Abstract
Background
Improvements in prosthetic materials, designs, and implant fixation for THA have led to bearing surface wear being the limitation of this technology. Hard-on-hard bearings promise decreased wear rates and increased survival. However, there may be different survival rates based on bearing materials, manufacturing technologies, and femoral component designs. Additionally, survival rate variability may be based on study design.
Questions/purposes
We determined survival rates and study levels of evidence and quality for the following bearings: stemmed metal-on-metal THA, metal-on-metal hip resurfacing, ceramic-on-ceramic THA, and ceramic-on-metal THA.
Methods
We performed a systematic review of the peer-reviewed literature addressing THA hard-on-hard bearings. Quality for Level I and II studies was assessed.
Results
The four Level I or II second-generation stemmed metal-on-metal THA studies reported between 96% and 100% mean survival at 38 to 60 months. The two Level I hip resurfacing studies reported 94% and 98% mean survival at 56 and 33 months. The four Level I studies of ceramic-on-ceramic THA reported survival from 100% at mean 51 months to 96% at 8 years.
Conclusions
While hard-on-hard bearing survival rates have generally been variable with earlier designs, contemporary implants have demonstrated survival of 95% or greater at followup of between 3 and 10 years. Some variability in survival may be due to differences in surgical technique, component positioning, and implant designs. As bearing designs continue to improve with modified materials and manufacturing techniques, use will increase, especially in young and active patients, though concerns remain about the increased reports of adverse events after metal-on-metal bearings.
Introduction
Because of the projected substantial future increase in the need for THA and the increasing demands placed on prostheses by a younger and generally more active patient population than previously treated by surgery, there has been renewed interest in developing new technologies. These will hopefully provide better function, decrease implant wear, and prolong prosthesis survival despite higher activity demands.
Whereas historically THA implant failure was frequently the result of aseptic loosening associated with failure of fixation and implant fracture, improvements in prosthetic materials, designs, and implant fixation resulted in wear of the bearing surface being the primary mechanical limitation of this technology in otherwise correctly implanted metal-on-polyethylene components [47, 84]. Changes in bearing technology have typically focused on increasing implant survival by decreasing articulation wear and resulting osteolysis and reducing dislocation rates. Alternative bearing surfaces are of two types: low-wear metal-on-polyethylene articulations and bearing surfaces using couples other than metal-on-polyethylene. The first encompasses modifications to metal-on-polyethylene articulations to increase their wear resistance. While it has been known for some time gamma irradiation of polyethylene increases wear resistance through crosslinking of the molecular structure [29, 40, 81], historically the clinical application of this altered material was limited because of the concurrent increase in material brittleness with irradiation [8]. More recently, improved strategies for reduction of free radicals during processing, such as serial annealing or doping with antioxidants, allowed for the clinical introduction of second-generation crosslinked polyethylene liners [61, 67, 74]. In vitro studies suggest a 75% to 97% reduction in wear rates compared to conventional polyethylene [21, 62]. Manley and Sutton [56] recently reported metal-on-crosslinked polyethylene bearings are being used in an estimated 70% of primary and revision THAs. This is despite remaining concerns about the material properties of crosslinked polyethylene, such as fatigue strength, fracture toughness, and elongation [66]. The second approach to the development of more wear-resistant bearings has involved the use of hard-on-hard bearing couples. These bearings have the potential to provide advantages in terms of improved implant tribology (lubrication, friction, wear), increased longevity, and reduced dislocation rates. However, there have been concerns about potential disadvantages of these bearings, including potential novel failure modes not typically associated with traditional metal-on-polyethylene articulations and with variable reported survival rates.
In this systematic review, we summarize the published survival rates and study levels of evidence for each of the following hard-on-hard bearing couples: (1) stemmed metal-on-metal THA, (2) metal-on-metal hip resurfacing arthroplasty, (3) ceramic-on-ceramic THA, and (4) ceramic-on-metal THA.
Search Criteria and Strategies
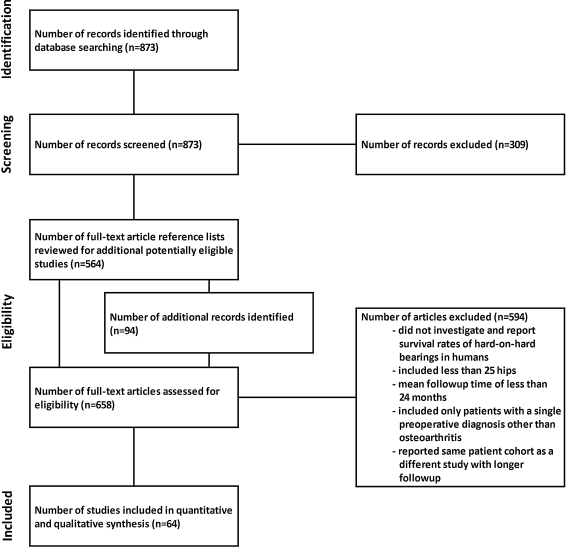
The PubMed database was queried for potentially relevant articles addressing metal-on-metal, ceramic-on-ceramic, and ceramic-on-metal THA or resurfacing hip arthroplasty using the following initial search string: “(((hip[title] and (arthroplasty[title] or replacement[title] or resurfacing[title])) and (metal[title] or ceramic[title] or alumina[title])) OR ((hip[title]) and (resurfacing[title])) OR ((resurfacing[title]) and (arthroplasty[title]) not (patella[title]))).” We identified and screened 873 records. Any records meeting the following criteria were excluded: (1) articles not in English; (2) review articles or letters to the editor; (3) reports of the treatment of any joint other than the hip; (4) studies of hard-on-polyethylene articulations (for example, ceramic heads articulating with polyethylene liners); (5) studies of revision of stemmed hip arthroplasties; (6) animal studies; and (7) first-generation total hip resurfacing implants (designs predating contemporary metal-on-metal articulations). We excluded 309 reports based on these criteria (Fig. 1).
Fig. 1.
A flow diagram shows manuscript identification, screening, eligibility, and inclusion
The reference lists of the remaining 564 reports were then searched for any additional studies meeting our search and exclusion criteria but not identified at the time of our initial search. An additional 94 records were identified through this process.
To answer our questions, the accumulated manuscripts were screened to identify those meeting the following criteria: (1) reported the survival rates of stemmed or resurfacing metal-on-metal hip arthroplasty, ceramic-on-ceramic THA, or ceramic-on-metal THA in humans; (2) included a minimum of 25 hips; and (3) reported a minimum mean followup of 24 months. Any studies limiting the inclusion of patients based on preoperative diagnosis (with the exception of osteoarthritis) were excluded, and only the report with the longest followup was included in cases of multiple reports of the same patient cohort at different time intervals. The manuscripts meeting these criteria were grouped by the type of bearing interface addressed, and the following data were extracted to a spreadsheet for each: the number of hips and patients studied, followup times, the type of implant and bearing, method of fixation, and survival rates. The study design was assessed using the manuscript guidelines found in the Instructions for Authors of Clinical Orthopaedics and Related Research, based on the levels of evidence established by the Centre for Evidence-based Medicine [11].
A total of 64 reports were identified meeting the above criteria: 21 addressed stemmed metal-on-metal THA [9, 13, 16, 19, 20, 23, 30, 35, 39, 51–53, 60, 63, 69, 75, 83, 86, 95, 96, 100], 22 addressed metal-on-metal hip resurfacing arthroplasty [1, 5, 14, 15, 24, 34, 41, 42, 49, 54, 57, 59, 64, 65, 70, 73, 78, 88, 92–94, 101], and 21 reported on ceramic-on-ceramic THA [4, 7, 10, 28, 31–33, 37, 38, 48, 50, 55, 68, 71, 72, 77, 80, 85, 90, 98, 99]. The number of studies with each level of evidence from I to IV is summarized (Table 1). No reports meeting the above criteria were identified that addressed ceramic-on-metal THA.
Table 1.
Number of studies for each bearing couple stratified by level of evidence
| Type of bearing | Level of evidence | |||
|---|---|---|---|---|
| I | II | III | IV | |
| Stemmed metal-on-metal | 3 | 1 | 1 | 16 |
| Metal-on-metal resurfacing | 2 | 1 | 4 | 15 |
| Ceramic-on-ceramic | 4 | 1 | 1 | 15 |
| Ceramic-on-metal | 0 | 0 | 0 | 0 |
The quality of studies with a level of evidence of I and II was assessed for internal validity by three of the authors (MGZ, AJJ, SAS), with any discrepancies resolved by discussion and consensus. First, studies were reviewed to confirm a randomized, controlled design. Two studies did not meet this criterion and were excluded from further analysis. The following parameters were graded as done, not done, or unclear for the remaining 10 studies based on the Cochrane guidelines [82]: randomization, allocation concealment, and blinding (of participants, assessors, and analysts). Additionally, the following study factors were rated as adequate, inadequate, or unclear: baseline comparability of groups based on demographic factors (statistically similar age, body mass index, gender, and preoperative diagnosis to qualify as adequate) and followup (no more than 10% of individuals from any one study arm lost to followup to qualify as adequate). All of the studies had deficiencies in at least one of the above quality dimensions, with a failure to properly blind participants, assessors, and analysts or to explicitly report the blinded parties occurring most commonly (Table 2).
Table 2.
Summarized results of study quality analysis
| Study | Level of evidence | Randomization | Allocation concealment | Blinding | Baseline comparability | Followup | ||
|---|---|---|---|---|---|---|---|---|
| Participants | Assessors | Analysts | ||||||
| Second-generation stemmed metal-on-metal THA | ||||||||
| Zijlstra et al. [100] (2009) | I | Done | Done | Unclear | Not done | Unclear | Adequate | Adequate |
| Jacobs et al. [39] (2004) | I | Unclear | Unclear | Unclear | Unclear | Unclear | Adequate | Inadequate |
| MacDonald et al. [53] (2003) | I | Done | Done | Unclear | Unclear | Unclear | Unclear | Adequate |
| Lombardi et al. [51] (2001) | II | Done | Unclear | Unclear | Unclear | Unclear | Adequate | Adequate |
| Metal-on-metal resurfacing | ||||||||
| Vendittoli et al. [94] (2010) | I | Done | Done | Not Done | Not done | Unclear | Yes | Unclear* |
| Ceramic-on-ceramic (second-generation alumina) | ||||||||
| Lewis et al. [48] (2010) | I | Done | Done | Done | Unclear | Unclear | Unclear | Adequate |
| Bascarevic et al. [4] (2009) | I | Done | Unclear | Unclear | Unclear | Unclear | Adequate | Unclear* |
| Capello et al. [10] (2008) | I | Unclear | Unclear | Unclear | Unclear | Unclear | Adequate | Unclear* |
| Ceramic-on-ceramic (alumina composite) | ||||||||
| Hamilton et al. [32] (2010) | I | Done | Done | Unclear | Unclear | Unclear | Adequate | Adequate |
| Lombardi et al. [50] (2010)† | II | Done | Done | Unclear | Unclear | Unclear | Unclear | Adequate |
* It appears none of the patients were lost to followup, but this is not explicitly stated in the report; †study of composite femoral head on pure alumina liner
Results
The 21 studies addressing stemmed metal-on-metal THA reported survival rates of 71% to 100% at mean followups ranging from 36 to 336 months (Table 3). Four studies encompassed first-generation metal-on-metal bearings [9, 13, 35, 60] that predated the introduction of high-tolerance bearings and improved metal alloys. These studies reported survival rates ranging from as high as 96% at a mean followup of 36 months (range, 24–48 months) to as low as 71% at a mean followup of 135 months (range, 24–140 months). All four studies were Level IV. Seventeen studies encompassed second-generation metal-on-metal bearings [16, 19, 20, 23, 30, 39, 51–53, 63, 69, 75, 83, 86, 95, 96, 100]. These studies reported survival ranging from 93% at 120 months to 100% at a mean followup of 60 months (range, 44–88 months). The longest reported mean followup was 126 months (range, 120–143 months), with a survival rate of 94%. The four Level I or II studies reported survival rates of between 96% and 100% at mean followups ranging from 38 to 60 months [39, 51, 53, 100].
Table 3.
Reported survival rates of first- and second-generation stemmed metal-on-metal THA
| Study | Number of hips (patients) | Type of bearing design | Followup (months)* | Femoral fixation | Acetabular fixation | Survival (%) | Level of evidence |
|---|---|---|---|---|---|---|---|
| First generation | |||||||
| Brown et al. [9] (2002) | 123 (101) | Modified low-tolerance CoCrMo | 336 | Cemented | Cemented | 74† | IV |
| Higuchi et al. [35] (1997) | 38 (38) | Modified low-tolerance CoCrMo | 135 (24–240) | Cemented | Cemented | 71 | IV |
| Dandy and Theodorou [13] (1975) | 739 (NR) | Modified low-tolerance CoCrMo | 60 (24–96) | Cemented | Cemented | 93 | IV |
| McKee and Watson-Farrar [60] (1966) | 50 (50) | Low-tolerance CoCrMo | 36 (24–48) | Cemented | Cemented | 96 | IV |
| Second generation | |||||||
| Neumann et al. [69] (2010) | 100 (99) | High-tolerance CoCrMo | 126 (120–143) | Uncemented | Uncemented | 94 | IV |
| Paleochorlidis et al. [75] (2009) | 99 (84) | High-tolerance CoCrMo | 114 (72–180) | Uncemented | Uncemented | 95 | IV |
| Zijlstra et al. [100] (2009) | 102 (NR) | High-tolerance CoCrMo | 60 | Cemented | Cemented | 97† | I |
| Dastane et al. [16] (2008) | 82 (80) | High-tolerance CoCrMo | 66 (26–140) | Uncemented | Uncemented | 99 | III |
| Delaunay et al. [19] (2008) | 83 (73) | High-tolerance CoCrMo | 120 | Uncemented | Uncemented | 96† | IV |
| Eswaramoorthy et al. [23] (2008) | 85 (82) | High-tolerance CoCrMo | 120 | Uncemented | Cemented | 96† | IV |
| Grubl et al. [30] (2007) | 105 (98) | High-tolerance CoCrMo | 120 | Uncemented | Uncemented | 99† | IV |
| Sharma et al. [86] (2007) | 209 | High-tolerance CoCrMo | 72 (60–132) | Cemented | Cemented | 95 | IV |
| Milosev et al. [63] (2006) | 640 (591) | High-tolerance CoCrMo | 120 | Uncemented | Uncemented | 93† | IV |
| Saito et al. [83] (2006) | 106 (90) | High-tolerance CoCrMo | 72 (60–96) | Uncemented | Cemented | 99 | IV |
| Jacobs et al. [39] (2004) | 95 (95) | High-tolerance CoCrMo | 40 (36–68) | Uncemented | Uncemented | 99 | I |
| Long et al. [52] (2004) | 161 (154) | High-tolerance CoCrMo | 76 (24–108) | Uncemented | Uncemented | 96 | IV |
| MacDonald et al. [53] (2003) | 22 (22) | High-tolerance CoCrMo | 38 (26–47) | Uncemented | Uncemented | 100 | I |
| Lombardi et al. [51] (2001) | 78 (78) | High-tolerance CoCrMo | 39 (23–62) | Uncemented | Uncemented | 100 | II |
| Dorr et al. [20] (2000) | 70 (70) | High-tolerance CoCrMo | 60 (48–84) | Uncemented | Uncemented | 98 | IV |
| Wagner and Wagner [95] (2000) | 76 (76) | High-tolerance CoCrMo | 60 (44–88) | Uncemented | Uncemented | 100 | IV |
| Weber [96] (1996) | 100 (98) | High-tolerance CoCrMo | 48 (24–84) | Uncemented | Uncemented | 95 | IV |
* Values are expressed as mean, with range in parentheses; †survivorship at noted followup time; NR = not reported; CoCrMo = cobalt-chromium-molybdenum.
The 22 studies addressing metal-on-metal hip resurfacing arthroplasty reported survival rates of 84% to 100% at mean followups ranging from 39 to 89 months (Table 4). Three reports were Level I or II studies [59, 65, 94], whereas 16 were Level IV. The two Level I studies reported survival rates of 94% at a mean followup of 56 months (range, 36–72 months) and 98% at a mean followup of 33 months (range, 24–60 months) [56, 78]. The single Level II study reported a survival rate of 95% at a mean followup of 36 months (range, 24–72 months) [59].
Table 4.
Reported survival rates of contemporary metal-on-metal hip resurfacing arthroplasty
| Study | Number of hips (patients) | Type of bearing design | Followup (months)* | Femoral fixation | Acetabular fixation | Survival (%) | Level of evidence |
|---|---|---|---|---|---|---|---|
| Daniel et al. [15] (2010) | 184 (160) | CoCrMo resurfacing | 84 (24–130) | Cemented | Uncemented | 84 | IV |
| Madhu et al. [54] (2010) | 117 (101) | CoCrMo resurfacing | 84 (60–113) | Cemented | Uncemented | 93 | IV |
| Vendittoli et al. [94] (2010) | 109 (NR) | CoCrMo resurfacing | 56 (36–72) | Cemented | Uncemented | 94 | I |
| Bergeron et al. [5] (2009) | 228 (209) | CoCrMo resurfacing | 55 | Cemented | Uncemented | 97† | IV |
| Killampalli et al. [41] (2009) | 100 (100) | CoCrMo resurfacing | NR (24–60) | Cemented | Uncemented | 100 | IV |
| Mont et al. [64] (2009) | 54 (54) | CoCrMo resurfacing | 40 (24–60) | Cemented | Uncemented | 96 | III |
| Ollivere et al. [73] (2009) | 104 (94) | CoCrMo resurfacing | 61 (38–76) | Cemented | Uncemented | 100 | IV |
| Zywiel et al. [101] (2009) | 33 (33) | CoCrMo resurfacing | 45 (24–67) | Cemented | Uncemented | 100 | III |
| Amstutz and LeDuff [1] (2008) | 1000 (838) | CoCrMo resurfacing | 68 (13–133) | Cemented | Uncemented | 95 | IV |
| Falez et al. [24] (2008) | 60 (58) | CoCrMo resurfacing | 32 (2–44) | Cemented | Uncemented | 92 | IV |
| Heilpern et al. [34] (2008) | 110 (98) | CoCrMo resurfacing | 71 (60–93) | Cemented | Uncemented | 96 | IV |
| Kim et al. [42] (2008) | 200 (200) | CoCrMo resurfacing | 31 (12–54) | Cemented | Uncemented | 93 | IV |
| McGrath et al. [59] (2008) | 40 (35) | CoCrMo resurfacing | 36 (24–72) | Cemented | Uncemented | 95 | II |
| Steffen et al. [88] (2008) | 610 (532) | CoCrMo resurfacing | 60 (24–96) | Cemented | Uncemented | 95 | IV |
| Marker et al. [57] (2007) | 550 (NR) | CoCrMo resurfacing | 44 (7–75) | Cemented | Uncemented | 93 | IV |
| Mont et al. [65] (2007) | 1016 (906) | CoCrMo resurfacing | 33 (24–66) | Cemented | Uncemented | 94 | I |
| Nishii et al. [70] (2007) | 50 (45) | CoCrMo resurfacing | 60 | Cemented | Uncemented | 96† | IV |
| Pollard et al. [78] (2006) | 63 (NR) | CoCrMo resurfacing | 61 (52–71) | Cemented | Uncemented | 94 | III |
| Vail et al. [93] (2006) | 57 (52) | CoCrMo resurfacing | 36 (24–48) | Cemented | Uncemented | 97 | III |
| Lilikakis et al. [49] (2005) | 70 (66) | CoCrMo resurfacing | 29 (24–38) | Uncemented | Uncemented | 97 | IV |
| Treacy et al. [92] (2005) | 144 (130) | CoCrMo resurfacing | 60 | Cemented | Uncemented | 98† | IV |
| Daniel et al. [14] (2004) | 446 (384) | CoCrMo resurfacing | 39 (24–98) | Cemented | Uncemented | 99 | IV |
* Values are expressed as mean, with range in parentheses; †survivorship at noted followup time; NR = not reported; CoCrMo = cobalt-chromium-molybdenum.
The 21 studies addressing ceramic-on-ceramic THA reported survival rates of 73% to 100% at mean followups ranging from 31 to 240 months (Table 5). The studies were grouped based on advances in ceramic composition and manufacturing that are beyond the scope of the present report but have been described elsewhere [58, 97]. Eight studies encompassed first-generation alumina bearings [37, 55, 71, 72, 77, 80, 85, 98] predominantly used until the mid 1990 s, before the introduction of improved raw materials and manufacturing technologies. These studies reported survival rates ranging from 96% at an unreported mean followup (range, 2–11 years) to a 73% survival at a mean followup of 37 months (range, 24–52 months). All of these studies were Level IV. Eleven studies reported on second-generation alumina bearings [4, 7, 10, 28, 31, 33, 38, 48, 68, 90, 99], produced with smaller base material grain size, increased material purity, and high-pressure ceramic fusion techniques. Three of these studies were Level I [4, 10, 48] and reported survival rates ranging from 100% at a mean followup of 51 months (range, 34–63 months) to 96% at 8 years. The remaining nine studies were Level III or IV. Two of the studies reported one specific polyethylene-ceramic sandwich construction liner [33, 38] and found lower survival rates of 83% and 91%, respectively. The survival rates in the remaining reports ranged from 94% to 100%. Two studies reported the results of new-generation alumina matrix composite components (for example, combining alumina with specific smaller proportions of zirconia, chromium oxide, and strontium). The Level I study reported 98% survival at a mean followup of 31 months (range, 21–49 months) [32], while the Level II study reported 95% survival at a mean followup of 73 months (range, 26–108 months) [50].
Table 5.
Selected reported survival rates of historical and modern ceramic-on-ceramic bearings
| Study | Number of hips (patients) | Followup (months)* | Survival (%) | Level of evidence |
|---|---|---|---|---|
| Early-generation alumina | ||||
| Petsatodis et al. [77] (2010) | 85 (78) | 240 | 84‡ | IV |
| Huo et al. [37] (1996) | 27 (25) | 73 (60–95) | 85 | IV |
| Riska [80] (1993) | 290 (255) | 64 (24–144) | 92 | IV |
| Nizard et al. [71] (1992) | 187 (172) | 120 | 83‡ | IV |
| Winter et al. [98] (1992) | 100 (100) | NR (120–168) | 75 | IV |
| Mahoney and Dimon [55] (1990) | 42 (34) | 51 (27–66) | 83 | IV |
| Sedel et al. [85] (1990) | 54 (NR) | NR (24–132) | 96 | IV |
| O’Leary et al. [72] (1988) | 69 (62) | 37 (24–52) | 73 | IV |
| Late-generation alumina | ||||
| Lewis et al. [48] (2010) | 30 (30) | 100 (58–121) | 97 | I |
| Bascarevic et al. [4] (2009) | 82 (78) | 51 (34–63) | 100 | I |
| Greene et al. [28] (2009) | 103 (97) | 50 (48–64) | 100 | IV |
| Capello et al. [10] (2008) | 380 (275) | 96 (60–NR) | 96‡ | I |
| Iwakiri et al. [38] (2008) | 82 (77) | 80 (60–100) | 91 | IV |
| Ha et al. [31] (2007) | 74 (64) | 66 (60–72) | 100 | IV |
| Sugano et al. [90] (2007) | 170 (143) | 72 (60–96) | 99 | III |
| Hasegawa et al. [33] (2006) | 35 (30) | 70 (60–77) | 83 | IV |
| Murphy et al. [68] (2006) | 194 (173) | 50 (24–108) | 96 | IV |
| Yoo et al. [99] (2005) | 93 (79) | 68 (60–73) | 100 | IV |
| Bizot et al. [7] (2004) | 71 (62) | 108 | 94‡ | IV |
| Alumina composite | ||||
| Hamilton et al. [32] (2010) | 177 (NR) | 31 (21–49) | 98 | I |
| Lombardi et al. [50] (2010)† | 65 (NR) | 73 (26–108) | 95 | II |
* Values are expressed as mean, with range in parentheses; †study of composite femoral head on pure alumina liner; ‡survivorship at noted followup time; NR = not reported.
We identified no studies reporting survival of ceramic-on-metal THA.
Discussion
Despite the popularity of metal-on-polyethylene articulation usage since THA was first popularized a half-century ago, hard-on-hard bearings have consistently been used, though to a lesser extent. However, their use has been more controversial, with some surgeons advocating the use of hard-on-hard couples in virtually all patients, and others arguing the potential for adverse events preclude their use in virtually all arthroplasty procedures. Achieving a consensus concerning their use has been further complicated by the dominance of case series and case study reports that have a high potential for study bias and for over- or underestimating the true survival rates of these bearings. These factors motivated us to undertake this review to systematically assess the published evidence concerning the survival of several commonly used alternative bearing surfaces for THA.
We acknowledge the following limitations of our study. First, while we have limited our inclusion criteria to reports written in English, some of the bearing couples were developed and used extensively in non-English-speaking countries and their results were reported in several respected native-language journals. For example, much of the research and development of ceramic prostheses occurred, and continues to take place, in France and Germany, and it is likely there are many reports published in French or German that would meet all of our inclusion criteria, with the exception of the language restriction. With English currently being the de facto universal academic language in the Western world and with more than 20 studies included for each of the investigated bearing couples, we believe these studies will provide an overview of the currently known survival rates of these articulating couples. Second, the majority of the studies identified had a nonrandomized design, and the remaining reports had one or more deficiencies in quality compromising internal validity, increasing the potential for selection, performance, attrition, and assessment bias. Furthermore, substantial variability in the study methods and data reporting resulted in considerable heterogeneity and precluded the possibility of accurate aggregation or comparison of the reported findings across multiple studies. Third, there are other factors that may contribute to implant survival that were not included in our analysis and were often not reported in studies, such as differences in femoral and acetabular component design and fixation, femoral head diameter, and implant positioning. Fourth, many of the included reports originate from well-known centers with procedures performed by high-volume subspecialty-trained surgeon-innovators, and the results may not necessarily accurately reflect those that would be achieved by general orthopaedists or those who perform a smaller number of cases on an annual basis. Fifth, because of the relatively recent introduction of modern resurfacing components, the series with longer followups typically involve patients operated on during a period where appropriate patient indications were being explored and components and instrumentation were being developed. However, for all bearing types, the majority of studies, especially those with longer followups, have low levels of evidence (III and IV), raising questions about the potential for positive outcome bias [22, 36, 89] that may not accurately reflect the survival most surgeons can expect to achieve. Additionally, most of the Level I studies have mean followups of 5 years or less, further limiting the ability to discern purported differences in long-term survival in hip arthroplasty among different types of hard-on-hard bearings. This paucity of prospective, comparative studies limits the ability to evaluate the potential advantages in terms of survival of hard-on-hard bearings compared to metal-on-polyethylene articulations. Finally, even when such studies are conducted, they are complicated by the large number of subjects needed for an adequately powered comparison of survival rates. For example, assuming a power of 0.8 and alpha of 0.05, approximately 870 hips would need to be enrolled for a 5% difference in survival rates (95% versus 90%) to reach significance. Even with a 10% difference in survival (95% versus 85%), 280 subjects would be required. Nevertheless, despite these and other potential limitations, we believe our study presents important findings in terms of the short- to mid-term survival rates of contemporary hard-on-hard bearings in hip arthroplasty.
Our findings suggest modern metal-on-metal THA consistently provides survivorship of 95% or more at followups from 3 to 10 years, and it is hoped the large majority of these prostheses will continue to demonstrate similar survival at longer followups. The availability of near-anatomic femoral head sizes and the extremely low in vitro wear rates of these bearings, even when compared to modern crosslinked polyethylene liners, theoretically make them an appropriate choice in young and highly active patients. However, additional clinical evidence and longer followup are needed to confirm these claims.
Modern metal-on-metal hip resurfacing similarly appears to provide survival rates of 95% and more at followup times currently approaching 10 years when performed by experienced surgeons in properly selected patients. This procedure may be especially suitable for young, active patients because it may provide unique benefits in terms of preservation of femoral bone stock, increased postoperative activity levels, and potentially more natural joint biomechanics. However, additional evidence in direct comparison to other hip arthroplasty prostheses is necessary to confirm these suggestions. Additionally, hip resurfacing is a distinct procedure requiring surgeons to learn techniques different from those used for standard THA. It is a technically demanding procedure associated with a substantial learning curve. Intraoperative notching of the femoral neck must be avoided to minimize the risk of postoperative femoral neck fractures [17, 57, 87]. Additionally, adequate acetabular cup coverage and appropriate femoral component positioning, as well as removal of all osteophytes, are necessary to minimize the likelihood of impingement and/or groin pain [6, 46]. Finally, proper case selection is critical as patients with poor bone quality (due to osteopenia or extensive osteonecrosis of the femoral head), large femoral head or neck cysts, or smaller femoral neck sizes are susceptible to catastrophic femoral neck fractures [65].
While early ceramic-on-ceramic implants were characterized by high failure rates as a result of both component fracture and loosening of the monolithic acetabular components, advances in component design and manufacturing technology have resulted in modern implants having substantially higher survival rates, very low wear, and an extremely low incidence of femoral head fracture (0.19% combined in the studies included in the present analysis, and an estimated 0.012% in the largest reported series to date of approximately 500,000 femoral heads [97]). Nonetheless, concerns remain about the possibility of component chipping and noisy implants. Ongoing research and advances in ceramic technology and implant design may succeed in addressing these disadvantages in the future [3, 12, 79]. Recently, some authors have recommended the use of a ceramic-on-highly-crosslinked polyethylene bearing in younger active patients, which is postulated to provide low wear rates while minimizing the possibility of component chipping or squeaking. In a prospective randomized study of 177 modern ceramic-on-ceramic and 87 ceramic-on-highly-crosslinked polyethylene THAs, Hamilton et al. [32] reported similar survivorship and complication rates in both groups at a mean followup of 31 months (range, 21–49 months), with no squeaking reported in either group. Data from other investigators and over longer followup periods are needed to ascertain whether this is an appropriate alternative.
The use of ceramic-on-metal bearing couples has been proposed as an alternative that may provide benefits in terms of wear similar to those of ceramic-on-ceramic articulations, while further decreasing the incidence of component chipping or squeaking. However, while investigative studies are underway to assess these potential benefits, no currently published evidence was identified to support these claims.
Although not specifically assessed in our review, there has been a recent increase in concern among the orthopaedic community about the potential for both local and systemic distribution of metal debris and especially with the potential for adverse local tissue reactions. A number of reports from the Nuffield Orthopaedic Centre in Oxford, United Kingdom, have provided some insight into these complications. Pandit et al. [76] reported symptomatic pseudotumors in 20 hips treated with metal-on-metal hip resurfacing in 17 patients and estimated the incidence of this complication at 1%. Kwon et al. [44] suggested the incidence of asymptomatic pseudotumors after hip resurfacing may be as high as 6.5%, with almost all identified cases occurring in patients with implant sizes of 50 mm or less. Glyn-Jones et al. [25] suggested the incidence of symptomatic pseudotumors may increase with time. A subsequent report from Kwon et al. [43] identified a higher wear rate in resurfacing patients revised for symptomatic tissue reactions as compared to those revised for other reasons with evident edge loading of retrieved components in all cases. Interestingly, these reactions are not limited to metal-on-metal articulations. Svensson et al. [91] reported a case of pseudotumor formation 2.5 years after uncemented metal-on-polyethylene THA associated with corrosion at the prosthesis head-neck junction. While adverse local tissue reactions do appear to be associated with abnormally high metal particle generation rates secondary to factors such as poor implant positioning and/or suboptimal prosthesis design [2, 18, 44, 45], the causes are likely multifactorial and the true incidence remains unknown. However, it is clear these adverse local tissue reactions, if not identified and revised promptly, can result in substantial periarticular soft tissue destruction and poor outcomes of revision surgery [26]. Although national joint registry data suggest overall revision rates of modern standard head size metal-on-metal articulations appear to be similar to, or lower than, those found with metal-on-ceramic and ceramic-on-ceramic articulations [27], in the absence of additional evidence to more accurately assess the incidence and predisposing factors of adverse reactions, patients should be made aware of the risks associated with these bearings. Their use should be approached with caution in women of childbearing age and avoided in patients with a history of metal sensitivity. Nevertheless, even a relatively low incidence of these complications may be unacceptable to both surgeons and patients, and the use of metal-on-metal articulations may decrease unless they can be reliably avoided. As a result, it is critical a full understanding of the factors leading to these reactions be achieved to further reduce their incidence.
In general, while hip arthroplasties using earlier-generation hard-on-hard bearings had more variable survival rates, contemporary designs are consistently reported to have good survival rates. The majority of authors reported 95% or more of stemmed THA implants remain in situ, regardless of the specific bearing couple used at mean followups of between 3 and 10 years. It is worth noting, though, some of the clinical successes may have been the result of improvements in implant fixation techniques and design parameters. The survival rates for hip resurfacing are somewhat more variable.
High short- and mid-term survival rates have been reported by a number of investigators with each of the studied hard-on-hard bearings. Adverse events from many of these hard-on-hard bearings can be minimized by appropriate patient selection and surgical technique. As bearing designs continue to improve with new and modified materials, improved manufacturing techniques, and a better understanding of factors associated with potential adverse reactions, the use of hard-on-hard bearings may increase, especially in young and active patients. However, an increased emphasis in the orthopaedic community on well-designed prospective comparative studies, high-quality systematic reviews, and the development of a comprehensive joint registry are critical to accurately assess many of the potential advantages and disadvantages ascribed to these developing technologies, as well as the influence of various patient and implant factors on outcomes and survival rates.
Footnotes
Michael A. Mont is a consultant for Stryker Orthopaedics (Mahwah, NJ) and Wright Medical Technology, Inc (Arlington, TN), receives royalties from Stryker, and receives research or institutional support from Stryker, Wright Medical, the National Institutes of Health (NIAMS and NICHD), and TissueGene, Inc (Rockville, MD). Thomas P. Schmalzried is a board member of the Orthopaedic Research and Education Foundation, is a member of the editorial board for Orthopedics Today, receives royalties from DePuy Orthopaedics, Inc (Warsaw, IN) and Stryker, is a consultant for Stryker, receives research or institutional support from DePuy and Stryker, and holds stock or stock options in Johnson and Johnson, Smith and Nephew, Stryker, and Zimmer, Inc (Warsaw, IN). Michael G. Zywiel serves on the editorial board of Expert Review of Medical Devices. The remaining authors certify that they have no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This work was performed at Sinai Hospital of Baltimore.
References
- 1.Amstutz HC, Le Duff MJ. Eleven years of experience with metal-on-metal hybrid hip resurfacing: a review of 1000 conserve plus. J Arthroplasty. 2008;23:36–43. doi: 10.1016/j.arth.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 2.Aroukatos P, Repanti M, Repantis T, Bravou V, Korovessis P. Immunologic adverse reaction associated with low-carbide metal-on-metal bearings in total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2135–2142. doi: 10.1007/s11999-009-1187-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bal BS, Khandkar A, Lakshminarayanan R, Clarke I, Hoffman AA, Rahaman MN. Testing of silicon nitride ceramic bearings for total hip arthroplasty. J Biomed Mater Res B Appl Biomater. 2008;87:447–454. doi: 10.1002/jbm.b.31123. [DOI] [PubMed] [Google Scholar]
- 4.Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, Timotijevic S. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. November 1, 2009 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 5.Bergeron SG, Desy NM, Nikolaou VS, Debiparshad K, Antoniou J. The early results of metal-on-metal hip resurfacing: a prospective study at a minimum two-year follow-up. Bull NYU Hosp Jt Dis. 2009;67:132–134. [PubMed] [Google Scholar]
- 6.Bin Nasser A, Beaule PE, O’Neill M, Kim PR, Fazekas A. Incidence of groin pain after metal-on-metal hip resurfacing. Clin Orthop Relat Res. 2010;468:392–399. doi: 10.1007/s11999-009-1133-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bizot P, Hannouche D, Nizard R, Witvoet J, Sedel L. Hybrid alumina total hip arthroplasty using a press-fit metal-backed socket in patients younger than 55 years: a six- to 11-year evaluation. J Bone Joint Surg Br. 2004;86:190–194. doi: 10.1302/0301-620X.86B2.14026. [DOI] [PubMed] [Google Scholar]
- 8.Bradford L, Baker DA, Graham J, Chawan A, Ries MD, Pruitt LA. Wear and surface cracking in early retrieved highly cross-linked polyethylene acetabular liners. J Bone Joint Surg Am. 2004;86:1271–1282. doi: 10.2106/00004623-200406000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Brown SR, Davies WA, DeHeer DH, Swanson AB. Long-term survival of McKee-Farrar total hip prostheses. Clin Orthop Relat Res. 2002;402:157–163. doi: 10.1097/00003086-200209000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Capello WN, D’Antonio JA, Feinberg JR, Manley MT, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty. 2008;23:39–43. doi: 10.1016/j.arth.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Centre for Evidence-based Medicine. CEBM Levels of Evidence. Available at: http://www.cebm.net/index.aspx?o=5653. Accessed April 28, 2010.
- 12.Chevillotte C, Trousdale RT, Chen Q, Guyen O, An KN. The 2009 Frank Stinchfield Award. “Hip squeaking”: a biomechanical study of ceramic-on-ceramic bearing surfaces. Clin Orthop Relat Res. 2010;468:345–350. doi: 10.1007/s11999-009-0911-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dandy DJ, Theodorou BC. The management of local complications of total hip replacement by the McKee-Farrar technique. J Bone Joint Surg Br. 1975;57:30–35. [PubMed] [Google Scholar]
- 14.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 15.Daniel J, Ziaee H, Kamali A, Pradhan C, Band T, McMinn DJ. Ten-year results of a double-heat-treated metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2010;92:20–27. doi: 10.2106/JBJS.H.01821. [DOI] [PubMed] [Google Scholar]
- 16.Dastane MR, Long WT, Wan Z, Chao L, Dorr LD. Metal-on-metal hip arthroplasty does equally well in osteonecrosis and osteoarthritis. Clin Orthop Relat Res. 2008;466:1148–1153. doi: 10.1007/s11999-008-0180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis ET, Olsen M, Zdero R, Papini M, Waddell JP, Schemitsch EH. A biomechanical and finite element analysis of femoral neck notching during hip resurfacing. J Biomech Eng. 2009;131:041002. doi: 10.1115/1.3072889. [DOI] [PubMed] [Google Scholar]
- 18.Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291–1297. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]
- 19.Delaunay CP, Bonnomet F, Clavert P, Laffargue P, Migaud H. THA using metal-on-metal articulation in active patients younger than 50 years. Clin Orthop Relat Res. 2008;466:340–346. doi: 10.1007/s11999-007-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation: four to seven-year results. J Bone Joint Surg Am. 2000;82:789–798. doi: 10.2106/00004623-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Dumbleton JH, D’Antonio JA, Manley MT, Capello WN, Wang A. The basis for a second-generation highly cross-linked UHMWPE. Clin Orthop Relat Res. 2006;453:265–271. doi: 10.1097/01.blo.0000238856.61862.7d. [DOI] [PubMed] [Google Scholar]
- 22.Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991;337:867–872. doi: 10.1016/0140-6736(91)90201-Y. [DOI] [PubMed] [Google Scholar]
- 23.Eswaramoorthy V, Moonot P, Kalairajah Y, Biant LC, Field RE. The Metasul metal-on-metal articulation in primary total hip replacement: clinical and radiological results at ten years. J Bone Joint Surg Br. 2008;90:1278–1283. doi: 10.1302/0301-620X.90B10.20378. [DOI] [PubMed] [Google Scholar]
- 24.Falez F, Favetti F, Casella F, Panegrossi G. Hip resurfacing: why does it fail? Early results and critical analysis of our first 60 cases. Int Orthop. 2008;32:209–216. doi: 10.1007/s00264-006-0313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glyn-Jones S, Pandit H, Kwon YM, Doll H, Gill HS, Murray DW. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009;91:1566–1574. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 26.Grammatopolous G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, Murray DW, Gill HS. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009;91:1019–1024. doi: 10.1302/0301-620X.91B8.22562. [DOI] [PubMed] [Google Scholar]
- 27.Graves S, Davidson D, Steiger R, Tomkins A, Ryan P, Griffith L, McDermott B, Pratt N, Miller L, Stanford T. National Joint Replacement Registry Annual Report. Australia: Adelaide; 2008. [Google Scholar]
- 28.Greene JW, Malkani AL, Kolisek FR, Jessup NM, Baker DL. Ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2009;24:15–18. doi: 10.1016/j.arth.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 29.Grobbelaar CJ, du Plessis TA, Marais F. The radiation improvement of polyethylene prostheses: a preliminary study. J Bone Joint Surg Br. 1978;60:370–374. doi: 10.1302/0301-620X.60B3.681412. [DOI] [PubMed] [Google Scholar]
- 30.Grubl A, Marker M, Brodner W, Giurea A, Heinze G, Meisinger V, Zehetgruber H, Kotz R. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res. 2007;25:841–848. doi: 10.1002/jor.20381. [DOI] [PubMed] [Google Scholar]
- 31.Ha YC, Koo KH, Jeong ST, Joon Yoo J, Kim YM, Joong Kim H. Cementless alumina-on-alumina total hip arthroplasty in patients younger than 50 years: a 5-year minimum follow-up study. J Arthroplasty. 2007;22:184–188. doi: 10.1016/j.arth.2006.02.169. [DOI] [PubMed] [Google Scholar]
- 32.Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010;468:358–366. doi: 10.1007/s11999-009-1091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hasegawa M, Sudo A, Uchida A. Alumina ceramic-on-ceramic total hip replacement with a layered acetabular component. J Bone Joint Surg Br. 2006;88:877–882. doi: 10.1302/0301-620X.88B7.17675. [DOI] [PubMed] [Google Scholar]
- 34.Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90:1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 35.Higuchi F, Inoue A, Semlitsch M. Metal-on-metal CoCrMo McKee-Farrar total hip arthroplasty: characteristics from a long-term follow-up study. Arch Orthop Trauma Surg. 1997;116:121–124. doi: 10.1007/BF00426058. [DOI] [PubMed] [Google Scholar]
- 36.Hopewell S, Loudon K, Clarke MJ, Oxman AD, Dickersin K. Publication bias in clinical trials due to statistical significance or direction of trial results. Cochrane Database Syst Rev. 2009:MR000006. [DOI] [PMC free article] [PubMed]
- 37.Huo MH, Martin RP, Zatorski LE, Keggi KJ. Cementless total hip arthroplasties using ceramic-on-ceramic articulation in young patients: a minimum 5-year follow-up study. J Arthroplasty. 1996;11:673–678. doi: 10.1016/S0883-5403(96)80005-2. [DOI] [PubMed] [Google Scholar]
- 38.Iwakiri K, Iwaki H, Minoda Y, Ohashi H, Takaoka K. Alumina inlay failure in cemented polyethylene-backed total hip arthroplasty. Clin Orthop Relat Res. 2008;466:1186–1192. doi: 10.1007/s11999-008-0168-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacobs M, Gorab R, Mattingly D, Trick L, Southworth C. Three- to six-year results with the Ultima metal-on-metal hip articulation for primary total hip arthroplasty. J Arthroplasty. 2004;19:48–53. doi: 10.1016/j.arth.2004.06.021. [DOI] [PubMed] [Google Scholar]
- 40.Kanao Y. An experimental study on the wear of HDP socket in total hip arthroplasty: quantification of worn surface by SEM 3-D image analysis and effect of gamma-ray-irradiation of HDP on improving tolerance to wear [in Japanese] Nippon Seikeigeka Gakkai Zasshi. 1992;66:291–301. [PubMed] [Google Scholar]
- 41.Killampalli VV, Hayes A, Parsons N, Costa ML, Prakash U. Hip resurfacing using the trochanteric flip osteotomy. Hip Int. 2009;19:131–135. doi: 10.1177/112070000901900209. [DOI] [PubMed] [Google Scholar]
- 42.Kim PR, Beaule PE, Laflamme GY, Dunbar M. Causes of early failure in a multicenter clinical trial of hip resurfacing. J Arthroplasty. 2008;23:44–49. doi: 10.1016/j.arth.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 43.Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, Murray DW. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. J Bone Joint Surg Br. 2010;92:356–361. doi: 10.1302/0301-620X.92B3.23281. [DOI] [PubMed] [Google Scholar]
- 44.Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. “Asymptomatic” pseudotumors after metal-on-metal hip resurfacing arthroplasty prevalence and metal ion study. J Arthroplasty. June 28, 2010 [Epub ahead of print]. [DOI] [PubMed]
- 45.Langton DJ, Sprowson AP, Joyce TJ, Reed M, Carluke I, Partington P, Nargol AV. Blood metal ion concentrations after hip resurfacing arthroplasty: a comparative study of articular surface replacement and Birmingham Hip Resurfacing arthroplasties. J Bone Joint Surg Br. 2009;91:1287–1295. doi: 10.1302/0301-620X.91B10.22308. [DOI] [PubMed] [Google Scholar]
- 46.Lavigne M, Rama KR, Roy A, Vendittoli PA. Painful impingement of the hip joint after total hip resurfacing: a report of two cases. J Arthroplasty. 2008;23:1074–1079. doi: 10.1016/j.arth.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 47.Learmonth ID. Total hip replacement and the law of diminishing returns. J Bone Joint Surg Am. 2006;88:1664–1673. doi: 10.2106/JBJS.F.00218. [DOI] [PubMed] [Google Scholar]
- 48.Lewis PM, Al-Belooshi A, Olsen M, Schemitch EH, Waddell JP. Prospective randomized trial comparing alumina ceramic-on-ceramic with ceramic-on-conventional polyethylene bearings in total hip arthroplasty. J Arthroplasty. 2010;25:392–397. doi: 10.1016/j.arth.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 49.Lilikakis AK, Vowler SL, Villar RN. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: minimum of two years follow-up. Orthop Clin North Am. 2005;36:215–222. doi: 10.1016/j.ocl.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Lombardi AV, Jr, Berend KR, Seng BE, Clarke IC, Adams JB. Delta ceramic-on-alumina ceramic articulation in primary THA: prospective, randomized FDA-IDE study and retrieval analysis. Clin Orthop Relat Res. 2010;468:367–374. doi: 10.1007/s11999-009-1143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lombardi AV, Jr, Mallory TH, Alexiades MM, Cuckler JM, Faris PM, Jaffe KA, Keating EM, Nelson CL, Jr, Ranawat CS, Williams J, Wixson R, Hartman JF, Capps SG, Kefauver CA. Short-term results of the M2a-taper metal-on-metal articulation. J Arthroplasty. 2001;16:122–128. doi: 10.1054/arth.2001.29307. [DOI] [PubMed] [Google Scholar]
- 52.Long WT, Dorr LD, Gendelman V. An American experience with metal-on-metal total hip arthroplasties: a 7-year follow-up study. J Arthroplasty. 2004;19:29–34. doi: 10.1016/j.arth.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 53.MacDonald SJ, McCalden RW, Chess DG, Bourne RB, Rorabeck CH, Cleland D, Leung F. Metal-on-metal versus polyethylene in hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2003;406:282–296. doi: 10.1097/00003086-200301000-00039. [DOI] [PubMed] [Google Scholar]
- 54.Madhu TS, Akula MR, Raman RN, Sharma HK, Johnson VG. The Birmingham hip resurfacing prosthesis: an independent single surgeon’s experience at 7-year follow-up. J Arthroplasty. January 5, 2010 [Epub ahead of print]. [DOI] [PubMed]
- 55.Mahoney OM, Dimon JH., 3rd Unsatisfactory results with a ceramic total hip prosthesis. J Bone Joint Surg Am. 1990;72:663–671. [PubMed] [Google Scholar]
- 56.Manley MT, Sutton K. Bearings of the future for total hip arthroplasty. J Arthroplasty. 2008;23:47–50. doi: 10.1016/j.arth.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 57.Marker DR, Seyler TM, Jinnah RH, Delanois RE, Ulrich SD, Mont MA. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty. 2007;22:66–71. doi: 10.1016/j.arth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 58.Masson B. Emergence of the alumina matrix composite in total hip arthroplasty. Int Orthop. 2009;33:359–363. doi: 10.1007/s00264-007-0484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McGrath MS, Desser DR, Ulrich SD, Seyler TM, Marker DR, Mont MA. Total hip resurfacing in patients who are sixty years of age or older. J Bone Joint Surg Am. 2008;90(Suppl 3):27–31. doi: 10.2106/JBJS.H.00464. [DOI] [PubMed] [Google Scholar]
- 60.McKee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee-Farrar prosthesis. J Bone Joint Surg Br. 1966;48:245–259. [PubMed] [Google Scholar]
- 61.McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Development of an extremely wear-resistant ultra high molecular weight polyethylene for total hip replacements. J Orthop Res. 1999;17:157–167. doi: 10.1002/jor.1100170203. [DOI] [PubMed] [Google Scholar]
- 62.Mendenhall Associates Inc. 2009 Hip and Knee Implant Review. Orthop Network News. 2009;20:1–20.
- 63.Milosev I, Trebse R, Kovac S, Cor A, Pisot V. Survivorship and retrieval analysis of Sikomet metal-on-metal total hip replacements at a mean of seven years. J Bone Joint Surg Am. 2006;88:1173–1182. doi: 10.2106/JBJS.E.00604. [DOI] [PubMed] [Google Scholar]
- 64.Mont MA, Marker DR, Smith JM, Ulrich SD, McGrath MS. Resurfacing is comparable to total hip arthroplasty at short-term follow-up. Clin Orthop Relat Res. 2009;467:66–71. doi: 10.1007/s11999-008-0465-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mont MA, Seyler TM, Ulrich SD, Beaule PE, Boyd HS, Grecula MJ, Goldberg VM, Kennedy WR, Marker DR, Schmalzried TP, Sparling EA, Vail TP, Amstutz HC. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 66.Morrison ML, Jani S. Evaluation of sequentially crosslinked ultra-high molecular weight polyethylene. J Biomed Mater Res B Appl Biomater. 2009;90:87–100. doi: 10.1002/jbm.b.31257. [DOI] [PubMed] [Google Scholar]
- 67.Muratoglu OK, Bragdon CR, O’Connor DO, Jasty M, Harris WH. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty. 2001;16:149–160. doi: 10.1054/arth.2001.20540. [DOI] [PubMed] [Google Scholar]
- 68.Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102. doi: 10.1097/01.blo.0000246532.59876.73. [DOI] [PubMed] [Google Scholar]
- 69.Neumann DR, Thaler C, Hitzl W, Huber M, Hofstadter T, Dorn U. Long-term results of a contemporary metal-on-metal total hip arthroplasty: a 10-year follow-up study. J Arthroplasty. 2010;25:700–708. doi: 10.1016/j.arth.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 70.Nishii T, Sugano N, Miki H, Takao M, Koyama T, Yoshikawa H. Five-year results of metal-on-metal resurfacing arthroplasty in Asian patients. J Arthroplasty. 2007;22:176–183. doi: 10.1016/j.arth.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 71.Nizard RS, Sedel L, Christel P, Meunier A, Soudry M, Witvoet J. Ten-year survivorship of cemented ceramic-ceramic total hip prosthesis. Clin Orthop Relat Res. 1992;282:53–63. [PubMed] [Google Scholar]
- 72.O’Leary JF, Mallory TH, Kraus TJ, Lombardi AV, Jr, Lye CL. Mittelmeier ceramic total hip arthroplasty: a retrospective study. J Arthroplasty. 1988;3:87–96. doi: 10.1016/S0883-5403(88)80057-3. [DOI] [PubMed] [Google Scholar]
- 73.Ollivere B, Duckett S, August A, Porteous M. The Birmingham hip resurfacing: 5-year clinical and radiographic results from a district general hospital. Int Orthop. 2010;34:631–634. doi: 10.1007/s00264-009-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Oral E, Christensen SD, Malhi AS, Wannomae KK, Muratoglu OK. Wear resistance and mechanical properties of highly cross-linked, ultrahigh-molecular weight polyethylene doped with vitamin E. J Arthroplasty. 2006;21:580–591. doi: 10.1016/j.arth.2005.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Paleochorlidis IS, Badras LS, Skretas EF, Georgaklis VA, Karachalios TS, Malizos KN. Clinical outcome study and radiological findings of Zweymuller metal on metal total hip arthroplasty: a follow-up of 6 to 15 years. Hip Int. 2009;19:301–308. doi: 10.1177/112070000901900402. [DOI] [PubMed] [Google Scholar]
- 76.Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- 77.Petsatodis GE, Papadopoulos PP, Papavasiliou KA, Hatzokos IG, Agathangelidis FG, Christodoulou AG. Primary cementless total hip arthroplasty with an alumina ceramic-on-ceramic bearing: results after a minimum of twenty years of follow-up. J Bone Joint Surg Am. 2010;92:639–644. doi: 10.2106/JBJS.H.01829. [DOI] [PubMed] [Google Scholar]
- 78.Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip: a five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 79.Restrepo C, Post ZD, Kai B, Hozack WJ. The effect of stem design on the prevalence of squeaking following ceramic-on-ceramic bearing total hip arthroplasty. J Bone Joint Surg Am. 2010;92:550–557. doi: 10.2106/JBJS.H.01326. [DOI] [PubMed] [Google Scholar]
- 80.Riska EB. Ceramic endoprosthesis in total hip arthroplasty. Clin Orthop Relat Res. 1993;297:87–94. [PubMed] [Google Scholar]
- 81.Rose RM, Cimino WR, Ellis E, Crugnola AN. Exploratory investigations on the structure dependence of the wear resistance of polyethylene. Wear. 1982;77:89–104. doi: 10.1016/0043-1648(82)90048-5. [DOI] [Google Scholar]
- 82.Ryan R, Hill S, Broclain D, Horey D, Oliver S, Prictor M. Study Quality Guide. Cochrane Consumers and Communication Review Group; 2007. Available at: http://www.latrobe.edu.au/chcp/assets/downloads/StudyQualityGuide050307.pdf. Accessed July 12, 2010.
- 83.Saito S, Ryu J, Watanabe M, Ishii T, Saigo K. Midterm results of Metasul metal-on-metal total hip arthroplasty. J Arthroplasty. 2006;21:1105–1110. doi: 10.1016/j.arth.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 84.Sanfilippo JA, Austin MS. Implants for total hip arthroplasty. Expert Rev Med Devices. 2006;3:769–776. doi: 10.1586/17434440.3.6.769. [DOI] [PubMed] [Google Scholar]
- 85.Sedel L, Kerboull L, Christel P, Meunier A, Witvoet J. Alumina-on-alumina hip replacement: results and survivorship in young patients. J Bone Joint Surg Br. 1990;72:658–663. doi: 10.1302/0301-620X.72B4.2380223. [DOI] [PubMed] [Google Scholar]
- 86.Sharma S, Vassan U, Bhamra MS. Metal-on-metal total hip joint replacement: a minimum follow-up of five years. Hip Int. 2007;17:70–77. doi: 10.1177/112070000701700203. [DOI] [PubMed] [Google Scholar]
- 87.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 88.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90:436–441. doi: 10.1302/0301-620X.90B4.19648. [DOI] [PubMed] [Google Scholar]
- 89.Stern JM, Simes RJ. Publication bias: evidence of delayed publication in a cohort study of clinical research projects. BMJ. 1997;315:640–645. doi: 10.1136/bmj.315.7109.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br. 2007;89:455–460. doi: 10.1302/0301-620X.89B4.18458. [DOI] [PubMed] [Google Scholar]
- 91.Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty: a case report. J Bone Joint Surg Am. 1988;70:1238–1242. [PubMed] [Google Scholar]
- 92.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 93.Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123–131. doi: 10.1097/01.blo.0000238852.08497.92. [DOI] [PubMed] [Google Scholar]
- 94.Vendittoli PA, Ganapathi M, Roy AG, Lusignan D, Lavigne M. A comparison of clinical results of hip resurfacing arthroplasty and 28 mm metal on metal total hip arthroplasty: a randomised trial with 3–6 years follow-up. Hip Int. 2010;20:1–13. doi: 10.1177/112070001002000101. [DOI] [PubMed] [Google Scholar]
- 95.Wagner M, Wagner H. Medium-term results of a modern metal-on-metal system in total hip replacement. Clin Orthop Relat Res. 2000;379:123–133. doi: 10.1097/00003086-200010000-00015. [DOI] [PubMed] [Google Scholar]
- 96.Weber BG. Experience with the Metasul total hip bearing system. Clin Orthop Relat Res. 1996;329:S69–S77. doi: 10.1097/00003086-199608001-00007. [DOI] [PubMed] [Google Scholar]
- 97.Willmann G. Ceramic femoral head retrieval data. Clin Orthop Relat Res. 2000;379:22–28. doi: 10.1097/00003086-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 98.Winter M, Griss P, Scheller G, Moser T. Ten- to 14-year results of a ceramic hip prosthesis. Clin Orthop Relat Res. 1992;282:73–80. [PubMed] [Google Scholar]
- 99.Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87:530–535. doi: 10.2106/JBJS.D.01753. [DOI] [PubMed] [Google Scholar]
- 100.Zijlstra WP, Cheung J, Sietsma MS, Raay JJ, Deutman R. No superiority of cemented metal-on-metal vs metal-on-polyethylene THA at 5-year follow-up. Orthopedics. 2009;32:479. doi: 10.3928/01477447-20090527-06. [DOI] [PubMed] [Google Scholar]
- 101.Zywiel MG, Marker DR, McGrath MS, Delanois RE, Mont MA. Resurfacing matched to standard total hip arthroplasty by preoperative activity levels: a comparison of postoperative outcomes. Bull NYU Hosp Jt Dis. 2009;67:116–119. [PubMed] [Google Scholar]