doi: 10.1016/j.jhsa.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stroup DF, Berlin JA, Morton SC. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 26.Handoll HH, Madhok R. Conservative interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003:CD000314, 1–14. doi: 10.1002/14651858.CD000314. [DOI] [PubMed] [Google Scholar]
- 27.Margaliot Z, Haase SC, Kotsis SV, Kim HM, Chung KC. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg. 2005;30A:1185–1199. doi: 10.1016/j.jhsa.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 28.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 29.van Aaken J, Beaulieu JY, Della Santa D, Kibbel O, Fusetti C. High rate of complications associated with extrafocal kirschner wire pinning for distal radius fractures. Chir Main. 2008;27:160–166. doi: 10.1016/j.main.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 30.Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325. e1326. doi: 10.1016/j.arthro.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 31.Ryu JY, Cooney WP, 3rd, Askew LJ, An KN, Chao EY. Functional ranges of motion of the wrist joint. J Hand Surg [Am] 1991;16:409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]
- 32.Ring D, Jupiter JB. Treatment of osteoporotic distal radius fractures. Osteoporos Int. 2005;16:S80–84. doi: 10.1007/s00198-004-1808-x. [DOI] [PubMed] [Google Scholar]
- 33.Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1568–1577. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]
- 34.Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1837–1846. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 35.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg. 1986;68A:647–659. [PubMed] [Google Scholar]
- 36.Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg. 1994;19A:325–340. doi: 10.1016/0363-5023(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 37.Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005;36:1435–1439. doi: 10.1016/j.injury.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 38.Melone CP., Jr Open treatment for displaced articular fractures of the distal radius. Clin Orthop Relat Res. 1986:103–111. [PubMed] [Google Scholar]
- 39.Margaliot Z, Chung KC. Systematic reviews: a primer for plastic surgery research. Plast Reconstr Surg. 2007;120:1834–1841. doi: 10.1097/01.prs.0000295984.24890.2f. [DOI] [PubMed] [Google Scholar]
- 40.Fanuele J, Koval KJ, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91:1313–1319. doi: 10.2106/JBJS.H.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87:837–40. doi: 10.1302/0301-620X.87B6.15608. [DOI] [PubMed] [Google Scholar]
- 42.Cannegieter DM, Juttman JW. Cancellous grafting and external fixation for unstable Colles fractures. J Bone Joint Surg. 1997;79B:428–432. doi: 10.1302/0301-620x.79b3.6835. [DOI] [PubMed] [Google Scholar]
- 43.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27:1–6. doi: 10.1007/s00264-002-0393-x. Epub 2002 Aug 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gruber G, Gruber K, Giessauf C, Clar H, Zacherl M, Fuerst F, Bernhardt GA. Volar plate fixation of AO type C2 and C3 distal radius fractures, a single-center study of 55 patients. J Orthop Trauma. 2008 Aug;22:467–72. doi: 10.1097/BOT.0b013e318180db09. [DOI] [PubMed] [Google Scholar]
- 45.Fujii K, Henmi T, Kanematsu Y, Mishiro T, Sakai T, Terai T. Fractures of the distal end of the radius in elderly patients. A comparative study of anatomic and functional results. J Orthop Surg. 2002;10:9–15. doi: 10.1177/230949900201000103. [DOI] [PubMed] [Google Scholar]
- 46.Hede JS, Lindblad BE, Mikkelsen SS, Knudsen HM. Comparison of intramedullary fixation and percutaneous pinning of displaced and comminuted Colles’ fractures: a prospective and consecutive study. J Plas and Recon Surg and Hand Surgery. 2000;34:161–166. doi: 10.1080/02844310050160033. [DOI] [PubMed] [Google Scholar]
- 47.Hegeman JH, Oskam J, Vierhout PA, Ten Duis HJ. External fixation for unstable intra-articular distal radial fractures in women older than 55 years. Acceptable functional end results in the majority of the patients despite significant secondary displacement. Injury. 2005;36:339–44. doi: 10.1016/j.injury.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 48.Krukhaug Y, Ugland S, Lie SA, Hove LM. External fixation of fractures of the distal radius: a randomized comparison of the Hoffman compact II non-bridging fixator and the Dynawrist fixator in 75 patients followed for 1 year. Acta Orthop. 2009;80:104–8. doi: 10.1080/17453670902807433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lattmann T, Dietrich M, Meier C, Kilgus M, Platz A. Comparison of 2 surgical approaches for volar locking plate osteosynthesis of the distal radius. J Hand Surg. 2008;33A:1135–1143. doi: 10.1016/j.jhsa.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 50.McQueen MM, Hajducka, Court-Brown CM. Redisplaced unstable fractures of the distal radius. J Bone Joint Surg (Br) 1996;78B:404–9. [PubMed] [Google Scholar]
- 51.McQueen MM. Redisplaced unstable fractures of the distal radius. J Bone Joint Surg (Br) 1998;80B:665–9. doi: 10.1302/0301-620x.80b4.8150. [DOI] [PubMed] [Google Scholar]
- 52.Orbay JL, Fernandez DL. Volar fixed angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29A:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 53.Pritchett JW. External fixation or closed medullary pinning for unstable Colles fractures? J Bone Joint Surg. 1995;77B:267–269. [PubMed] [Google Scholar]
- 54.Sanchez-Sotelo J, Munuera L, Madero R. Treatment of fractures of the distal radius with a remodellable bone cement. J Bone Joint Surg (Br) 2000;82B:856–63. doi: 10.1302/0301-620x.82b6.10317. [DOI] [PubMed] [Google Scholar]
- 55.Schmalholz A. External skeletal fixation versus cement fixation in the treatment of redislocated Colles’ fracture. Clin Ortho Relat Research. 1990;254:236–241. [PubMed] [Google Scholar]
- 56.Shiota E, Matsuzaki A, Arinaga M, Izaki T, Kozaki N. Conehead wedging screw for distal radius fractures in elderly patients. Clin Ortho Relat Research. 2003;407:203–210. doi: 10.1097/00003086-200302000-00029. [DOI] [PubMed] [Google Scholar]
- 57.Ziran BH, Scheel M, Keith MW. Pin reduction and fixation of volar fracture fragment s of distal radius fractures via the flexor carpi radialis tendon. J Trauma. 2000;49:433–439. doi: 10.1097/00005373-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 58.Lanting B, MacDermaid J, Drosdowech D, Faber KJ. Proximal humeral fractures: A systematic review of treatment modalities. J Shoulder Elbow Surg. 2008;18:42–54. doi: 10.1016/j.jse.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 59.Muller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermaid J. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: A systematic review. J Hand Therapy. 2004;17:210–28. doi: 10.1197/j.jht.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 60.Cook DJ, Guyatt GH, Laupacis A, Sackett DL, Goldberg RJ. Clinical recommendations using levels of evidence for antithrombotic agents. Chest. 1995;108:227S–230S. doi: 10.1378/chest.108.4_supplement.227s. [DOI] [PubMed] [Google Scholar]