Abstract
Background
Pelvic radiographs are helpful in assessing limb-length discrepancy (LLD) before and after THA but are subject to variation. Different methods are used to determine LLDs. As a pelvic reference, both ischial tuberosities and the teardrops are used, and as a femoral reference, the lesser trochanter and center of the femoral head are used.
Questions/purposes
We validated the different methods for preoperative radiographic measurement of LLDs and evaluated their reliability.
Patients and Methods
LLDs were measured on full-leg radiographs for 52 patients (29 men, 23 women) with osteoarthritis (OA) of the hip and compared with different methods for measuring LLDs on AP radiographs of the pelvis.
Results
The true LLD varied from −8.0 to 9.1 mm. When the biischial line was used as a pelvic reference, the LLD measured on AP pelvis radiographs was different from the true LLD. No difference was found when the interteardrop line was used as a pelvic reference. There was substantial interobserver agreement when the lesser trochanter was used as a femoral reference (kappa = 0.66–0.70) and excellent interobserver and intraobserver agreement for all other measurements (kappa = 0.84–0.93).
Conclusions
Our data show use of the biischial line as a pelvic reference should be discouraged and the interteardrop line is a better alternative. The center of the femoral head is a more reliable femoral landmark compared with the lesser trochanter.
Level of Evidence
Level I, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Preoperative templating is essential to the orthopaedic surgeon for preoperatively evaluating and planning many aspects of a THA. The benefits of templating include accurate prediction of prosthetic size, subsequent optimization of prosthetic longevity, and minimization of intraoperative complications [5]. Furthermore, preoperative templating helps to achieve appropriate offset and limb-length equality, which would lead to better abductor muscle function, less limping, and decreased need for walking aids [7].
Although limb lengthening may be required to provide a stable hip [2], a LLD not only is associated with patient dissatisfaction [36], but also is the most common reason for litigation after THA [19]. LLD after THA has been associated with complications, including sciatic, femoral, and peroneal nerve palsies [32, 34, 46, 50]; low back pain [1, 9, 13, 14]; abnormal gait [17, 26]; and dislocation [56].
It is well-recognized that preoperative pelvic radiographs are helpful in assessing LLD but also are subject to variation because of changes in the position of limbs and pelvis. Different methods are used to determine the LLD (Table 1). As a pelvic reference, both ischial tuberosities and the teardrops are used. On the femoral side, the lesser trochanter and center of the femoral head are used. LLD is expressed as the difference of the distance between a femoral and a pelvic landmark on both sides.
Table 1.
Different methods used to determine LLDs on an AP pelvic radiograph
| Study | Landmark | |||
|---|---|---|---|---|
| Pelvis | Femur | |||
| IT | BI | LT | CH | |
| Austin et al. [2] (2003) | x | x | ||
| Bono [5] (2004) | x | x | ||
| Clark et al. [8] (2006) | x | x | ||
| Eggli et al. [12] (1998) | x | x | ||
| Gonzalez Della Valle et al. [15] (2005) | x | x | ||
| Hoikka et al. [20] (1991) | x | x | ||
| Khanduja et al. [23] (2006) | x | x | ||
| Konyves and Bannister [24] (2005) | x | x | ||
| Krishnan et al. [25] (2006) | x | x | ||
| Maloney and Keeney [29] (2004) | x | x | ||
| Matsuda et al. [30] (2006) | x | x | ||
| Mihalko et al. [32] (2001) | x | x | ||
| Murphy and Ecker [33] (2007) | x | x | ||
| Parvizi et al. [35] (2003) | x | x | ||
| Ranawat and Rodriguez [38] (1997) | x | x | ||
| Rand and Ilstrup [39] (1983) | x | x | ||
| Sathappan et al. [42] (2008) | x | x | ||
| Suh et al. [47] (2004) | x | x | ||
| Unnanuntana et al. [49] (2009) | x | x | ||
| Wedemeyer et al. [51] (2008) | x | x | ||
| White and Dougall [53] (2002) | x | x | ||
| Williamson and Reckling [54] (1978) | x | x | ||
| Woo and Morrey [56] (1982) | x | x | ||
| Woolson et al. [58] (1999) | x | x | ||
IT = interteardrop line; BI = biischial line; LT = tip of the lesser trochanter; CH = center of the femoral head.
We validated the different methods for preoperative radiographic measurement of LLDs and evaluated their reliability. Specifically, we wished to assess how measurement of LLDs using specific landmarks on pelvic films compared with LLDs measured from standing long-leg films to determine which landmarks provide the most reliable accuracy. Our null hypothesis is that there is no difference between the LLD measured on full-leg radiographs and LLD measured on pelvic radiographs in patients with OA of the hip. We also wished to assess the intraobserver reproducibility of LLD measurements on pelvic films.
Patients and Methods
Seventy consecutive patients with OA of the hip undergoing THAs had standing AP full-leg radiographs to measure LLD preoperatively. All radiographs were stored on a Picture Archiving and Communication System (PACS; Agfa HealthCare, Mortsel, Belgium). A long ruler was placed along the lower limb at the level of the hip and used for scaling. Measurements were performed using specialized planning software (MediCAD Planning Version V2.04, MediCAD Multimedia, London, UK) with a precision of 0.1 mm.
Only the radiographs complying with the following criteria were used [25]: (1) no significant deformity of the femoral head; (2) no developmental dysplasia; (3) no obvious disorder of the lower limb that could be another cause of LLD; (4) no previous arthroplasty of the hip, knee, or ankle; (5) no clinical evidence for flexion contractures of the hip or knee; (6) similar size of the lesser trochanter and the degree of overlap of the medial cortex of the greater trochanter on both sides to exclude asymmetric rotation of both legs [10]; (7) distance between the symphysis and the sacrococcygeal joint of approximately 30 mm (range, 10–40 mm) in men compared with 50 mm (range, 40–60 mm) in women to exclude abnormal pelvic tilt in the sagittal plane [45, 48]; and (8) coccyx centered on the pubic symphysis to exclude rotation of the pelvis in the transverse plane [48].
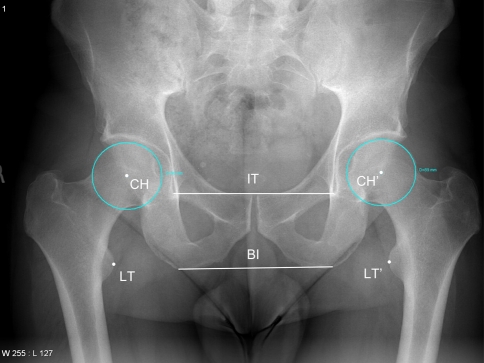
Only 52 of 70 standing AP full-leg radiographs met the inclusion criteria (29 men, 23 women). The mean age of the patients was 68.4 years (range, 49–78 years). On the pelvis of the same film, four points and lines were marked to make measurements: (1) the center of the femoral head (CH) was marked using concentric circles, which automatically demarcated the center of the circle; (2) the tip of the lesser trochanter (LT); (3) the biischial line (BI), which connects the caudal margins of the ischial tuberosities; and (4) the interteardrop line (IT), which connects the caudal margins of the teardrops (Fig. 1).
Fig. 1.
An AP radiograph of the pelvis shows the different landmarks marked to measure LLD. CH = center of the femoral head; LT = tip of the lesser trochanter; BI = biischial line; IT = interteardrop line.
True LLD was measured as the difference in distance between the hip center and the ankle center [28]. Radiographic assessment of a LLD on the pelvis was performed by using the IT and the BI as a pelvic reference. A line was drawn perpendicular to these lines and passing through the femoral references (CH and LT). The distance between these landmarks (IT-CH, IT-LT, BI-CH, and BI-LT) was calculated. The difference in distance between both sides was used to assess LLD on the pelvic radiographs.
Intraobserver and interobserver variations were determined from all selected sets of radiographs measured initially and after 3 weeks by the same author (GM) and by another author (AM) who conducted an independent assessment.
Statistical analysis was performed using Graphpad PRISM® 5.00 (Graphpad, San Diego, CA, USA) and SPSS® Statistical Software (Version 15.0; SPSS Inc, Chicago, IL, USA). An ANOVA test with Bonferroni’s multiple comparison test was used to compare measurements on the pelvis with the true LLD. Intraclass correlation was measured and evaluated using the grouping recommended by Landis and Koch [27]. Scores between 0.61 and 0.8 represented substantial agreements and those greater than 0.81 almost perfect agreements.
Results
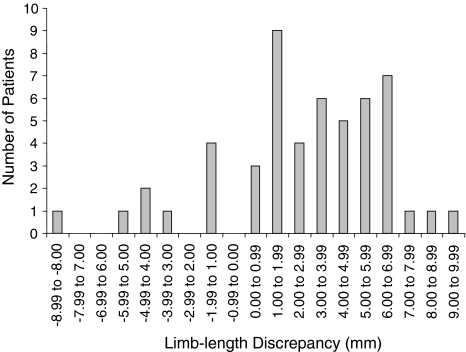
The mean true LLD was 3.88 mm (range, −8.0 to 9.1 mm). In 41 patients (78.9%), the leg with osteoarthritic changes at the level of the hip was shorter than the contralateral side. Nine patients (17.3%) had a longer limb and two patients (3.8%) had equal limb lengths (Fig. 2).
Fig. 2.
A bar chart shows the number of patients in relation to the measured LLD on a standing AP full-leg radiograph.
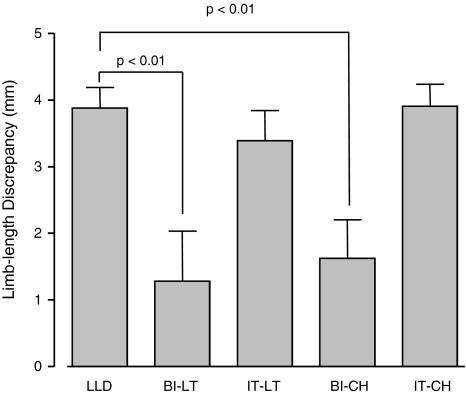
The mean difference between the true LLD and the LLD measured with landmarks on the pelvis was −2.6 mm for BI-IT (range, −11.5 to 10.8 mm), −2.3 mm for BI-CH (range, −10.4 to 8.8 mm), −0.5 mm for IT-LT (range, −5.8 to 4.5 mm), and 0.3 mm for IT-CH (range, −1.8 to 2.8 mm). Statistical analysis showed a difference (p < 0.01) when comparing the true LLD with BI-LT and BI-CH. No difference was found comparing the true LLD with the IT as a pelvic reference (IT-LT or IT-CH) regardless of the femoral reference (Fig. 3).
Fig. 3.
A bar chart shows the mean values for the different methods used to measure LLD. Whiskers indicate SD. LLD = LLD on AP full-leg radiograph; CH = center of the femoral head; LT = tip of the lesser trochanter; BI = biischial line; IT = interteardrop line.
There was almost perfect agreement for all intraobserver measurements (kappa = 0.84–0.93). Almost perfect agreement was found for all measurements performed with the CH as a femoral landmark (kappa = 0.85–0.87). Only substantial agreement was found when the LT was used as a femoral landmark (kappa = 0.66–0.70) (Table 2).
Table 2.
Reproducibility of measurements
| Error | BI-LT | IT-LT | BI-CH | IT-CH |
|---|---|---|---|---|
| Intraobserver | 0.84 | 0.86 | 0.93 | 0.91 |
| Interobserver | 0.70 | 0.66 | 0.85 | 0.87 |
IT = interteardrop line; BI = biischial line; LT = tip of the lesser trochanter; CH = center of the femoral head.
Discussion
Typical pathologic features of degenerative joint disease of the hip are progressive loss of cartilage and superior migration of the femoral head, which result in LLD. One of the intraoperative challenges in a THA is correcting a LLD without compromising hip stability [2, 37]. Preexisting LLDs should be accounted for during preoperative planning and should be corrected at the time of THA [4]. A common complication of THA is postoperative limb lengthening [11, 37, 38], which may be required to provide adequate stability [2]. Edeen et al. [11] reported a mean difference of 14.9 mm between the surgically treated and contralateral limbs, and 32% of their patients were aware of and dissatisfied with this problem. Although full-leg standing AP radiographs may provide a clear measurement of true LLD, they are not used frequently in daily practice. A standard AP view of the pelvis is used much more commonly to assess the preoperative LLD in THA [54]. This method has been reported to be as reliable as orthoroentgenograms [54] and reproducible, with a measurement error of ± 1 mm [53]. Review of the orthopaedic literature identifies different methods used to determine the LLD (Table 1). Our goal was to validate the different methods for LLD measurement on pelvic radiographs and evaluate their intraobserver and interobserver variability.
There are several limitations to this study. Functional limb length is the result of a complex interaction of the lengths of bones, implants, and soft tissue contractures. No single measure adequately conveys all of this information. The physical examination should include an assessment of spinal deformity and iliac crest symmetry. An abduction, adduction, or flexion contracture should be assessed and quantified because of the potential influence on perceived length. A flexion contracture can lead to overestimating shortening. Common causes of a perceived long limb include scoliosis, fixed pelvic tilt, and contralateral limb deformity [8]. In our study, patients with a spinal deformity and soft tissue contractures were excluded.
Preoperative measurement of a LLD alone will not lead to accurate restoration of the limb length after THA. The surgeon must use this information to determine the femoral osteotomy level. Various methods of measuring limb length change during surgery include comparing the dimensions of the resected bone with the dimensions replaced by the prosthesis [12, 57, 58], comparing the distance between the center of the trial head and the lesser trochanter [30, 43], the use of mechanical jigs and measuring calipers [6, 22, 37, 44], or the use of reference pins driven into the pelvis [3, 21, 31]. Some surgeons advocate the use of computer-assisted methods [33, 41, 55]. We did not compare preoperative and postoperative LLDs.
There is no consensus in the literature regarding what constitutes a significant LLD after THA [1, 35]. Some authors recommend the surgically treated limb length should be within 10 mm of the contralateral limb because this does not affect the functional parameters of gait [40] and produces a satisfactory result in most patients [2, 57]. One study [53] in the orthopaedic literature suggests a LLD has no effect on the functional outcome of THA, but many surgeons perceive it as an important problem to avoid [6, 12, 22, 24, 29, 58]. A shoe lift may not always be well accepted as an alternative [52]. Many patients are annoyed by a LLD, and patient education is important in preventing dissatisfaction. Although a small LLD may not be noticed by the patient, proper preoperative planning based on reliable measurements is very important to avoid it as much as possible.
Our data show the use of the biischial line as a pelvic landmark should be discouraged and the interteardrop line is a better alternative with measurements to the center of the femoral head or lesser trochanter that correlate well with the true LLD. There was no difference when using either the lesser trochanter or the center of the femoral head as a femoral landmark. Intraobserver variability testing showed less agreement when the lesser trochanter was used as a pelvic landmark compared with the center of the femoral head.
LLD measurement was more accurate with the interteardrop line as a pelvic landmark instead of the ischial tuberosity because the teardrop has been described as a more consistent landmark less influenced by the position of the pelvis [16, 58]. In patients with developmental dysplasia of the hip, the teardrop can be difficult to identify on an AP pelvic radiograph. With the use of a digital templating system, the center of the femoral head was easily identified using concentric circles. In patients with marked femoral head deformity, the center of the head can be more difficult to define. The shape, thickness, and therefore proximal and distal intersection of the lesser trochanter and the femoral cortex on a standard radiograph are subject to variation owing to femoral rotation [18]. We used the most medial part of the lesser trochanter as a femoral reference. Although the lesser trochanter is used most frequently as the femoral landmark (Table 1), it is not clearly demarcated and could be the subject of interobserver error as observed with the less accurate interobserver agreement.
The surgeon should not rely on templating alone but also use intraoperative testing and/or measurement and preoperative assessment of LLDs. When using preoperative templating to assess for LLDs, we recommend using the interteardrop line and center of the femoral head. This would lead to the most accurate measurement of a LLD compared with the true LLD measured on standing AP full-leg radiographs.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abraham WD, Dimon JH., 3rd Leg length discrepancy in total hip arthroplasty. Orthop Clin North Am. 1992;23:201–209. [PubMed] [Google Scholar]
- 2.Austin MS, Hozack WJ, Sharkey PF, Rothman RH. Stability and leg length equality in total hip arthroplasty. J Arthroplasty. 2003;18(3 suppl 1):88–90. doi: 10.1054/arth.2003.50073. [DOI] [PubMed] [Google Scholar]
- 3.Bal BS. A technique for comparison of leg lengths during total hip replacement. Am J Orthop (Belle Mead NJ) 1996;25:61–62. [PubMed] [Google Scholar]
- 4.Blackley HR, Howell GE, Rorabeck CH. Planning and management of the difficult primary hip replacement: preoperative planning and technical considerations. Instr Course Lect. 2000;49:3–11. [PubMed] [Google Scholar]
- 5.Bono JV. Digital templating in total hip arthroplasty. J Bone Joint Surg Am. 2004;86(suppl 2):118–122. doi: 10.2106/00004623-200412002-00016. [DOI] [PubMed] [Google Scholar]
- 6.Bose WJ. Accurate limb-length equalization during total hip arthroplasty. Orthopedics. 2000;23:433–436. [PubMed] [Google Scholar]
- 7.Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty. 2002;17(4 suppl 1):17–22. doi: 10.1054/arth.2002.33263. [DOI] [PubMed] [Google Scholar]
- 8.Clark CR, Huddleston HD, Schoch EP, 3rd, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:38–45. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Cummings G, Scholz JP, Barnes K. The effect of imposed leg length difference on pelvic bone symmetry. Spine (Phila Pa 1976). 1993;18:368–373. doi: 10.1097/00007632-199303000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Dolhain P, Tsigaras H, Bourne RB, Rorabeck CH, Mac Donald S, Mc Calden R. The effectiveness of dual offset stems in restoring offset during total hip replacement. Acta Orthop Belg. 2002;68:490–499. [PubMed] [Google Scholar]
- 11.Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ) 1995;24:347–351. [PubMed] [Google Scholar]
- 12.Eggli S, Pisan M, Müller ME. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br. 1998;80:382–390. doi: 10.1302/0301-620X.80B3.7764. [DOI] [PubMed] [Google Scholar]
- 13.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine (Phila Pa 1976). 1983;8:643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Giles LG, Taylor JR. Low-back pain associated with leg length inequality. Spine (Phila Pa 1976). 1981;6:510–521. doi: 10.1097/00007632-198109000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez Della Valle A, Slullitel G, Piccaluga F, Salvati EA. The precision and usefulness of preoperative planning for cemented and hybrid total hip arthroplasty. J Arthroplasty. 2005;20:51–58. doi: 10.1016/j.arth.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 16.Goodman SB, Adler SJ, Fyhrie DP, Schurman DJ. The acetabular teardrop and its relevance to acetabular migration. Clin Orthop Relat Res. 1988;236:199–204. [PubMed] [Google Scholar]
- 17.Gurney B, Mermier C, Robergs R, Gibson A, Rivero D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J Bone Joint Surg Am. 2001;83:907–915. doi: 10.2106/00004623-200106000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Hananouchi T, Sugano N, Nakamura N, Nishii T, Miki H, Yamamura M, Yoshikawa H. Preoperative templating of femoral components on plain X-rays: rotational evaluation with synthetic X-rays on ORTHODOC. Arch Orthop Trauma Surg. 2007;127:381–385. doi: 10.1007/s00402-007-0349-0. [DOI] [PubMed] [Google Scholar]
- 19.Hofmann AA, Skrzynski MC. Leg-length inequality and nerve palsy in total hip arthroplasty: a lawyer awaits! Orthopedics. 2000;23:943–944. doi: 10.3928/0147-7447-20000901-20. [DOI] [PubMed] [Google Scholar]
- 20.Hoikka V, Santavirta S, Eskola A, Paavilainen T, Wirta J, Lindholm TS. Methodology for restoring functional leg length in revision total hip arthroplasty. J Arthroplasty. 1991;6:189–193. doi: 10.1016/S0883-5403(06)80163-4. [DOI] [PubMed] [Google Scholar]
- 21.Huddleston HD. An accurate method for measuring leg length and hip offset in hip arthroplasty. Orthopedics. 1997;20:331–332. doi: 10.3928/0147-7447-19970401-10. [DOI] [PubMed] [Google Scholar]
- 22.Jasty M, Webster W, Harris W. Management of limb length inequality during total hip replacement. Clin Orthop Relat Res. 1996;333:165–171. doi: 10.1097/00003086-199612000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Khanduja V, Tek V, Scott G. The effect of a neck-retaining femoral implant on leg-length inequality following total hip arthroplasty: a radiological study. J Bone Joint Surg Br. 2006;88:712–715. doi: 10.1302/0301-620X.88B6.17190. [DOI] [PubMed] [Google Scholar]
- 24.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87:155–157. doi: 10.1302/0301-620X.87B2.14878. [DOI] [PubMed] [Google Scholar]
- 25.Krishnan SP, Carrington RW, Mohiyaddin S, Garlick N. Common misconceptions of normal hip joint relations on pelvic radiographs. J Arthroplasty. 2006;21:409–412. doi: 10.1016/j.arth.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 26.Lai KA, Lin CJ, Jou IM, Su FC. Gait analysis after total hip arthroplasty with leg-length equalization in women with unilateral congenital complete dislocation of the hip: comparison with untreated patients. J Orthop Res. 2001;19:1147–1152. doi: 10.1016/S0736-0266(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 27.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 28.Machen MS, Stevens PM. Should full-length standing anteroposterior radiographs replace the scanogram for measurement of limb length discrepancy? J Pediatr Orthop B. 2005;14:30–37. doi: 10.1097/01202412-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Maloney WJ, Keeney JA. Leg length discrepancy after total hip arthroplasty. J Arthroplasty. 2004;19(4 suppl 1):108–110. doi: 10.1016/j.arth.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Matsuda K, Nakamura S, Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006;77:375–379. doi: 10.1080/17453670610046280. [DOI] [PubMed] [Google Scholar]
- 31.McGee HM, Scott JH. A simple method of obtaining equal leg length in total hip arthroplasty. Clin Orthop Relat Res. 1985;194:269–270. [PubMed] [Google Scholar]
- 32.Mihalko WM, Phillips MJ, Krackow KA. Acute sciatic and femoral neuritis following total hip arthroplasty: a case report. J Bone Joint Surg Am. 2001;83:589–592. doi: 10.2106/00004623-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Murphy SB, Ecker TM. Evaluation of a new leg length measurement algorithm in hip arthroplasty. Clin Orthop Relat Res. 2007;463:85–89. doi: 10.1097/BLO.0b013e318126c08f. [DOI] [PubMed] [Google Scholar]
- 34.Nercessian OA, Piccoluga F, Eftekhar NS. Postoperative sciatic and femoral nerve palsy with reference to leg lengthening and medialization/lateralization of the hip joint following total hip arthroplasty. Clin Orthop Relat Res. 1994;304:165–171. [PubMed] [Google Scholar]
- 35.Parvizi J, Sharkey PF, Bissett GA, Rothman RH, Hozack WJ. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2310–2317. doi: 10.2106/00004623-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Ranawat CS. The pants too short, the leg too long! Orthopedics. 1999;22:845–846. doi: 10.3928/0147-7447-19990901-16. [DOI] [PubMed] [Google Scholar]
- 37.Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16:715–720. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 38.Ranawat CS, Rodriguez JA. Functional leg-length inequality following total hip arthroplasty. J Arthroplasty. 1997;12:359–364. doi: 10.1016/S0883-5403(97)90190-X. [DOI] [PubMed] [Google Scholar]
- 39.Rand JA, Ilstrup DM. Comparison of Charnley and T-28 total hip arthroplasty. Clin Orthop Relat Res. 1983;180:201–205. [PubMed] [Google Scholar]
- 40.Rösler J, Perka C. The effect of anatomical positional relationships on kinetic parameters after total hip replacement. Int Orthop. 2000;24:23–27. doi: 10.1007/s002640050006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarin VK, Pratt WR, Bradley GW. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplasty. 2005;20:887–891. doi: 10.1016/j.arth.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 42.Sathappan SS, Ginat D, Patel V, Walsh M, Jaffe WL, Di Cesare PE. Effect of anesthesia type on limb length discrepancy after total hip arthroplasty. J Arthroplasty. 2008;23:203–209. doi: 10.1016/j.arth.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 43.Schmalzried TP. Preoperative templating and biomechanics in total hip arthroplasty. Orthopedics. 2005;28(8 suppl):s849–851. doi: 10.3928/0147-7447-20050802-09. [DOI] [PubMed] [Google Scholar]
- 44.Shiramizu K, Naito M, Shitama T, Nakamura Y, Shitama H. L-shaped caliper for limb length measurement during total hip arthroplasty. J Bone Joint Surg Br. 2004;86:966–969. doi: 10.1302/0301-620X.86B7.14587. [DOI] [PubMed] [Google Scholar]
- 45.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 46.Stone RG, Weeks LE, Hajdu M, Stinchfield FE. Evaluation of sciatic nerve compromise during total hip arthroplasty. Clin Orthop Relat Res. 1985;201:26–31. [PubMed] [Google Scholar]
- 47.Suh KT, Cheon SJ, Kim DW. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop Scand. 2004;75:40–44. doi: 10.1080/00016470410001708070. [DOI] [PubMed] [Google Scholar]
- 48.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 49.Unnanuntana A, Wagner D, Goodman SB. The accuracy of preoperative templating in cementless total hip arthroplasty. J Arthroplasty. 2009;24:180–186. doi: 10.1016/j.arth.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 50.Weber ER, Daube JR, Coventry MB. Peripheral neuropathies associated with total hip arthroplasty. J Bone Joint Surg Am. 1976;58:66–69. [PubMed] [Google Scholar]
- 51.Wedemeyer C, Quitmann H, Xu J, Heep H, Knoch M, Saxler G. Digital templating in total hip arthroplasty with the Mayo stem. Arch Orthop Trauma Surg. 2008;128:1023–1029. doi: 10.1007/s00402-007-0494-5. [DOI] [PubMed] [Google Scholar]
- 52.White AB. AAOS Committee on Professional Liability: Study of 119 closed malpractice claims involving hip replacement. AAOS Bulletin. July 1994.
- 53.White TO, Dougall TW. Arthroplasty of the hip: leg length is not important. J Bone Joint Surg Br. 2002;84:335–338. doi: 10.1302/0301-620X.84B3.12460. [DOI] [PubMed] [Google Scholar]
- 54.Williamson JA, Reckling FW. Limb length discrepancy and related problems following total hip joint replacement. Clin Orthop Relat Res. 1978;134:135–138. [PubMed] [Google Scholar]
- 55.Wixson RL, MacDonald MA. Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation. J Arthroplasty. 2005;20(7 suppl 3):51–56. doi: 10.1016/j.arth.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 56.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 57.Woolson ST. Leg length equalization during total hip replacement. Orthopedics. 1990;13:17–21. doi: 10.3928/0147-7447-19900101-05. [DOI] [PubMed] [Google Scholar]
- 58.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14:159–164. doi: 10.1016/S0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]