Abstract
Objectives. We sought state-level factors associated with the adoption of medications to treat mental health conditions on state formularies for the AIDS Drug Assistance Program.
Methods. We interviewed 22 state and national program experts and identified 7 state-level factors: case burden, federal dollar-per-case Ryan White allocation size, political orientation, state wealth, passage of a mental health parity law, number of psychiatrists per population, and size of mental health budget. We then used survival analysis to test whether the factors were associated with faster adoption of psychotropic drugs from 1997 to 2008.
Results. The relative size of a state's federal Ryan White HIV/AIDS Program allocation, the state's political orientation, and its concentration of psychiatrists were significantly associated with time-to-adoption of psychotropic drugs on state AIDS Drug Assistance Program formularies.
Conclusions. Substantial heterogeneity exists across states in formulary adoption of drugs to treat mental illness. Understanding what factors contribute to variation in adoption is vital given the importance of treating mental health conditions as a component of comprehensive HIV care.
As HIV care has changed from an acute to a chronic care model, providers and policymakers have recognized the need to treat mental health conditions among HIV-infected populations. HIV and mental illness are interrelated in several important ways.1 Severe mental illness, particularly bipolar disorder and schizophrenia, may increase risk behavioral factors for HIV, thereby increasing the likelihood of infection.2–5 Depression may worsen HIV disease, leading to conditions such as CD4+ T-lymphocyte count decline, increased incidence of AIDS-defining illness, and increased AIDS-related mortality.6–9 Likewise, symptoms of HIV may overlap with somatic symptoms of depression,10,11 the stigma and social effects of HIV may cause depression,12–14 and depression may hamper adherence to the entire continuum of HIV care, including adherence to antiretroviral therapy.15–19 One half of individuals in a nationally representative sample of HIV-infected individuals in the United States had a psychiatric disorder.20 This prevalence may increase because new HIV infections disproportionately affect youth, women, individuals with lower socioeconomic status, and minorities.1 Treating mental illness is therefore important not only as part of holistic care for HIV-infected individuals but also as part of improving HIV-related health outcomes.
Approximately 30% of HIV-infected individuals in the United States receive antiretroviral medications through state AIDS Drug Assistance Programs (ADAPs), which are financed and maintained through the Ryan White HIV/AIDS Program (National ADAP Monitoring Project 2008). ADAPs, and Ryan White programs more generally, are “payers of last resort” for individuals who have gaps in private insurance coverage, who have not progressed to AIDS and thus do not meet Medicaid and Medicare disability requirements, or who do not meet Medicaid income requirements.21
State Ryan White programs have considerable discretion in their program design; this flexibility allows state programs to respond to local needs and the changing HIV epidemic.21 Some federal requirements exists, such as maintaining a minimum pharmaceutical formulary.21 However, decisions on program enrollment, the breadth of reimbursable services and pharmaceuticals, and financing mechanisms are left to the states. The allocation of responsibility of ADAP management decisions to states has led to considerable interstate variation in program generosity, including the size and scope of drug formularies. Drug formularies vary widely, with some states covering primarily antiretrovirals and drugs to treat and prevent opportunistic infections, and other states maintaining unrestricted, open formularies.22
Given the importance of treating mental health conditions as a component of comprehensive HIV care, it is noteworthy that some state ADAP formularies have been much quicker to add medications to treat these conditions. We examined whether there are factors associated with a state's adoption of psychotropic drugs. To generate hypotheses, we interviewed 22 state ADAP managers and other ADAP experts working at national organizations, in academia, for advocacy groups, and in the federal government. We identified a convenience sample of experts involved with state Ryan White programs in both early and later periods to explore factors related to program design over its history. Our sample also included state-level program staff from different geographic regions and some individuals with special expertise in ADAP funding to treat comorbid mental illness. On the basis of these interviews, we identified 7 state-level factors that we hypothesized could be associated with formulary adoption of psychotropic drugs: case burden, the size of federal dollar-per-case Ryan White allocations, political orientation, state wealth, passage of a mental health parity law, the number of psychiatrists per population, and the size of the mental health budget.
METHODS
We obtained drug formulary data from National ADAP Monitoring Project annual reports.22 We identified an expert panel of 6 clinicians with extensive experience treating HIV-infected populations to review our coding of psychotropic drug data. We identified whether a state's ADAP formulary included drugs to treat mental illness in a given year and whether the formulary included drugs to treat specific conditions, including unipolar depression, bipolar depression, anxiety, and schizophrenia. We coded several drugs for multiple conditions. We coded drugs by condition rather than drug class after consultation with our expert panel and ADAP managers. We excluded several drugs commonly used off-label to treat HIV treatment symptoms, including pain and nausea. For each condition, our outcome measure was whether a state included at least 2 drugs for that condition on its formulary in a specific year. The appendix (available as a supplement to the online version of this article at http://www.ajph.org) contains additional details of our categorization of psychotropic drugs by condition.
State-Level Factors
We hypothesized 7 independent variables to be associated with a state's inclusion of mental health drugs on an ADAP formulary. We summarize the data sources and measures in Table 1.
TABLE 1.
State-Level Factors Possibly Associated With a State's Adoption of Psychotropic Drugs on AIDS Drug Assistance Program Drug Formularies: United States, 1997–2008
| Variable | Hypothesis | Measurement | Data Sources |
| Case burden | States with larger HIV-infected populations will be more likely to adopt psychotropic drugs on their ADAP formularies. | Annual AIDS incidence, log-transformed | Centers for Disease Control and Prevention |
| Federal allocation for RW | States with larger federal dollar-per-case allocations have more slack resources to include psychotropic drugs on their ADAP formularies. | Quintile of federal RW allocation, divided by case count | Health Resources and Services Administration, Centers for Disease Control and Prevention, Government Accountability Office |
| Political orientation | States with a Democratic political orientation will be more likely to fund generous public health programs, including adopting psychotropic drugs on their ADAP formularies. | Sum of political party control for state house, senate, and governor | Council of State Governments |
| State wealth | Wealthier states have more resources available to include psychotropic drugs on their ADAP formularies. | Total taxable resources, log-transformed and adjusted for inflation | Department of the Treasury |
| Passage of mental health parity law | States that have successfully passed mental health parity laws have more political support for public programs to treat mental health, making them more likely to adopt psychotropic drugs on their ADAP formularies. | Implementation of state parity law = 1 | National Alliance for the Mentally Ill |
| No. of psychiatrists per population | States with a higher concentration of psychiatrists would be more likely to adopt psychotropic drugs on their ADAP formularies. | Number of psychiatrists, log-transformed | Area Resource File and US Census |
| Size of mental health budget | States with larger mental health budgets have more political support for programs to treat mental health, making them more likely to adopt psychotropic drugs on their ADAP formularies. | Expenditures for state mental health departments, log-transformed and adjusted for inflation | National Association of State Mental Health Program Directors Research Institute, Inc |
Note. ADAP = AIDS Drug Assistance Program; RW = Ryan White HIV/AIDS Program.
First, we expected that a state's HIV case burden would be associated with quicker adoption on the basis of prior work suggesting that problems perceived to be larger in magnitude often engender broader policy action.23,24 Furthermore, states with a larger case burden are likely to have stronger advocacy groups pressing for a more comprehensive approach to financing HIV care. We used year-specific annual AIDS incidence log-transformed from 1990 to 2006 to measure the size of a state's case burden. We used AIDS incidence rather than HIV incidence because not all state HIV surveillance systems reported reliable HIV estimates throughout the study period. Past research on alternate measures of case burden for use in the Ryan White allocation formulas suggests that AIDS incidence is a reasonable proxy for current case burden.25 We obtained data from the Centers for Disease Control and Prevention.
Second, we expected that states with a larger federal dollars-per-case Ryan White allocation would be more likely to include drugs to treat mental illness on their ADAP formulary. Previous research suggests that states with so-called slack resources are more likely to implement cost-expanding policies.26 For a state's federal Ryan White dollars-per-case allocation, we used allocation data from the Health Resources and Services Administration and the Government Accountability Office, combined with estimates of case burden (used in the allocation formula) from the Health Resources and Services Administration and the Centers for Disease Control and Prevention. We standardized federal allocations by dividing by the states’ case count. We used the state's allocation quintile (which compares states to each other within years) rather than absolute dollars-per-case because the case counting methods have changed throughout the program's legislative history.25 The measure included only Titles I and II (currently renamed Parts A, B, and C) because those funds are used for ADAPs. Throughout the article, we use the more general term “case burden” to reflect the various case counting methods for the case burden variable (log AIDS incidence) and the case standardization in the federal Ryan White allocation variable (cumulative number of patients with AIDS before 1997 and estimated number of living patients with AIDS from 1997 to 2006).
Third, we expected that states with more liberal political orientations would be more likely to adopt a broader ADAP formulary that includes psychotropic drugs. For a state's political orientation, we used data from the Council of State Governments. For each chamber of a state's legislature in each year, a Democratic majority was coded as 1 and a Republican majority was coded as −1. Similarly, a governor's office held by a Democrat, Independent, or Republican in a given year was coded as 1, 0, or −1, respectively. For each year, scores were summed with a range from −3 to 3, reflecting a continuum from a Democrat-dominated state government to a Republican-dominated state government.27
Fourth, we expected that wealthier states would be more likely to include mental health drugs on their formularies. In particular, given evidence that state budget crises have led to waitlists in some state's ADAPs,22 states’ wealth per capita in a given year may affect the generosity of the program. We used year-specific total taxable resources log-transformed and adjusted for inflation from the US Department of the Treasury and other sources.28,29
Fifth, we expected that states that successfully passed state mental health parity laws over this period would be more likely to include mental health drugs on ADAP formularies. We coded whether a state implemented a state parity law in a specific year using information available from the National Alliance for the Mentally Ill Web site, and we validated this with data collected by other groups—including the American Psychiatric Association, the National Mental Health Association, the National Council of State Legislatures—and with data from published articles.30,31 In practice, some challenges exist to studying the effects of state parity laws because these laws are heterogeneous and hard to characterize. State parity literature varies substantially about how to categorize these laws. We used relatively broad criteria for defining whether a state implemented a parity law, although we did not consider laws that applied only to state employees as parity states in this analysis.
Sixth, we expected that states with more psychiatrists per population would be more likely to include drugs to treat mental illness on ADAP formularies as the result of professional organization lobbying and a larger supply of mental health providers. We log-transformed psychiatrists per population, obtained from the Area Resource File (number of psychiatrists per state) and the US Census Bureau (state population), in a state in a specific year.
Finally, we expected that states with larger budgets to fund state mental health departments would be more likely to include mental health drugs on ADAP formularies because of a broader commitment to treat mental illness. We obtained data on the size of a state's mental health budget from the National Association of State Mental Health Program Directors Research Institute.32 We log-transformed expenditures to fund each state's mental health department and adjusted them for inflation.
Empirical Modeling Strategy
We used a multivariate regression framework to test whether the 7 state-level predictors were associated with faster adoption of psychotropic drugs. We evaluated the hypotheses outlined in Table 1 by examining the statistical significance and sign of each coefficient.
We analyzed the time-to-event data from 1997 to 2008 using parametric models for survival time data. We have reported 5 separate sets of models that correspond to the adoption of any drug to treat mental illness (primary outcome) and the adoption of drugs to treat each of the 4 conditions (unipolar depression, bipolar depression, anxiety disorders, and schizophrenia). The model took the following form:
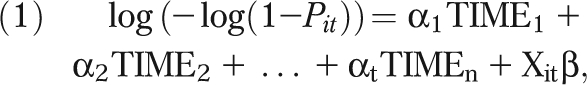 |
where Pit is the probability that a state i includes mental health drugs in period t, given that the state had not already included them, TIMEt represents a set of dummy variables corresponding to the n periods, and Xit is a vector of state characteristics whose values are allowed to vary across the eras. The complementary log-log link function accounted for the interval length and gave the coefficients a relative risk interpretation.33 We estimated the model through maximum likelihood using SAS version 9.2 (SAS Institute, Cary, NC).
For each outcome, we estimated 2 sets of models with periods of different lengths: a model grouped by year, and a model grouped by era. Time-to-adoption survival data are often estimated using semiparametric methods (the Cox proportional hazards model). We were not able to use this standard approach because of left censoring. Our data source contains only formulary data from 1997 to 2008, and some states did not have functional ADAPs until 1996. However, some states had already included mental health drugs on their formulary by 1997. Although it is theoretically possible to generate survival models that adjust for left censoring, conventional statistical software packages do not yet have the capacity to incorporate both left censoring and time-varying covariates.
Year-time and era-time grouped models.
The year-grouped model contained a set of dummy variables (YEARt) for years 1997 through 2008. In this specification, years 1991 through 1997 were aggregated into 1 year (1997). The second modeling strategy grouped predictor and outcome data by 4 major eras of ADAP-related policymaking. Era definitions were derived from informal conversations with program managers and HIV policy experts and a review of Ryan White documents. The first era included years 1991–1997 and corresponded to the early years of the program before and during the introduction of new combination antiretroviral therapy in 1996. During this period, ADAPs were forming and learning how to operate. Limited drug therapies engendered a focus on acute care rather than chronic disease management. The second era included years 1998–2002. All ADAPs had formed by this period. In contrast to the first era, ADAPs experienced budget shortfalls because of the high cost of medications and patients living longer. In 2003, the fusion inhibitor Fuzeon (Genentech, South San Francisco, CA) was introduced. Because this drug was expensive, states had to decide whether to include it on the formulary and how to restrict its use. The National ADAP Monitoring Project described how Fuzeon “underscores the changing nature of the treatment environment in which ADAPs operate, which in turn creates new fiscal pressures.”34 The third era was 2003–2005. The last era included years 2006–2008. These years correspond to the implementation of Medicare Part D drug benefits, which shifted costs away from ADAP.35
As a sensitivity analysis, we estimated a third set of regressions that used a 2-stage approach: a logistic regression that predicted early adoption (by 1997) and a time-to-event model for late adopters (1998–2008). Results were consistent with those presented here and are available from the authors upon request.
Lagged and grouped covariates.
We lagged all covariates by 1 year. Models derived from data grouped across multiple years used the mean value of the covariate in the period.
RESULTS
Table 2 includes descriptive information on each explanatory factor at key time points (1997, 2002, 2005, and 2007). Major changes over time include a decrease in the median case burden (from 13.45 AIDS patients per population in 1997 to 6.9 AIDS patients per capita in 2008), a shift from a Republican to Democratic mean state political orientation (from a −0.32 state power score in 1997 to 0.38 in 2008), and a large increase in the percentage of states adopting a mental health parity law over time (from 10% of states in 1997 to 94% of states in 2008).
TABLE 2.
Summary Data on State-Level Factors Possibly Associated With the Adoption of Psychotropic Drugs: United States, 1997–2008
| Variable | 1997 | 2002 | 2005 | 2008 |
| Case burden, median | 13.45 | 8.05 | 7.80 | 6.90 |
| Federal RW allocation quintile, meana | 1.96 | 1.96 | 1.96 | 1.96 |
| Liberal political orientation, mean | −0.32 | −0.18 | −0.28 | 0.38 |
| State wealth, $ per population, median | 36 867 | 41 122 | 43 479 | 47 452 |
| Mental health parity law, % adoption | 10 | 74 | 82 | 94 |
| No. of psychiatrists per population, median | 10.5 | 10.2 | 10.2 | 10.4 |
| Size of mental health budget, $ thousand, median | 2644 | 2926 | 2980 | 3677 |
Note. RW = Ryan White HIV/AIDS Program.
Allocation quintile values are from 0 to 4.
Table 3 displays the fraction of states (N = 50) that had adopted drugs to treat any mental health condition and drugs to treat specific conditions (unipolar depression, bipolar depression, anxiety disorders, and schizophrenia) by the end of each era (1997, 2002, 2005, and 2008). By 1997, 10% of states included drugs to treat at least 1 condition. At that time, the most commonly included condition was unipolar depression (8% of states). Less than 5% of states had drugs to treat bipolar depression, anxiety, or schizophrenia. By 2008, 82% of states included drugs to treat at least 1 mental health condition. Unipolar depression remained the most commonly included condition (72%), although at least half of states included drugs to treat bipolar depression (58%), anxiety (50%), and schizophrenia (66%).
TABLE 3.
Percentage of States’ Formularies (N = 50) That Adopted Psychotropic Drugs to Treat Mental Health Conditions on AIDS Drug Assistance Programs: United States, 1997–2008
| Drug Treatment Variable | 1997, % Adoption | 2002, % Adoption | 2005, % Adoption | 2008, % Adoption |
| Any mental health condition | 10 | 48 | 56 | 82 |
| Depression | 8 | 48 | 56 | 72 |
| Bipolar depression | 2 | 34 | 38 | 58 |
| Anxiety disorders | 4 | 28 | 30 | 50 |
| Schizophrenia | 2 | 34 | 36 | 66 |
Note. Adoption is a measure of whether a state included at least 2 drugs for that condition in a specific year.
Table 4 shows the regression results examining the adoption of drugs to treat any mental health condition. The 2 models correspond to the year-time (column 1) and era-time (column 2) specifications. Regression coefficients can be interpreted as log-relative risk.
TABLE 4.
Parameter Estimates for Survival Models of Time-to-Adoption of Mental Health Drugs to Treat at Least 1 Mental Health Condition on AIDS Drug Assistance Program Formularies: United States, 1997–2008
| Era Specification |
Year Specification |
|||
| Variable | b (SE) | P | b (SE) | P |
| AIDS incidence | −0.40 (0.30) | .189 | −0.33 (0.30) | .277 |
| Allocation quintile | 0.42 (0.18) | .022* | 0.42 (0.16) | .007** |
| Power score | 0.25 (0.11) | .018* | 0.21 (0.09) | .025* |
| Total taxable resources | 1.13 (1.50) | .453 | 1.01 (1.39) | .47 |
| Mental health parity law | −0.43 (0.54) | .433 | −0.21 (0.43) | .624 |
| No. of psychiatrists per capita | 1.20 (0.61) | .05 | 1.07 (0.52) | .04* |
| State mental health agency budget | −0.12 (0.23) | .588 | −0.13 (0.23) | .555 |
| Era dummies | Yes | No | ||
| Year dummies | No | Yes | ||
Note. Reference for era dummies is era 1; reference for year dummies is 1997.
*P value significant at .05; **P value significant at .01.
The relative size of a state's federal Ryan White allocation, its political orientation, and its concentration of psychiatrists were all significant predictors of time-to-adoption. States with larger Ryan White allocations, more Democratic political orientations, and a larger number of psychiatrists per capita were earlier to adopt mental health drugs. Case burden, total taxable resources, the presence of a mental health parity law, and the state mental health agency budget were not associated with time-to-adoption of drugs to treat mental health conditions. Results were consistent for the models that used the year- and era-time specifications.
Looking at the year specification, a 1-unit increase in the allocation quintile was associated with a 52.4% higher probability of adopting drugs to treat any mental health condition in the next year, holding all other factors constant (relative risk = exp[0.42] = 1.524; % increase = [1.524 – 1.0] × 100 = 52.4%). Compared with states in the lowest federal allocation quintile, states in the highest federal allocation quintile were more than 4 times as likely to adopt a drug in the next year (relative risk = exp[4 × 0.42] = 5.394; % increase = [5.394 – 1.0] × 100 = 4.394). A shift in state political representation involving a state's house of representatives, senate, or governor's office changing from Republican to Democratic control was associated with a 52.3% higher probability of adopting psychotropic drugs in the next year. (A party switch was associated with a 2-unit increase in the state power score because each Republican majority is coded as −1, and each Democratic majority is coded as +1; relative risk = exp[2 × 0.21] = 1.523; % increase = [1.523 – 1.0] × 100.) A 1% increase in the number of psychiatrists per population was associated with a 1.073% difference in the hazards of adopting a drug.
Table 5 shows the regression results for the models that examine adoption of drugs to treat specific conditions (unipolar depression, bipolar depression, anxiety, and schizophrenia). These models all use a year-time specification; the era-time specification results were qualitatively similar and are not included here but are available from the authors upon request.
TABLE 5.
Parameter Estimates for Survival Models of Time-to-Adoption of Mental Health Drugs to Treat Specific Conditions on AIDS Drug Assistance Program Drug Formularies: United States, 1997–2008
| Depression |
Bipolar Disorder |
Anxiety |
Schizophrenia |
|||||
| Variable | b (SE) | P | b (SE) | P | b (SE) | P | b (SE) | P |
| AIDS incidence | −0.34 (0.33) | .298 | −0.43 (0.33) | .192 | −0.67 (0.36) | .063 | −0.23 (0.32) | .48 |
| Allocation quintile | 0.43 (0.16) | .009** | 0.39 (0.18) | .029* | 0.26 (0.18) | .148 | 0.30 (0.16) | .058* |
| Power score | 0.21 (0.10) | .032* | 0.04 (0.11) | .71 | 0.16 (0.12) | .17 | 0.12 (0.11) | .265 |
| Total taxable resources | 0.10 (1.53) | .95 | 2.39 (1.59) | .134 | 4.04 (1.83) | .027* | 2.16 (1.42) | .127 |
| Mental health parity law | −0.35 (0.44) | .426 | 0.38 (0.54) | .478 | −0.24 (0.56) | .662 | 0.23 (0.53) | .672 |
| No. of psychiatrists per capita | 1.24 (0.55) | .024* | −0.09 (0.56) | .877 | 0.83 (0.62) | .174 | 0.56 (0.56) | .315 |
| State mental health agency budget | −0.05 (0.24) | .821 | 0.25 (0.26) | .336 | 0.49 (0.27) | .071 | 0.08 (0.24) | .745 |
| Era dummies | No | No | No | No | ||||
| Year dummies | Yes | Yes | Yes | Yes | ||||
Note. Conditions treated were unipolar depression, bipolar depression, anxiety, and schizophrenia. Reference for year dummies was 1997. All models used the year-time specification. Results were consistent with models that used the era-time specification.
*P value significant at .05; **P value significant at .01.
States with a larger federal allocation had a shorter time-to-adoption of drugs to treat unipolar depression, bipolar depression, and schizophrenia. States with a more Democratic political orientation had a shorter time-to-adoption of antidepressants. States with greater total taxable resources were more likely to be early adopters of drugs to treat anxiety. States with more psychiatrists per capita were more likely to be early adopters of antidepressants. As with the previous results, case burden, the presence of a mental health parity law, and the size of a state's mental health agency budget were not significant predictors of drug adoption.
In addition to these models presented in Tables 4 and 5, we performed sensitivity analyses using a 1- or 3-drug threshold. These analyses yielded consistent results and are available from the authors upon request.
DISCUSSION
We found that the relative size of a state's federal Ryan White allocation, a state's political orientation, and its concentration of psychiatrists were all significantly associated with time-to-adoption of psychotropic drugs on state ADAP formularies. In addition, states with greater total taxable resources were more likely to be early adopters of drugs to treat anxiety.
This study has several strengths. First, although there is a broad literature on the importance of treating comorbid mental health conditions, there has been less analysis of the political factors that make an HIV-infected person more or less likely to have access to psychotropic drugs across states. This study contributes to the literature on how federal and state health policies facilitate access to care. Past literature has demonstrated significant interstate variation in federal Ryan White allocations.25,36,37 Our analysis built on this finding by testing empirically whether these differential allocations (on a dollar-per-case standard) corresponded with interstate variation in the coverage of mental health drugs. Second, our time-to-event analysis allowed us to explicitly model program changes over time as underlying conditions (such as political ideology) change within a state.
An additional strength is that we used multiple outcome measures (any mental health drug indication and specific drug indications). This approach allowed us to identify which types of drugs were most likely to be adopted and whether the state-level factors that predicted the adoption of psychotropic drugs changed by condition. Some states, such as Missouri, Montana, and New York, included a wide range of drugs to treat mental health conditions during their initial formulary expansions. However, ADAPs with more limited formularies had to make deliberate choices of which mental health drugs to include first. Examining the time-to-adoption of drugs to treat specific conditions (rather than mental health drugs more generally) showed that drugs to treat depression were likely to be adopted earlier (Table 3). The significant coefficients for federal Ryan White allocations (depression, bipolar, and schizophrenia outcomes) and state wealth (anxiety outcome) suggest that resource constraints were a major factor in decisions to expand formularies to include drugs to treat specific mental health conditions. Future research may clarify how ADAP decision makers consider clinical, epidemiologic, and economic evidence in their decisions to include drugs to treat specific mental health conditions.
This study had a few potential limitations, which suggest avenues of future research. Although we were not able to consider the relative price of drugs in this study, it is likely that the cost of a drug is another important factor in determining a state's formulary adoption. If so, the continued movement of many psychotropic drugs off patent in the coming years should create greater access to affordable mental health treatments among this population. Also, we did not consider the inclusion of drugs to treat substance use disorders in this study. As with mental health, the comorbidity of substance use disorders is high in the HIV population.38 Our research suggests that by 2008, only 22% of formularies included drugs to treat substance use disorders. (We calculated the inclusion of substance abuse medications using the same methodology as for the other conditions. We did not include drugs to treat nicotine dependence.) Drug therapy plays an increasingly important role in the treatment of substance use disorders with the availability of bupenorphine, naltrexone, and others.
Although past research documents how access to HIV services among poor and minority populations differs from access in the general population,39,40 our state-level data did not allow us to test whether there are individual differences in access to psychotropic drugs among these groups. However, the issue of access to psychotropic drugs among vulnerable populations living with HIV warrants further study.
Our quantitative analysis did not consider why drugs were included, how formulary decisions were made, or variation in decision-making processes across states. Because many ADAP managers did not remain in their positions throughout the study period, it was difficult to measure intent. In particular, it was challenging to determine whether the state added certain drugs with off-label indications to treat mental health or HIV disease. Several commonly included drugs have multiple indications (such as lamotrigine for bipolar depression and schizophrenia). Without additional information, it was impossible to determine whether the drug was included to treat 1 or all possible conditions. To address this data limitation, we minimized the probability of false-positive classifications by excluding drugs commonly used to treat non–mental health conditions and requiring that states include at least 2 drugs for the conditions. Although this decision rule could have led to some miscoding, our robust findings in sensitivity analyses suggest that this was not a major problem.
In the era-time grouped model, the aggregation of covariate data lost some precision. However, because the values of these covariates were highly correlated across time and because the year and era models yielded similar results, we do not think this loss of precision led to significant bias.
Finally, HIV care is financed publicly through a complex network of care, which includes Medicare, Medicaid, and the Veterans Administration. Additionally, states may provide mental health services to ADAP patients through state mental health agencies. Consequently, a state may have a limited ADAP formulary because mental health drugs are available through other public programs. Subsequent research could explore how HIV-infected individuals access care through local fragmented systems of care, the extent to which local case management systems allow HIV-infected individuals to manage comorbid mental illness, and the effects of these various local systems of care on HIV and mental health outcomes.
Acknowledgments
The National Institute on Drug Abuse (grant R01DA015612) and the Agency of Healthcare Research and Quality (grant T32HS017589) supported this work.
We are grateful to the ADAP and mental health experts who agreed to participate in the interviews and expert panel, as well as A. David Paltiel, Patricia Keenan, Mark Schlesinger, and Haiqun Lin for a review of an earlier draft.
Human Participant Protection
No protocol was necessary for the statistical analysis because data were obtained from secondary sources. The expert interviews were exempt from review because experts included public officials, participants remained anonymous, and the interview guide did not solicit sensitive or confidential information.
References
- 1.Committee on Public Financing and Delivery of HIV Care, Board on Health Promotion and Disease Prevention Public Financing and Delivery of HIV/AIDS Care: Securing the Legacy of Ryan White. Washington, DC: National Academies Press; 2005 [Google Scholar]
- 2.Grassi L. Risk of HIV infection in psychiatrically ill patients. AIDS Care. 1996;8(1):103–116 [DOI] [PubMed] [Google Scholar]
- 3.Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illness. Clin Psychol Rev. 1997;17(3):271–291 [DOI] [PubMed] [Google Scholar]
- 4.Sullivan G, Koegel P, Kanouse DE, et al. HIV and people with serious mental illness: the public sector's role in reducing HIV risk and improving care. Psychiatr Serv. 1999;50(5):648–652 [DOI] [PubMed] [Google Scholar]
- 5.Weiser SD, Wolfe WR, Bangsberg DR. The HIV epidemic among individuals with mental illness in the United States. Curr HIV/AIDS Rep. 2004;1(4):186–192 [DOI] [PubMed] [Google Scholar]
- 6.Ironson G, O'Cleirigh C, Fletcher MA, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67(6):1013–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285(11):1466–1474 [DOI] [PubMed] [Google Scholar]
- 8.Anastos K, Schneider MF, Gange SJ, et al. The association of race, sociodemographic, and behavioral characteristics with response to highly active antiretroviral therapy in women. J Acquir Immune Defic Syndr. 2005;39(5):537–544 [PubMed] [Google Scholar]
- 9.Cook JA, Grey D, Burke J, et al. Depressive symptoms and AIDS-related mortality among a multisite cohort of HIV-positive women. Am J Public Health. 2004;94(7):1133–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalichman SC, Sikkema KJ, Somlai A. Assessing persons with human immunodeficiency virus (HIV) infection using the Beck Depression Inventory: disease processes and other potential confounds. J Pers Assess. 1995;64(1):86–100 [DOI] [PubMed] [Google Scholar]
- 11.Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV/AIDS. J Nerv Ment Dis. 2000;188(10):662–670 [DOI] [PubMed] [Google Scholar]
- 12.Mak WW, Poon CY, Pun LY, Cheung SF. Meta-analysis of stigma and mental health. Soc Sci Med. 2007;65(2):245–261 [DOI] [PubMed] [Google Scholar]
- 13.Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–1831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith R, Rossetto K, Peterson BLA. Meta-analysis of disclosure of one's HIV-positive status, stigma, and social support. AIDS Care. 2008;20(10):1266–1275 [DOI] [PubMed] [Google Scholar]
- 15.Fairfield KM, Libman H, Davis RB, Eisenberg DM. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999;14(7):395–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care STDS. 2008;22(3):233–243 [DOI] [PubMed] [Google Scholar]
- 17.Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17(4):169–177 [DOI] [PubMed] [Google Scholar]
- 18.Horberg MA, Silverberg MJ, Hurley LB, et al. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47(3):384–390 [DOI] [PubMed] [Google Scholar]
- 19.Kacanek D, Jacobson DL, Spiegelman D, Wanke C, Isaac R, Wilson IB. Incident depression symptoms are associated with poorer HAART adherence: a longitudinal analysis from the Nutrition for Healthy Living study. J Acquir Immune Defic Syndr. 2010;53(2):266–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bing EG, Burnam MA, Longshore D, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–728 [DOI] [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services The Ryan White Program. Available at: http://hab.hrsa.gov/about. Accessed February 2011
- 22.National ADAP Monitoring Project. Available at: http://www.kff.org/hivaids/upload/7029-041.pdf. Accessed November 19, 2008
- 23.Kingdon JW. Agendas, Alternatives, and Public Policies. 2nd ed New York: Longman; 2003 [Google Scholar]
- 24.Rochefort DA, Cobb RW, The Politics of Problem Definition. Lawrence, KS: University Press of Kansas; 1994 [Google Scholar]
- 25.Committee on the Ryan White CARE Act, Institute of Medicine of the National Academies Measuring What Matters: Allocation, Planning, and Quality Assessment for the Ryan White CARE Act. Washington, DC: National Academies Press; 2004 [PubMed] [Google Scholar]
- 26.Daley DM, Garand JC. Horizontal diffusion, vertical diffusion, and internal pressure in state environmental policymaking, 1989–1998. American Politics Research. 2005;33(5):615–644 [Google Scholar]
- 27.Barry CL, Busch SH. Do state parity laws reduce the financial burden on families of children with mental health care needs? Health Serv Res. 2007;42(3 pt 1):1061–1084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Compson ML. Historical estimates of total taxable resources for U.S. states, 1981–2000. Publius: The Journal of Federalism. 2003;33(2):55–73 [Google Scholar]
- 29.Mikesell J. Changing state fiscal capacity and tax effort in an era of devolving government, 1981–2003. Publius: The Journal of Federalism. 2007;37(4):532–550 [Google Scholar]
- 30.Gitterman DP, Sturm R, Pacula RL, Scheffler RM. Does the sunset of mental health parity really matter? Adm Policy Ment Health. 2001;28(5):353–369 [DOI] [PubMed] [Google Scholar]
- 31.Peck MC, Scheffler RM. An analysis of definitions of mental illness used in state parity laws. Psychiatr Serv. 2002;53(9):1089–1095 [DOI] [PubMed] [Google Scholar]
- 32.National Association of State Mental Health Program Directors Research Institute. State Mental Health Agency Profiles Systems (Profiles) and Revenues Expenditures Study. Available at: http://www.nri-inc.org/projects/Profiles/RevenuesExpenditures.cfm. Accessed February 2011
- 33.Allison PD. Survival Analysis Using SAS: A Practical Guide. Cary, NC: SAS Institute, Inc; 2003 [Google Scholar]
- 34.David MD, Aldridge C, Kates J, Chou L. National ADAP Monitoring Project Annual Report; 2003. Available at: http://www.kff.org/hivaids/20030430a-index.cfm. Accessed February 2011
- 35.Henry J. Kaiser Family Foundation. U.S. Federal Funding for HIV/AIDS: The FY 2009 Budget Request. Available at: http://www.kff.org/hivaids/7861.cfm. Accessed February 2011
- 36.Martin EG, Pollack HA, Paltiel AD. Fact, fiction, and fairness: resource allocation under the Ryan White CARE Act. Health Aff (Millwood). 2006;25(4):1103–1112 [DOI] [PubMed] [Google Scholar]
- 37.Martin EG, Keenan PS. Sticky dollars: inertia in the evolution of federal allocations for HIV care through the Ryan White HIV/AIDS Program. Publius: The Journal of Federalism. 2011; 41(4):101–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burnam MA, Bing EG, Morton SC, et al. Use of mental health and substance abuse treatment services among adults with HIV in the United States. Arch Gen Psychiatry. 2001;58(8):729–736 [DOI] [PubMed] [Google Scholar]
- 39.Korthuis PT, Saha S, Fleishman JA, et al. Impact of patient race on patient experiences of access and communication in HIV care. J Gen Intern Med. 2008;23(12):2046–2052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cunningham WE, Markson LE, Andersen RM, et al. Prevalence and predictors of highly active antiretroviral therapy use in patients with HIV infection in the United States. HCSUS Consortium. HIV cost and services utilization. J Acquir Immune Defic Syndr. 2000;25(2):115–123 [DOI] [PubMed] [Google Scholar]


